Does Genetics Influence Supplementation Benefits?
 The cause of type 1 diabetes is a mystery. If you go to an authoritarian source like the Mayo Clinic, you will discover that:
The cause of type 1 diabetes is a mystery. If you go to an authoritarian source like the Mayo Clinic, you will discover that:
- Type 1 diabetes is an autoimmune disease that selectively attacks the insulin-producing islet cells of the pancreas.
- Certain genetic variants predispose individuals to type 1 diabetes.
- The autoimmune response may be triggered by a viral infection or other unknown environmental factors in genetically susceptible individuals.
- The incidence of type 1 diabetes increases as you travel away from the equator, which suggests that vitamin D may be involved.
The idea that vitamin D may be involved is an important concept because it suggests that vitamin D supplementation might reduce the risk of developing type 1 diabetes. This idea was reinforced by a Finnish study (E Hyponnen et al, Lancet, 358: 1500-1503, 2001) published in 2001 showing the vitamin D supplementation of newborn infants reduced the incidence of type 1 diabetes at age 1.
However, subsequent studies in other parts of the world have had mixed results. Some have confirmed the results of the Finnish study. Others have come up empty.
Similarly, some studies have shown a correlation between low 25-hydroxyvitamin D levels in the blood and the development of type 1 diabetes in children, while other studies have found no correlation.
Why the discrepancy between studies? Some of the differences can be explained by differences in the populations studied or differences in study design. But what if there were another variable that none of the previous studies has considered?
The study (JM Norris et al, Diabetes, 67: 146-154, 2018) I review this week describes just such a variable. The authors of the study hypothesized that the association between 25-hydroxyvitamin D levels and the risk of developing type 1 diabetes is influenced by mutations that affect the way vitamin D works in the body. Previous studies have not taken these mutations into account. If the author’s hypothesis is true, it might explain why these studies have produced conflicting results.
In this article, I will answer 3 questions:
- Does vitamin D prevent type 1 diabetes?
- If so, is supplementation with vitamin D important?
- Who will benefit most from vitamin D supplementation?
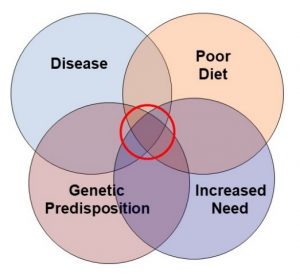
But, before I answer those questions, I should begin by providing some background. I will start by reviewing the how diet, increased need, disease, and genetics influence the likelihood that we will benefit from supplementation. Then I will review vitamin D metabolism.
Does Genetics Influence Supplementation Benefits?
 The reason so many studies find no benefit from supplementation is that they are asking the wrong question. They are asking “Does supplementation benefit everyone?” That is an unrealistic expectation.
The reason so many studies find no benefit from supplementation is that they are asking the wrong question. They are asking “Does supplementation benefit everyone?” That is an unrealistic expectation.
I have proposed a much more realistic model (shown on the left) for when we should expect supplementation to be beneficial. Simply put, we should ask:
- Is the diet inadequate with respect to the nutrient that is being studied?
- Is there an increased need for that nutrient because of age, gender, activity level, or environment?
- Is there a genetic mutation that affects the metabolism or need for that nutrient?
- Is there an underlying disease state that affects the need for that nutrient?
When clinical studies are designed without taking this paradigm into account, they are doomed to fail. Let me give you some specific examples.
- The Heart Outcomes Prevention Evaluation study concluded supplementation with folate and other B vitamins did not reduce heart disease risk. The problem was that 70% of the people in the study were getting adequate amounts of folate from their diet at the beginning of the study. For those individuals not getting enough folate in their diet, B vitamin supplementation decreased their risk of heart disease by 15%. This is an example of poor diet influencing the need for supplementation.
The other three examples come from studies on the effect of vitamin E supplementation on heart disease that I summarized in an article in “Health Tips From The Professor” a few years ago. Here is a brief synopsis.
- The Women’s Health Study concluded that vitamin E did not decrease heart disease risk in the general population. However, the study also found that in women over 65 (who are at high risk of heart disease), vitamin E supplementation decreased major cardiovascular events and cardiovascular deaths by 25%. This is an example of increased need because of age and gender influencing the need for supplementation.
- The Women’s Antioxidant Cardiovascular Study” concluded that vitamin E did not decrease heart disease risk in the general population. However, when they looked at women who already had cardiovascular disease at the beginning of the study, vitamin E supplementation decreased risk of heart attack, stroke, and cardiovascular death by 23%. This is an example of an underlying disease affecting the need for supplementation.
- The HOPE study concluded that vitamin E did not decrease heart disease risk in the general population. However, when they looked at individuals with a mutation that increases the risk of heart disease, vitamin E supplementation significantly decreased their risk of developing heart disease. This is an example of genetics affecting the need for supplementation.
These are just a few of many examples. When you ask whether supplementation benefits everyone, the answer is often no. However, when you look at people with inadequate diet, increased need, underlying disease, and/or genetic predisposition, the answer is often yes.
This background sets the stage for the current study. Of course, to understand the author’s hypothesis that mutations in genes involved in vitamin D metabolism might influence the effect of vitamin D on the risk of developing type 1 diabetes, you need to know a little about vitamin D metabolism.
Biochemistry 101: Vitamin D Metabolism
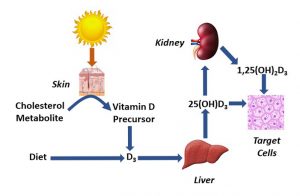 When sunlight strikes a metabolite of cholesterol in our skin, it is converted to a precursor that spontaneously isomerizes to form vitamin D3. Because this series of reactions is usually not sufficient to provide all the vitamin D3 our bodies require, we also need to get vitamin D3 from diet and supplementation.
When sunlight strikes a metabolite of cholesterol in our skin, it is converted to a precursor that spontaneously isomerizes to form vitamin D3. Because this series of reactions is usually not sufficient to provide all the vitamin D3 our bodies require, we also need to get vitamin D3 from diet and supplementation.
However, vitamin D3 is not active by itself. It first needs to be converted to 25-hydroxyvitamin D by our liver and then to the active 1,25-dihydroxyvitamin D. 1,25-dihydroxyvitamin D is an important hormone that regulates many cells in our body.
Some of the 1,25-dihydroxyvitamin D is synthesized by our kidneys and released into the bloodstream. This 1,25-dihyroxyvitamin D binds to vitamin D receptors on the surface of many cells and initiates regulatory pathways that affect metabolism inside the cell.
Other cells take up 25-hydroxyvitamin D and convert it to 1,25-dihydroxyvitamin D themselves. In these cells both the synthesis and regulatory effects of 1,25-dihydroxyvitamin D occur entirely inside the cell.
In both cases, it is 1,25-dihydroxyvitamin D that regulates cellular metabolism. The only difference is the way this regulation is accomplished.
There are two additional points that are relevant to this study.
- The efficiency of conversion of vitamin D to 25-hydroxyvitamin D varies from person to person.
-
- Thus, blood levels of 25-hydroxyvitamin D are considered a more reliable measure of vitamin D status than dietary intake of vitamin D or sun exposure.
-
- Blood levels of 25-hydroxyvitamin D levels ≥50 nmol/L are considered optimal, while levels of 30 to <50 nmol/L are considered suboptimal, and levels <30 nmol/L are considered deficient.
- 1,25-dihydroxyvitamin D binds to the vitamin D receptor on immune cells. This initiates a series of reactions that decrease the risk of autoimmune responses by our immune system.
How Was This Study Done?
 This study was called TEDDY (The Environmental Determinants Of Type 1 Diabetes in the Young). Between September 2004 and February 2010, 424,788 newborn infants from 6 medical centers in Colorado, Georgia, Washington, Finland, Germany, and Sweden were screened for genes that predispose to type 1 diabetes.
This study was called TEDDY (The Environmental Determinants Of Type 1 Diabetes in the Young). Between September 2004 and February 2010, 424,788 newborn infants from 6 medical centers in Colorado, Georgia, Washington, Finland, Germany, and Sweden were screened for genes that predispose to type 1 diabetes.
The investigators identified 21,589 high-risk infants, and 8,676 of them were enrolled in this study before age 4 months. Clinic visits for the children occurred every 3 months between 3 and 48 months of age and every 6 months thereafter.
- A DNA sample was taken at the time they entered the study and analyzed for mutations in genes involved in vitamin D metabolism.
- 25-hydroxy vitamin D levels were obtained at each office visit. Because some studies have suggested the vitamin D status during the first year of life is important, the data were analyzed in two ways.
-
- An average of all 25-hydroxyvitamin D levels (referred to as “childhood 25-hydroxyvitamin D levels”).
-
- An average of 25-hydroxyvitamin D levels during the first 12 months (referred to as “early infancy 25-hydroxyvitamin D levels”).
- Serum autoantibodies to pancreatic islet cells were measured at each office visit as a measure of an autoimmune attack on those cells. Persistent autoimmune response was defined as positive autoantibodies on two consecutive office visits.
While this study did not directly measure type 1 diabetes, children with an autoimmune response to their pancreatic islet cells are highly likely to develop type 1 diabetes. Thus, for purposes of simplicity I will refer to “risk of developing type 1 diabetes” rather than “persistent autoimmune response” in describing these results.
-
- 418 children developed persistent autoantibodies to their pancreatic islet cells during the study. The onset of this autoimmune response ranged from 2 months to 72 months with an average of 21 months.
-
- These children were compared to 3 matched controls from their medical center who did not develop an autoimmune response.
This study was remarkable for two reasons:
1) It was much larger than previous studies. This gave it greater power to detect an effect of vitamin D status on the risk of developing type 1 diabetes.
2) This was the first study to ask whether mutations in genes controlling the metabolism of vitamin D influenced the effect of vitamin D on the risk of developing type 1 diabetes.
Does Vitamin D Prevent Type 1 Diabetes?
 The study compared the risk of developing type 1 diabetes in children whose 25-hydroxyvitamin D levels were optimal (≥50 nmol/L) to children whose 25-hydroxyvitamin D levels were suboptimal (30 to <50 nmol/L). The results were:
The study compared the risk of developing type 1 diabetes in children whose 25-hydroxyvitamin D levels were optimal (≥50 nmol/L) to children whose 25-hydroxyvitamin D levels were suboptimal (30 to <50 nmol/L). The results were:
- Optimal vitamin D status during childhood was associated with a 31% decrease in the risk of developing type 1 diabetes.
- Optimal vitamin D status during early infancy (first 12 months) was associated with a 40% decrease in the risk of developing type 1 diabetes.
In other words, having optimal vitamin D status significantly reduces the likelihood of developing of type 1 diabetes in childhood.
- 25-hydroxyvitamin D levels >75 nmol/L provided no additional benefit.
In other words, you need sufficient vitamin D, but higher levels provide no additional benefit.
- They tested 5 genes involved in vitamin D metabolism to see if they influenced the effect of vitamin D on the risk of developing type 1 diabetes. Only the VDR (vitamin D receptor) gene had any influence.
-
- When the VDR gene was fully functional, optimal vitamin D status had no effect on the risk of developing type 1 diabetes. This means that even suboptimal (30 to <50 nmol/L) levels of 25-hydroxyvitamin D were sufficient to prevent type 1 diabetes when the vitamin D receptor was fully functional.
-
- Only 9% of the children in this study were vitamin D deficient (<30 nmol/L 25-hydroxyvitamin D). Presumably, these children would be at high risk of developing type 1 diabetes even with a fully functional VDR gene. However, there were not enough children in that category to test this hypothesis.
- When they looked at children with mutations in the VDR gene:
-
- Optimal vitamin D status during childhood was associated with a 59% decrease in the risk of developing type 1 diabetes.
-
- Optimal vitamin D status during early infancy (first 12 months) was associated with a 67% decrease in the risk of developing type 1 diabetes.
In short, the need for optimal vitamin D levels to reduce the risk of developing type 1 diabetes is only seen in children with a mutation in the VDR (vitamin D receptor) gene.
- This is a clear example of genetics affecting the need for a nutrient.
-
- For children with a fully functional VDR gene, even 30-50 nmol/L 25-hydroxyvitamin D was sufficient to reduce the risk of developing type 1 diabetes.
-
- However, children with mutations in the VDR gene required ≥50 nmol/L 25-hydroxyvitamin D to reduce their risk of developing type 1 diabetes.
- This is also an example of genetics affecting the need for supplementation with vitamin D.
-
- 42% of the children in this study had suboptimal levels of 25-hydroxyvitamin D. Those who also have a mutation in the VDR gene would require supplementation to bring their 25-hydroxyvitamin D up to the optimal level to reduce their risk of developing type 1 diabetes.
-
- Other studies have estimated that up to 61% of children in the US may have suboptimal 25-hydroxyvitamin D levels.
What Does This Study Mean For You?
 Let’s start with the three questions I proposed at the beginning of this article.
Let’s start with the three questions I proposed at the beginning of this article.
1) Does vitamin D prevent type 1 diabetes? Based on this study, the answer appears to be a clear yes. However, this is the first study of this kind. We need more studies that into account the effect of mutations in the VDR gene.
2) If so, is supplementation with vitamin D important? If we think in terms of supplementation with RDA levels of vitamin D or sufficient vitamin D to bring 25-hydroxyvitamin D into the optimal range, the answer is also a clear yes. However, there is no evidence from this study that higher doses of vitamin D provide additional benefits.
3) Who will benefit most from vitamin D supplementation? Based on this study, the children who will benefit the most from vitamin D supplementation are those who have a suboptimal vitamin D status and have a mutation in the VDR (vitamin D receptor) gene. To put this into perspective:
-
- Up to 60% of children and adults in this country have suboptimal vitamin D levels.
-
- The percentage of suboptimal vitamin D levels is highest for people who are obese, have pigmented skin, are institutionalized (eg, elderly in nursing homes), and/or live far from the equator.
-
- Supplementation with a multivitamin containing the RDA for vitamin D reduces the risk of having suboptimal vitamin D status by 2.5 to 5-fold depending on the person’s ethnicity.
-
- This study may be just the tip of the iceberg. The vitamin D receptor is also found on many other cells that control important biological functions.
Finally, if you are a parent or parent-to-be, you probably have several questions. Here are the ones I have  anticipated:
anticipated:
#1: Is my child at risk for developing type 1 diabetes? If you or a close family member has type 1 diabetes, you can assume your child is genetically predisposed to developing type 1 diabetes. Other factors that increase your child’s risk of developing type 1 diabetes are obesity, non-White ethnicity, and geographical location far from the equator.
#2: Should I have my baby tested for genetic predisposition to type 1 diabetes? That is not currently recommended. Just be aware of the risk factors listed above.
#3: Should I have my baby tested for VDR mutations? That is unnecessary. If your child has a VDR mutation, they just need sufficient vitamin D, not mega doses of vitamin D. And there are lots of other reasons for making sure your child gets sufficient vitamin D.
#4: How much vitamin D should my child be getting? The recommendation is 400 IU up to age 1 and 600 IU over age 1.
#5: Should I give my child vitamin D supplements? It is a good idea. For children over age 1, I recommend a multivitamin supplying 600 IU of vitamin D.
For infants, the American Association of Pediatrics recommends 400 IU vitamin D drops, regardless of whether the infants are breast or formula fed. That is because studies during the first year of life show that less than one-fifth of all infants get the recommended 400 IU/d from any source, and fewer than one out of 10 breast-fed infants meet the requirement – even if the mother is getting adequate vitamin D in their diet.
One Caution: I do not recommend exceeding 400 IU for infants or 600 IU for children unless directed by your health care provider. In terms of the risk of developing type 1 diabetes, your child needs sufficient vitamin D, and more is not better.
#6: Should I have my child tested for 25-hydroxyvitamin D levels? That is not done routinely at the present time. However, if your child has one or more of the risk factors listed above, it is a conversation you should have with your health care provider.
The Bottom Line
While it is widely accepted that vitamin D helps reduce the risk of developing type 1 diabetes in childhood, that has been difficult to prove. Clinical studies have provided conflicting results. The authors of a recent study postulated that the discrepancies between studies may have arisen because the studies neglected the effect of mutations in genes controlling vitamin D metabolism which may affect the ability of vitamin D to reduce the risk of developing type 1 diabetes.
This study found that:
1) Infants and children with optimal vitamin D status (25-hydroxyvitamin D levels ≥50 nmol/L) were 31-40% less likely to develop type 1 diabetes than children with suboptimal vitamin D status (25-hydroxyvitamin D = 30 to <50 nmol/L).
2) However, the effect of vitamin D on the risk of developing type 1 diabetes was only seen in children with one or more mutations in the VDR (vitamin D receptor) gene. To interpret this observation, you need to know that:
-
- Type 1 diabetes is caused by an autoimmune attack on the pancreatic islet cells that release insulin.
-
- 1,25-dihydroxyvitamin D promotes immune tolerance and decreases the risk of autoimmune responses.
-
- 1,25-dihydroxyvitamin D exerts this effect by binding to the vitamin D receptor on the surface of immune cells.
3) Thus, mutations in the VDR gene modify the effect of vitamin D on the risk of developing type 1 diabetes. Specifically:
-
- When the VDR gene is fully active, even suboptimal levels of vitamin D appear to be sufficient to prevent the development of type 1 diabetes in childhood.
-
- However, when the VDR gene has mutations that reduce its activity, suboptimal levels of vitamin D no longer prevent type 1 diabetes. Optimal levels of vitamin D are required to reduce the risk of developing type 1 diabetes.
This is an example of genetics increasing the need for a nutrient (vitamin D) and increasing the need for supplementation to make sure that optimal levels of that nutrient are achieved.
While this study focused on the effect of vitamin D on the development of type 1 diabetes, this may just be the tip of the iceberg. The vitamin D receptor is also found on many other cells that control important biological functions.
For more details, read the article above. You will probably want to read the section “What Does This Mean For You?”, including my recommendations for parents of young children
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.