Where Can You Get The Iodine You Need?
Author: Dr. Stephen Chaney
 It shouldn’t be happening. The introduction of iodized salt in the 1920s virtually eliminated iodine deficiency in this country. However, in just the past twenty years the incidence of iodine deficiency has increased 3-8-fold in women of childbearing age. Recent studies have estimated that today 30-40% of women of childbearing age are iodine deficient.
It shouldn’t be happening. The introduction of iodized salt in the 1920s virtually eliminated iodine deficiency in this country. However, in just the past twenty years the incidence of iodine deficiency has increased 3-8-fold in women of childbearing age. Recent studies have estimated that today 30-40% of women of childbearing age are iodine deficient.
How did that happen?
- We have been told to cut back on sodium. Many Americans have responded by throwing away the (iodized) salt shaker. Unfortunately, we still get a lot of salt from processed foods, and that salt is usually non-iodized.
- When we do add salt to our foods it is usually the “healthier” designer salts. First it was sea salt. Now it is trendy versions like Pink Himalayan Salt. While sea salt might have some iodine naturally, the trendier versions are non-iodized.
- The New-Age Whole Food diets often ban salt from the diet. That increases the probability of becoming iodine deficient. For example, a recent study reported that women who followed the Paleo diet for two years became iodine deficient (S. Manousi et al, European Journal of Clinical Nutrition, 72: 124-129, 2018).
The consequences of iodine deficiency, especially among women of childbearing age, are alarming. In a previous issue of “Health Tips From the Professor” I reported that iodine is essential for bone and neural development during fetal development and infancy.
This study (JL Mills et al, Human Reproduction, doi: 10.1093/humrep/dex379, 2018) reports that iodine deficiency also reduces a woman’s chances of becoming pregnant.
How Was The Study Done?
 This study recruited 501 couples (ages 18-40) from 16 counties in Michigan and Texas. The women had all discontinued conception within the previous two months with the intention of becoming pregnant and were followed for an additional 12 months. Women with known thyroid disease were excluded from the study.
This study recruited 501 couples (ages 18-40) from 16 counties in Michigan and Texas. The women had all discontinued conception within the previous two months with the intention of becoming pregnant and were followed for an additional 12 months. Women with known thyroid disease were excluded from the study.
Urine samples were collected from each woman at the beginning of the study to determine iodine and creatine levels. The women used fertility monitors to time intercourse relative to ovulation (Basically, that means they optimized their chances of becoming pregnant). They then used digital home pregnancy monitors on the day of expected menstruation to identify pregnancies.
Finally, 90% of the women took either a multivitamin or a prenatal vitamin during the study (The significance of this will be discussed later).
The Perils Of Iodine Deficiency For Women
 The results of the study were:
The results of the study were:
- 44.3% of the women in the study were iodine deficient (defined as iodine-creatine ratios of <100 mcg/g). This was further broken down to:
-
- 21.8% were mildly iodine deficient (50-99 mcg/g).
-
- 20.8% were moderately iodine deficient (20-49 mcg/g).
-
- 1.7% were severely iodine deficient (<20 mcg/g).
- That is a total of 22.5% who had moderate to severe iodine deficiency.
- Women who had moderate to severe iodine deficiency had a 46% decrease in the chance of becoming pregnant over each menstrual cycle compared to the iodine sufficient group.
A simple way of reporting those data would be to say that their chances of becoming pregnant were reduced by 46%, but that would not convey the whole picture. Most of the women did become pregnant during the 12-month study. However, it took the women with moderate to severe iodine deficiency twice as long to become pregnant. Iodine deficiency did not prevent pregnancy from occurring, but it delayed it.
The authors concluded: “In summary, our data show that groups of women with iodine concentrations in the moderate to severe deficient range experience a significantly longer time to pregnancy…The US and European countries where iodine deficiency is common should evaluate the need for programs to increase iodine intake for women of childbearing age, particularly those trying to become pregnant.”
And the increased difficulty in becoming pregnant is just the tip of the iceberg. As I mentioned above, the consequences of iodine deficiency among women of childbearing age, can be devastating.
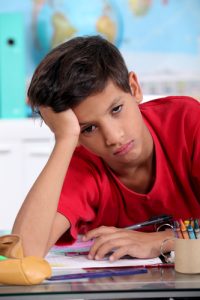
Iodine is essential for bone and neural development during fetal development and infancy. The American Academy of Pediatrics, The National Institutes Of Health, and the World Health Organization have all declared that mild iodine deficiency during pregnancy can prevent normal cognitive development and reduce IQ levels in children.
Because the consequences of iodine deficiency during pregnancy are so detrimental, if iodine deficiency also reduced the chances of a woman becoming pregnant, it could be considered a good thing. It could be part of Nature’s Plan. Unfortunately, this study suggests that iodine deficiency only delays pregnancy. It doesn’t prevent it.
Where Can You Get The Iodine You Need?
 Since iodine is so essential for a healthy pregnancy, the important question becomes: “Where can you get the iodine you need?”
Since iodine is so essential for a healthy pregnancy, the important question becomes: “Where can you get the iodine you need?”
- You could start by using old-fashioned iodized salt rather than designer salts in your salt shaker. However, I am reluctant to recommend anything that would increase sodium intake. We get far too much from processed foods already.
- Seafood (or seaweed, if you are a vegetarian) are the best food sources of iodine. However, our oceans are so contaminated I would recommend consuming those foods only occasionally.
- You will often see bread and dairy mentioned as good food sources because iodine was used in the preparation of those foods. However, iodine has largely been replaced by other agents, so those foods should no longer be considered good sources. For example:
-
- Iodine in commercial breads has traditionally come from the use of iodate as a dough conditioner. Today iodate has largely been replaced with bromide in commercial bread making. Not only does this trend decrease the amount of iodine available in our diet, but bromide also interferes with iodine utilization in our bodies
-
- Iodine in milk has traditionally come from the use of iodine-containing disinfectants to clean milk cans and teats. However, they have largely been replaced with other disinfectants
- Fruits and vegetables are a variable source of iodine, depending on where they were grown. That is because iodine levels in the soils vary tremendously from region to region.
- That leaves multivitamins and prenatal vitamins as your best source. However, you do need to read labels. You should look for supplements that provide 150 mcg of iodine. Unfortunately, only 50% of prenatal supplements in the United States even contain iodine. Remember, 90% of the women in this study took either a multivitamin or prenatal supplement and 44.3% of them were iodine deficient.
The Bottom Line
The introduction of iodized salt in the 1920s virtually eliminated iodine deficiency in this country. Now, almost 100 years later, iodine deficiency is back. Recent studies estimate that 30-40% of women of childbearing age are iodine deficient. This is concerning. Previous studies have shown iodine deficiency affects mental development during fetal development and infancy. A recent study suggests that iodine deficiency may also make it more difficult for women to become pregnant. Specifically, the study reported:
- 44.3% of the women in the study were iodine deficient. This was further broken down to:
-
- 21.8% were mildly iodine deficient.
-
- 20.8% were moderately iodine deficient.
-
- 1.7% were severely iodine deficient.
- That is a total of 22.5% with moderate to severe iodine deficiency.
- Women who had moderate to severe iodine deficiency had a 46% decrease in their chance of becoming pregnant over each menstrual cycle compared to the iodine sufficient group.
A simple way of reporting those data would be to say that their chances of becoming pregnant were reduced by 46%, but that would not convey the whole picture. Most of the women did become pregnant during the 12-month study. However, it took the women with moderate to severe iodine deficiency twice as long to become pregnant. Iodine deficiency did not prevent pregnancy from occurring, but it delayed it.
For more details about why iodine deficiency has reemerged in this country and where we can get the iodine we need, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.