What Are Telomeres And Why Do We Care?
Author: Dr. Stephen Chaney
 Ponce de Leon landed in Florida to search for the mythical “Fountain of Youth” in 1513. He never found it, but people have been searching for the Fountain of Youth ever since.
Ponce de Leon landed in Florida to search for the mythical “Fountain of Youth” in 1513. He never found it, but people have been searching for the Fountain of Youth ever since.
The more recent searches for the Fountain of Youth have involved potions and pills that promised to turn back the years. None of them worked either.
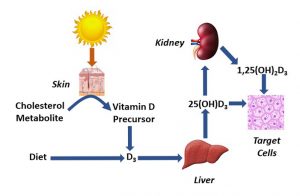
So, when I saw recent headlines proclaiming that vitamin D supplementation could reduce our biological age, I was skeptical. But then I read further, and discovered that the proposed mechanism involved slowing the rate of telomere shortening, I decided it was worth investigating the study (H Zhu et al, The American Journal of Clinical Nutrition, in press, May 5, 2025) behind the headlines.
But before I discuss the study, I should probably share another Biochemistry 101 nugget – “What are telomeres and why do we care?” (Once a professor, always a professor!)
What Are Telomeres And Why Do We Care?
- The genetic information that controls every cell in our body is stored in our DNA.
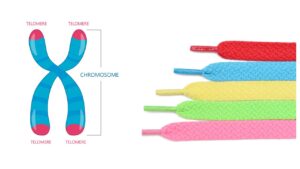
- DNA exists as a double-stranded helix that is organized into discrete chromosomes.
-
- If you had the pleasure of taking a biology class, you also know that the genetic information in DNA is transcribed into RNA molecules and is translated into cellular proteins. But you don’t need to know that information for this article.
It is an amazing system, but it has an Achilles heel.
- Our cells are full of enzymes called nucleases that can attach to the ends of chromosomes like little Pac Men and chew them up.
- And once these little Pac Men have chewed through essential genes, the chromosome becomes useless, and the cell dies.
Fortunately, there is a protective end on each chromosome called a telomere that is resistant to nucleases. You can think of it as analogous to the tip on the end of a shoelace (more about that analogy later).
 In more precise scientific terms, telomeres contain a very specific DNA sequence that causes them to loop back on themselves and form a quadruplex DNA structure (4 strands of DNA bound together) rather than the duplex (double helix) structure found throughout the rest of the chromosome. This makes telomeres resistant to nucleases, and each telomere contains multiple quadruplex structures.
In more precise scientific terms, telomeres contain a very specific DNA sequence that causes them to loop back on themselves and form a quadruplex DNA structure (4 strands of DNA bound together) rather than the duplex (double helix) structure found throughout the rest of the chromosome. This makes telomeres resistant to nucleases, and each telomere contains multiple quadruplex structures.
Unfortunately, nothing lasts forever – even telomeres.
- When we are young, our telomeres are long – between 2,000 and 10,000 nucleotides in length.
- But every time a cell divides, the telomeres get a little shorter.
-
- You can think of that like a biological clock – clicking off a few weeks or months of your life with each cell division.
- And for non-dividing cells, telomeres are also damaged by UV radiation and free radicals. This damage makes them sensitive to nucleases, which also shortens them.
Here is where the analogy with the tips on the end of shoelaces comes into play. If you’ve ever lost the tip at the end of a shoelace, you know the shoelace is worthless from then on.
It’s the same with our chromosomes:
- Once the telomere is gone, our chromosomes are susceptible to cellular nucleases and are rapidly degraded.
- When that happens, the cell dies because it no longer has genetic information to make essential proteins.
- And as more cells die our organs don’t work as well, our immune system weakens, and we become more susceptible to chronic diseases. We call this aging.
Previous studies have measured the average telomere length of people at various ages.
- If your telomeres are longer than average for your age, you are said to have a biological age that is less than your chronological age and vice versa.
This is a simplistic explanation of a complex process, but it provides you with enough information to understand the theory behind the current study.
How Was This Study Done?
 The investigators used a subset of the vitamin D data from a study called VITAL (Vitamin D and Omega-3 Trial). The VITAL study was a randomized, double-blind, placebo-controlled study (the gold standard of clinical studies) comparing the effect of supplementation with 2,000 IU/day of vitamin D versus a placebo.
The investigators used a subset of the vitamin D data from a study called VITAL (Vitamin D and Omega-3 Trial). The VITAL study was a randomized, double-blind, placebo-controlled study (the gold standard of clinical studies) comparing the effect of supplementation with 2,000 IU/day of vitamin D versus a placebo.
The study enrolled adults in their mid-fifties or older (average age = 65) with no previous history of cancer or cardiovascular disease and followed them for 5.3 years.
The participants filled out a yearly questionnaire to measure adherence to the study design. From these questionnaires the investigators reported that 80% of the participants in the VITAL study consumed at least two thirds of the capsules they were provided.
The original VITAL study was designed to look at the effect of vitamin D supplementation on cancer and cardiovascular disease. The “Cliffs Notes” version of the results are:
- Vitamin D reduced cancer deaths, but not the number of new cancer cases.
- Vitamin D did not have a significant effect on cardiovascular disease in this study.
The telomere study was based on a subset of 1054 participants in the VITAL study. These participants provided blood samples at the beginning of the study and at year 2 and year 4 for determination of telomere length.
Does Vitamin D Help You Live Longer?
- Telomeres shortened by 140 base pairs over the 4-year period in the control group receiving the placebo.
-
- The investigators estimated that this was equivalent to about 5 years of chronological age.
- In contrast, no significant shortening of telomeres was seen in the group receiving 2,000 IU/day of vitamin D.
The authors concluded, “In the VITAL telomere study, vitamin D3 supplementation reduced telomere attrition and preserved telomere length, supporting an anti-aging cellular effect of vitamin D…Future independent large-scale RCTs [randomized controlled trials] are warranted to replicate our findings…”
What Are The Strengths And Weaknesses Of This Study?
- This is the largest and longest study on the effect of vitamin D supplementation on telomere length publish to date.
- It is a randomized, double-blind, placebo-controlled trial – the gold standard for clinical trials.
- It is supported by several smaller studies that have come to the same conclusion.
It has a couple of weaknesses that actually strengthen the conclusions of the study.
- The investigators reported that only 80% of participants took two thirds or more of their vitamin D capsules. That makes the effective dose closer to 1,500 IU than 2,000 IU.
- The investigators did not measure blood levels of 1,25-dihydroxyvitamin D, the active form of vitamin D, and there is significant individual variation in our ability to convert supplemental vitamin D to 1,25-dihydroxyvitamin D.
-
- For example, we know that obesity and cholesterol medications interfere with our ability to convert vitamin D to 1,25-dihydroxyvitamin D.
-
- So, the investigators looked at participants who were obese or taking cholesterol medication and reported no effect of vitamin D on telomere shortening as expected. That suggests that the effect of vitamin D on telomere shortening might be even greater in individuals who were not obese and no taking cholesterol drugs.
Weaknesses:
- There is a lot we don’t know about telomeres and telomere shortening.
-
- For example, we don’t know why vitamin D affects telomere shortening. We have hypotheses. But none of them have been proven.
- Right now, all we have are associations.
-
- Telomere shortening is associated with aging. Does that mean we can increase our life span by preventing telomere shortening? We don’t know.
-
- Telomere shortening is associated with the onset of chronic diseases. Does that mean we can reduce our risk of chronic diseases by preventing telomere shortening? We don’t know.
What Does This Study Mean For You?
 At the beginning of this article I asked the question, “Does Vitamin D help you live longer?”
At the beginning of this article I asked the question, “Does Vitamin D help you live longer?”
- We know telomere shortening is associated with aging.
- The study I just reviewed shows that vitamin D supplementation significantly reduces telomere shortening.
Does that mean the answer to the question I posed is, “Yes”? Probably not. A more correct answer would be. “Maybe”.
The problem is that there are many causes of aging and there are many causes of chronic diseases. So, the question becomes, “Is telomere shortening…
- …The villain who pulls the trigger… (In this scenario, when your telomeres are gone, you are gone).
- …or an innocent bystander?” (In this scenario, it’s something else that pulls the trigger, and you die with your shortened telomeres intact).
We don’t know the answer to this question. But we do know that optimal vitamin D levels are important for:
- Healthy bones.
- A strong immune system.
- Neuromuscular health.
- Reduced risk of some chronic diseases.
If it also helps you live longer, count that as an unexpected benefit.
The Bottom Line
A recent study showed that vitamin D supplementation slowed the rate of telomere shortening, which may help you live longer.
For more information on this study, the relationship between telomere shortening and aging, and what this study means for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
_____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
___________________________________________________________________
About The Author
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading Biochemistry textbooks for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 53 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.