Nutrition Advances Over The Last Two Years
Author: Dr. Stephen Chaney
 In the nearly twelve years that I have been publishing “Health Tips From The Professor”, I have tried to go behind the headlines to provide you with accurate, unbiased health information that you can trust and apply to your everyday life.
In the nearly twelve years that I have been publishing “Health Tips From The Professor”, I have tried to go behind the headlines to provide you with accurate, unbiased health information that you can trust and apply to your everyday life.
The 600th issue of any publication is a major cause for celebration and reflection – and “Health Tips From The Professor” is no different.
I am dedicating this issue to reviewing some of the major stories I have covered in the past 100 issues. There are lots of topics I could have covered, but I have chosen to focus on three types of articles:
- Articles that have debunked long-standing myths about nutrition and health.
- Articles that have corrected some of the misinformation that seems to show up on the internet on an almost daily basis.
- Articles about the issues that most directly affect your health.
Here are my picks from the last two years:
Weight Loss Diets
 Since it is almost January, let’s start with a couple of articles about diet and weight loss (or weight gain). I have covered the effectiveness of the Paleo, Keto, Mediterranean, DASH, vegetarian, and Vegan diets for both short and long-term weight loss in my book “Slaying The Food Myths”, so I won’t repeat that information here. Instead, I will share a few updates from the past 100 issues.
Since it is almost January, let’s start with a couple of articles about diet and weight loss (or weight gain). I have covered the effectiveness of the Paleo, Keto, Mediterranean, DASH, vegetarian, and Vegan diets for both short and long-term weight loss in my book “Slaying The Food Myths”, so I won’t repeat that information here. Instead, I will share a few updates from the past 100 issues.
Is Time-Restricted Eating Better Than Other Diets? Time-restricted eating is one of the latest fads. But is it really better than other diets for weight loss and improved health? In this article I reviewed two studies that compare time-restricted eating with diets that do not restrict time of eating but cut calories to the same extent. You may be surprised at the results.
Can You Lose Weight Without Dieting? In this article I share 8 tips for losing weight without going on a diet. The article is based on research by Dr. Brian Wansink, a behavioral psychologist who specializes in studying how external clues influence our eating patterns. As you might suspect his 8 tips for losing weight have nothing to do with counting calories or going on restrictive diets.
Healthy Diets
 Is Whole Fat Dairy Healthy? For years dietary guidelines have been telling us to select low fat dairy foods. But some health gurus are telling you that isn’t true. They claim whole fat dairy is healthy. So, you are probably wondering, “What is the scoop (as in ice cream) on whole fat dairy?” In this article I look at the study behind the headlines and answer that question. But the answer is not a simple “Yes” or “No”. The answer is more nuanced. It turns out that whole fat dairy is healthier in some diets than in others.
Is Whole Fat Dairy Healthy? For years dietary guidelines have been telling us to select low fat dairy foods. But some health gurus are telling you that isn’t true. They claim whole fat dairy is healthy. So, you are probably wondering, “What is the scoop (as in ice cream) on whole fat dairy?” In this article I look at the study behind the headlines and answer that question. But the answer is not a simple “Yes” or “No”. The answer is more nuanced. It turns out that whole fat dairy is healthier in some diets than in others.
Are Low Carb Diets Healthy? Are low carb diets good for you or bad for you? It depends on which study you quote. Two major studies in recent years have come to opposite conclusions. In this article I help you sort through the conflicting studies and rephrase the question. Instead of, “Are low carb diets healthy”, the question should be, “Which low carb diets are healthy?”
Are All Plant-Based Diets Healthy? Plant-based diets have acquired a “health halo” in recent years. Your mama told you to eat your fruits and vegetables. And many health gurus have been telling you not to neglect your grains, legumes, nuts, and seeds as well. But some of these foods require a lot of food preparation.
Never fear! The food industry has come to your rescue with a wide variety of processed plant-based foods. No need for food prep. But are they as good for you as the unprocessed plant foods they replace? In this article I review a study that answers that question.
You probably know what that answer is, but the article is worth a read anyway. That is because the study also asks whether vegan and vegetarian diets are healthier than other primarily plant-based diets. And you may not know the answer to that question.
Diet And Heart Disease
 Are Eggs Bad For You? For years we were told that eggs are bad for us because they contain cholesterol. Then we were told that eggs in moderation may not increase our risk of heart disease. And recently studies have appeared claiming eggs may be good for our hearts. What is the truth about eggs and heart disease? In this article I review a recent study claiming eggs are bad for our heart and put that study into the context of other recent studies to clear up the “eggfusion”.
Are Eggs Bad For You? For years we were told that eggs are bad for us because they contain cholesterol. Then we were told that eggs in moderation may not increase our risk of heart disease. And recently studies have appeared claiming eggs may be good for our hearts. What is the truth about eggs and heart disease? In this article I review a recent study claiming eggs are bad for our heart and put that study into the context of other recent studies to clear up the “eggfusion”.
Which Diets Are Heart Healthy? Every popular diet claims to help you lose weight, reduce your risk of diabetes, and reduce your risk of heart disease. All these claims can’t be true. Which diets deliver on their promises, and which are just pretenders? In this article I review a recent study that answered that question for heart disease.
This study was a very large metanalysis of over 40 studies with 35,548 participants that looked at the effect of different diets on heart disease outcomes. The study identified two diets that significantly reduced the risk of heart disease. There are other diets that might reduce the risk of heart disease, but their benefits have not been proven by high quality clinical studies. They are merely pretenders.
The Dangers Of Processed Foods
 In previous issues of “Health Tips From the Professor” I have shared articles showing that diets high in processed foods are associated with an increased risk of obesity, diabetes, and heart disease. But the story keeps getting worse. Here are two articles on recent studies about processed foods that appeared in “Health Tips From The Professor” in the last two years.
In previous issues of “Health Tips From the Professor” I have shared articles showing that diets high in processed foods are associated with an increased risk of obesity, diabetes, and heart disease. But the story keeps getting worse. Here are two articles on recent studies about processed foods that appeared in “Health Tips From The Professor” in the last two years.
Why Does Processed Food Make You Fat? We already know that eating a lot of highly processed food is likely to make us fat. But what is it about processed food that makes us fat? In this article I review a recent study that answers that question.
This study is interesting for two reasons.
- It identifies the characteristics of processed foods that make us want to eat more.
- It identifies some minimally processed foods that have the same characteristics and suggests we should choose minimally processed foods wisely. Simply put, knowledge is power. We may want to avoid minimally processed foods that have the same obesity-inducing characteristics as processed foods.
Do Processed Foods Cause Cancer? Previous studies have shown that processed food consumption is associated with a higher risk of obesity, diabetes, and heart disease. Can it get any worse? In this article I review a recent study that shows processed food consumption is associated with an increased risk of several kinds of cancer.
Maintaining Muscle Mass As We Age
 As we age, we begin to lose muscle mass, a process called sarcopenia. Unless we actively resist loss of muscle mass it will eventually impact our quality of life and our health.
As we age, we begin to lose muscle mass, a process called sarcopenia. Unless we actively resist loss of muscle mass it will eventually impact our quality of life and our health.
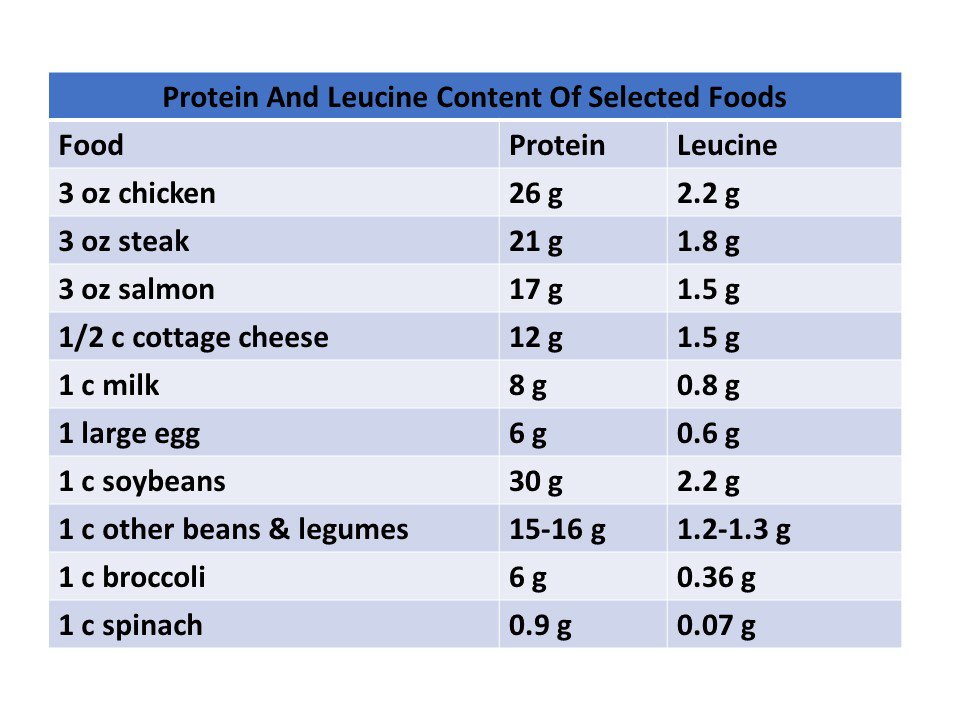
We can prevent this loss of muscle mass with resistance exercise, adequate protein intake, and adequate intake of the amino acid leucine. Previous studies have shown people over 50 need more of each of these to maintain muscle mass, but the amount they need has been uncertain until now. Three recent studies have given seniors better guidelines for maintaining muscle mass.
Can You Build Muscle In Your 80s? In this article I review a recent study that enrolled a group of octogenarians in a high-intensity exercise program to see if they could gain muscle mass. They were able to increase their muscle mass, but the intensity of the exercise required may surprise you.
Optimizing Protein Intake For Seniors. In this article I review two recent studies that looked at the amount, timing, and kind of protein needed for seniors in their 60s and 70s to maximize gain in muscle mass.
How Much Leucine Do Seniors Need? In this article I review a recent study that determined the amount of leucine seniors in their 70s need to optimize gains in muscle mass and strength.
The Benefits And Risks Of Supplementation
 If you listen to Big Pharma or the medical profession, you hear a lot about the “risks” of supplementation and very little about the benefits. In “Health Tips From the Professor” I try to present a more balanced view of supplementation by sharing high-quality studies showing benefit from supplementation and studies that put the supposed risks into perspective.
If you listen to Big Pharma or the medical profession, you hear a lot about the “risks” of supplementation and very little about the benefits. In “Health Tips From the Professor” I try to present a more balanced view of supplementation by sharing high-quality studies showing benefit from supplementation and studies that put the supposed risks into perspective.
The Good News About Omega-3s and Stroke. Multiple studies have shown that omega-3 supplementation reduces the risk of ischemic strokes (strokes caused by a blood clot). But it has been widely assumed they might increase the risk of hemorrhagic strokes (strokes caused by bleeding). In this article I review a meta-analysis of 29 clinical studies with 183,000 participants that tested that assumption.
How Much Omega-3s Are Best For Blood Pressure? Multiple studies have shown that omega-3 supplementation can reduce high blood pressure. But the doses used vary widely from one study to the next. In this article I review a meta-analysis of 71 double-blind, placebo-controlled clinical studies that determined the optimal dose of omega-3s for controlling blood pressure.
Omega-3 Supplements Are Safe. As I said above, it has been widely assumed that omega-3 supplementation increases the risk of bleeding and hemorrhagic stroke. In this article I review the definitive study on this topic. More importantly, it reveals which omega-3 supplements might increase bleeding risk and which do not.
Are Calcium Supplements Safe? Big Pharma and the medical profession have been warning us that calcium supplements may increase heart disease risk. In this article I review the definitive study on this topic.
Prenatal Supplements
 If you are pregnant or thinking of becoming pregnant, your health professional has likely recommended a prenatal supplement. You probably assume that prenatal supplements provide everything you need for a healthy pregnancy. Unfortunately, recent research has shown that assumption is not correct.
If you are pregnant or thinking of becoming pregnant, your health professional has likely recommended a prenatal supplement. You probably assume that prenatal supplements provide everything you need for a healthy pregnancy. Unfortunately, recent research has shown that assumption is not correct.
Is Your Prenatal Supplement Adequate? In this article I review a study that should serve as a wakeup call for every expectant mother. It showed that most prenatal supplements were woefully inadequate for a healthy pregnancy.
What Nutrients Are Missing In Prenatal Supplements? In this article I review a study that identified additional nutrients that are missing in most prenatal supplements.
Prenatal Supplements Strike Out Again. In this article I review a study that looked at the diet of pregnant women to determine their needs and compared that to the nutrients found in prenatal supplements. Once again, most prenatal supplements were woefully inadequate. Is it, “Three strikes and you are out”?
Exercise
 Walking Your Way To Health. We have been told that walking is good for our health. But how many steps should you take, how fast should you walk, and does it matter whether these steps are part of your daily routine or on long hikes? In this article I review a study that answers all these questions.
Walking Your Way To Health. We have been told that walking is good for our health. But how many steps should you take, how fast should you walk, and does it matter whether these steps are part of your daily routine or on long hikes? In this article I review a study that answers all these questions.
Which Exercise Is Best For Reducing Blood Pressure? If you have high blood pressure, you have probably been told to exercise more. But which exercise is best? In this article I review a study that answers that question. And the answer may surprise you.
Did You Know?
 If you have been reading “Health Tips From the Professor” for a while, you probably know that I enjoy poking holes in popular myths. Here are two new ones I deflated in past two years.
If you have been reading “Health Tips From the Professor” for a while, you probably know that I enjoy poking holes in popular myths. Here are two new ones I deflated in past two years.
Is Low Alcohol Consumption Healthy? You have probably heard that low alcohol intake (that proverbial glass of red wine) is good for you. But is that true? In this article I review a recent study that shows that myth was based on faulty interpretation of the data and provides a more nuanced interpretation of the data.
Is HDL Good For Your Heart? You have been told that increasing your HDL levels reduces your risk of heart disease so many times it must be true. But is it? In this article I review HDL metabolism and a recent study to provide a more nuanced interpretation of the relationship between HDL and heart disease risk.
How To Talk With Your Doctor About Cancer
Because of my years in cancer research, I am often asked whether someone should follow their oncologist’s advice and go on a recommended chemotherapy or radiation regimen. Of course, it would be unethical for me to provide that kind of advice.
In this article I tell you the questions to ask your oncologist about the prescribed treatment regimen, so you can make an informed decision. However, I also recommend you only ask these questions if you can handle the answers.
The Bottom Line
I have just touched on a few of my most popular articles above. You may want to scroll through these articles to find ones of interest to you that you might have missed over the last two years. If you don’t see topics that you are looking for, just go to https://chaneyhealth.com/healthtips/ and type the appropriate term in the search box.
In the coming years, you can look for more articles debunking myths, exposing lies and providing balance to the debate about the health topics that affect you directly. As always, I pledge to provide you with scientifically accurate, balanced information that you can trust. I will continue to do my best to present this information in a clear and concise manner so that you can understand it and apply it to your life.
Final Comment: You may wish to share the valuable resources in this article with others. If you do, then copy the link at the top and bottom of this page into your email. If you just forward this email and the recipient unsubscribes, it will unsubscribe you as well.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
_______________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com/lifestylechange/.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.