The Truth About Seed Oils
Author: Dr. Stephen Chaney
The Seed Oil Myths
 You’ve seen the claims. “You should avoid all seed oils. They are toxic.”
You’ve seen the claims. “You should avoid all seed oils. They are toxic.”
Any time you see claims like, “Avoid all…[add the food villain of the day]” or “[a certain food] is toxic” your “truth-meter” should go on high alert. Claims like that are more likely to be hype than truth.
More specifically, the claims about seed oils are:
- They are heavily processed.
- They contain toxic ingredients.
- They are genetically modified.
- They cause inflammation and oxidative damage.
- They increase your risk of inflammatory diseases, heart disease, and cancer.
- A healthier option is to replace seeds oils with animal foods high in saturated fats.
Like any good food myth, there is a kernel of truth to each of these claims. In this article I will describe the kernel of truth associated with each of these claims, put them into perspective, and give practical guidelines for incorporating seed oils into your diet.
The topics I will cover are:
- The truth about fats.
- The truth about omega-6 fats.
- The truth about saturated fats.
- The truth about canola oil.
- The truth about seed oils.
The Truth About Fats
 The health authorities and media must think the American public is stupid. They oversimplify everything. They tell us:
The health authorities and media must think the American public is stupid. They oversimplify everything. They tell us:
- Animal fats are saturated fat.
- Olive oil is monounsaturated fat.
- Vegetable oils are omega-6 polyunsaturated fat.
- Fish oil is omega-3 polyunsaturated fat.
The truth is that every naturally occurring fat and oil is a mixture of all four kinds of fat. And each food contains a unique mixture of fats. The kernel of truth is:
- Animal fats have a higher percentage of saturated fat than other fats and oils.
- Olive oil has a higher percentage of monounsaturated fat than other oils.
- Vegetable oils have a higher percentage of omega-6 polyunsaturated fat than other oils.
- Fish oil has a higher percentage of omega-3 polyunsaturated fat than other oils.
But the full truth is that each food contains a unique mixture of fats. For example,
- Meat and butter from grass-fed animals contain a greater percentage of omega-3 fats than meat and butter from animals which were fattened on corn.
- Flaxseed oil has a higher percentage of omega-3 fats than other seed oils.
- High-oleic sunflower oil has the highest percentage of monounsaturated fat than other seed oils.
-
- Other vegetable oils with high monounsaturated fat content include olive oil, avocado oil, and canola oil. [Note: Although olive oil is the source of monounsaturated fat that we hear about most, avocado oil is equally high in monounsaturated fat and has a higher smoke point, which makes it a better choice for high-heat cooking.]
- Walnuts have a higher percentage of omega-3 fats than other nuts.
- Macadamia nuts and almonds have the highest percentage of monounsaturated fats than other nuts, with cashews and peanuts not far behind. Nut butters, of course, reflect the fat composition of the nuts.
The point I am making is that while myths are simple, the truth is much more complex.
Take Home Lesson: Every vegetable oil and every seed oil has a unique composition of fats. Each has its unique benefits and unique drawbacks.
That is something you will want to think about the next time you read an article about the dangers or the benefits of all seed oils. Every seed oil is unique. No generalization applies to all of them.
Biochemistry 101 – Essential Fats
 Let’s start with the most important point.
Let’s start with the most important point.
- Omega-6 fats and omega-3 fats are essential. Simply put, that means:
- We can’t make them.
- They are essential for life.
- We must get them from our diet.
If they are essential, the next question is, “Why do we need them?” Let me start with a little “Biochemistry 101” and talk about their role in cell membranes and cellular regulation.
Cell Membranes:
- You might think of cell membranes as a solid protective armor around the cells, but nothing could be farther from the truth. A better analogy would be the ocean that covers vast areas of our planet. Our membranes are quite fluid.
- And that membrane fluidity is important. Our cell membranes contain receptors like the cholesterol receptor and insulin receptor that must cluster together for cholesterol and insulin to be transported into the cell. Those receptors cluster best when cell membranes are very fluid.
- Our membranes are most fluid when they contain high levels of polyunsaturated fats (For membrane fluidity it doesn’t matter if they are omega-6 or omega-3). Conversely, our membranes are less fluid when they contain high levels of saturated fats.
- And here is the most important point. Because our bodies cannot make omega-6 and omega-3 polyunsaturated fats, this is the one time it is literally true that, “We are what we eat”. If our diets are high in saturated fats, our membranes are high in saturated fats. If our diets are high in polyunsaturated fats, our membranes are high in polyunsaturated fats. And the ratio of omega-6 and omega-3 polyunsaturated fats in our membranes reflects the ratio of omega-6 and omega-3 polyunsaturated fats in our diet.
Take Home Lesson: Diets high in omega-6 and/or omega-3 fats help lower cholesterol levels and improve blood sugar regulation.
Cellular Regulation:
- Our cells also use the polyunsaturated fats in our cell membrane to make hormone-like substances called prostaglandins and leukotrienes that exert profound effects on nearby tissues. [Note: For the sake of simplicity, I will just talk about prostaglandins for the rest of this article, but what I say applies equally to leukotrienes.]
- The enzymes that make prostaglandins do not distinguish between omega-6 and omega-3 polyunsaturated fats. They just use whatever polyunsaturated fat they come across.
- That’s important because the effects of omega-6 and omega-3 prostaglandins are often different and are sometimes opposite.
- Here’s where the “We are what we eat” principle comes into play. The ratio of omega-6 and omega-3s in our diet determines the omega-6 and omega-3 content of our membranes. And that determines the type of prostaglandins our cells produce.
Take Home Lessons:
- Some of the benefits of omega-6s are unique because they are dependent on omega-6 prostaglandins. These benefits cannot be duplicated by diets high in omega-3s.
- Because some effects of omega-6 and omega-3 prostaglandins are opposite, we need to look closely at the omega-6 to omega-3 ratio in the diet to optimize the health benefits of these two essential polyunsaturated fats.
Now, with Biochemistry 101 behind us, we are ready to look at the truth about omega-6 fats.
The Truth About Omega-6 Fats
Let’s start by looking at the pros and cons of omega-6 fats.
Pros Of Omega-6 Fats
Cellular Health: Omega-6 and fats are important for maintaining proper membrane fluidity. And omega-6 prostaglandins also regulate cell metabolism and cellular repair mechanisms.
Heart Health: Omega-6s are associated with lower risk of heart disease. This is caused by:
- Lower cholesterol levels due to proper membrane fluidity which allows clustering of cholesterol receptors.
- More flexible endothelial cells lining our arteries, which helps lower blood pressure and prevent blockage of the arteries by blood clots. This is most likely due to more fluid cell membranes and the production of beneficial prostaglandins.
- Some of these benefits are duplicated by omega-3 fats, but the American Heart Association stated in a recent Health Advisory (WS Harris et al, Circulation, 119, 902-907, 2009) that omega-6 fats are essential for some heart health benefits. They cannot be replaced by omega-3s.
Brain Health: Omega-3s get most of the press here, but experts feel that omega-6s play an important and independent role as well.
Fetal Growth and Development: Omega-6 fats are essential for normal neural development and growth. The mechanism(s) for this benefit are ill-defined.
Other Benefits:
- Omega-6 fats support healthy skin, hair, and bones. The mechanisms for these effects are unknown, but most experts feel they are independent of omega-3 fats.
- Omega-6 fats are also important for reproductive health. Most experts think this is due to the production of omega-6 prostaglandins.
Take Home Lesson: Omega-6 fats are essential for a healthy heart, a healthy brain, and normal fetal growth and development.
Cons Of Omega-6 Fats
 Oxidation: Omega-6 (and omega-3) fats are very susceptible to oxidation, especially at high temperatures. This can lead to free radical formation, which can promote the formation of cancer cells.
Oxidation: Omega-6 (and omega-3) fats are very susceptible to oxidation, especially at high temperatures. This can lead to free radical formation, which can promote the formation of cancer cells.
You may have seen the statement that omega-6 fats cause cancer. This is an oversimplification. A more accurate statement would be, “Improperly used, any polyunsaturated fat may increase cancer risk. But this is largely avoidable. Here are the precautions I recommend:
- Choose your source carefully.
-
- For seeds and nuts look for freshness. If they look or taste funny, throw them out.
-
- For oils choose reputable brands and choose ones that use low-heat processing. Also, look for ones with minimal processing. They may be cloudy rather than clear, but they will also contain naturally occurring antioxidants and polyphenols.
- Don’t overheat them.
-
- Most vegetable oils are only suitable for use as salad dressings and other room temperature cooking.
-
- The exceptions are vegetable oils with high smoke points – for example, olive oil for stir fries and avocado oil for higher temperature cooking.
- Store them safely. Don’t give them a chance to become oxidized.
-
- We store sunflower seeds and almonds in our refrigerator and walnuts in our freezer.
-
- We buy unsaturated vegetable oils in small quantities (so they are used up quickly) and store them in the refrigerator.
Take Home Lesson: Improperly used, omega-6 fats, like any unsaturated fat, can become oxidized and form free radicals (the kernel of truth). Choose your source carefully. Don’t overheat them. Store them safely.
 Inflammation: This is the one you hear the most about. You have been told that omega-6 vegetable oils (seed oils) cause inflammation. As a blanket statement, it is mostly untrue. But it does have a kernel of truth.
Inflammation: This is the one you hear the most about. You have been told that omega-6 vegetable oils (seed oils) cause inflammation. As a blanket statement, it is mostly untrue. But it does have a kernel of truth.
Let’s start with the kernel of truth:
- Omega-6 fats are inflammatory only when compared to omega-3 fats. You have also been told that omega-6 fats are inflammatory when compared to saturated fats. This is false, as I will discuss below.
Let me elaborate on the first statement with a little more Biochemistry 101 (If you haven’t guessed, that’s my favorite topic. Once a professor, always a professor).
- Omega-6 fats are converted into one inflammatory prostaglandin. Omega-3 fats are converted into several anti-inflammatory prostaglandins (This is an example of some omega-6 and omega-3 prostaglandins having opposite effects).
- Because of their opposite effects on inflammation, some experts say that the optimal ratio of omega-6 to omega-3 fats is in the range of 1:1 to 4:1. But the typical American diet is around 15:1.
If the omega-6 to omega-3 ratio is important (and not every expert agrees that it is), the statement that we should avoid omega-6-containing vegetable oils (seed oils) because they are inflammatory is mostly untrue.
-
- Every omega-6 oil has a different omega-6 to omega-3 ratio. For example,
-
- Corn oil has a 50:1 ratio and sesame oil has a 42:1 ratio. If you are just going by omega-6 to omega-3 ratios, you might want to avoid these.
-
- Soybean oil has a 7:1 ratio and extra virgin olive oil has a 5:1 ratio. They are almost in the optimal range.
-
- Canola oil has a 2:1 ratio. It’s in the optimal range.
-
- And flaxseed oil is the clear winner with a 1:4 ratio.
But the truth is also much more complex than you have been led to believe.
- The kernel of truth is that omega-6 fats can be converted to an inflammatory prostaglandin.
- But omega-6 fats can also be converted to anti-inflammatory prostaglandins. And some omega-6 fats such as GLA are anti-inflammatory.
- Human clinical studies find that omega-6 fats either have no effect on inflammation or decrease it slightly (A Poli et al, International Journal of Molecular Sciences, 24, 4567, 2023).
Take Home Lesson: Omega-6 fats are converted into one inflammatory prostaglandin (the kernel of truth). But they are also converted to anti-inflammatory prostaglandins. The net effect in the human body is a slight anti-inflammatory effect.
The Truth About Saturated Fats

You have been told that saturated fats are anti-inflammatory and decrease the risk of heart disease. For many Americans those claims are enticing because it means they don’t have to change their diet. But are the claims true?
You have been told that these claims are based on science. There are clinical studies behind them. Is that true?
The problem is that there are a lot of bad studies on saturated fats in the literature, and the Dr. Strangeloves of the world cherry pick the ones that support their beliefs.
If you want to compare the effect of different kinds of fat on either inflammation or heart health, you must make sure that all other components of the diet are the same. Too many of these studies have compared a whole food diet high in saturated fat with the typical American diet high in omega-6 fats. The results are predictable. Anything is better than the typical American diet.
In a previous issue of “Health Tips From The Professor” I discussed the criteria for a good study of fats. High quality studies must:
- Show the subjects stick with the new diet for the duration of the study. Subjects find it difficult to adhere to a diet to which they are not accustomed long term and often revert to their more familiar diet. This requires either very close monitoring of what the subjects are eating or measurement of fat membrane composition to verify diet adherence, or both.
- Carefully control or measure what the saturated fats are replaced with. In good studies only the fat composition of the diet changes. All other components of the diet remain the same.
- Last two years or more. The fats we eat determine the fat composition of our cell membranes, and that is what ultimately determines both inflammation in our bodies and our risk of dying from heart disease. While it is true to say, “We are what we eat”, changing the fat composition of our cell membranes does not occur overnight. It takes 2 years or more to achieve a 60-70% change in the fat composition of cell membranes.
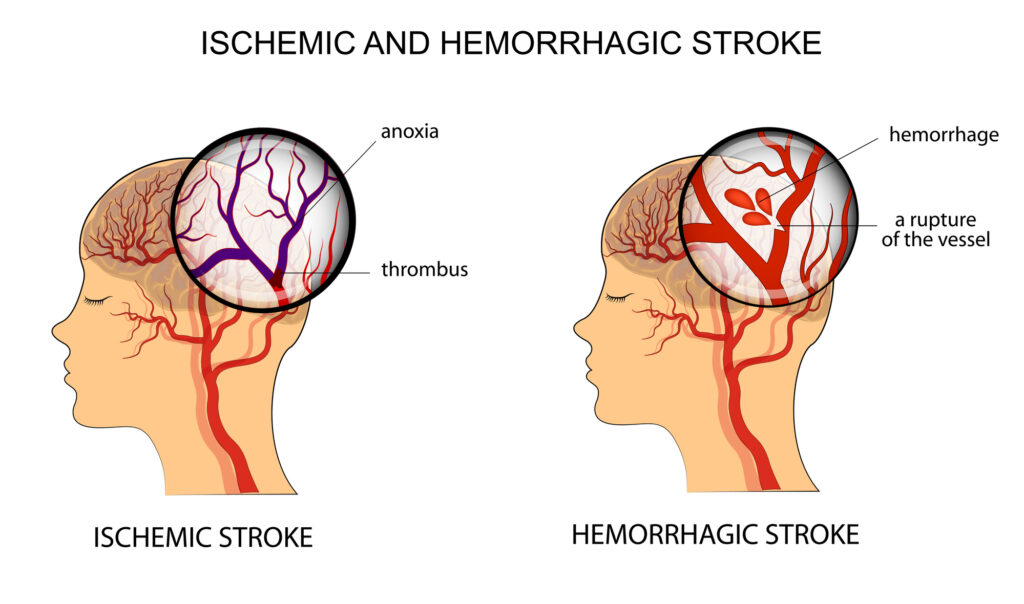
- Measures multiple markers of inflammation or actual cardiovascular end points such as heart attack, stroke, and deaths due to heart disease.
 When studies are done that meet these criteria the results are as follows:
When studies are done that meet these criteria the results are as follows:
Inflammation (A Poli et al, International Journal of Molecular Sciences, 24: 4567, 2023):
- Replacing saturated fats with omega-6 fats reduces inflammation by 8%.
- Replacing saturated fats with omega-3 fats reduces inflammation by 48%
Heart Disease (FM Sacks et al, Circulation, 136, Number 3, 2017):
- Replacing saturated fats with omega-6 from decreased the risk of heart disease by 24%.
- Replacing saturated fats with a mixture of both omega-6 and omega-3 fats decreased the risk of heart disease by 29%. This is equivalent to statin therapy, without the side effects.
- When the replacement of saturated fats with omega-6 and omega-3 fats occurred in the context of a heart healthy diet such as the Mediterranean diet, heart disease risk was reduced by 47%.
The Food and Nutrition Board of the Institute of Medicine recommends that Americans not exceed 10% of calories from saturated fat.
- Two thirds of Americans exceed this limit.
The Food and Nutrition Board recommends that omega-6 fats be around 5-6% of calories. Because omega-6 fats play an important role in heart health, the American Heart Association recommends they be at 5-10% of calories.
- Americans get around 6.5% of their calories from omega-6 fats.
Take Home Lesson: Replacing saturated fat with omega-6 fats reduces both inflammation and heart disease risk. Adding omega-3 fats reduces both even more. So, bringing omega-6 and omega-3 into a better balance is a good idea. But omega-6 fats are essential and are at the recommended intake for most Americans, so don’t do this by cutting back on healthy omega-6 fats. Instead, add some more omega-3s.
The Truth About Canola Oil
 There are a lot of things t like about canola oil:
There are a lot of things t like about canola oil:
- It is an excellent source of healthy omega-6 fats.
- It has a good omega-6 to omega-3 ratio (2:1), which makes it anti-inflammatory.
- It is also a good source of monounsaturated fats and has a moderate smoke point, which makes it suitable for low heat cooking.
So, why is it so unpopular? Unfortunately, it suffers from a lot of undeserved myths. Each has a kernel of truth. But like a secret passed around the room, the myths have grown with each repetition, and the truth has become unrecognizable.
So, let’s try to separate the myths from the truth.
Myth: Canola oil is genetically engineered.
Truth: It was created by old-fashioned plant breeding.
Myth: Canola oil contains toxic ingredients.
Truth:
- Rapeseed oil comes from the oilseed rape plant (a relative of mustard).
- Rapeseed oil contains erucic acid and glucosinolates, both of which can be toxic in large amounts (the kernel of truth).
- Baldur Stefansson from the University of Manitoba bred a “double low” variety the oilseed rape plant which produces an oil that contains <2% of both erucic acid and glucosinolates and is safe for human consumption. This new oil was named canola oil (from Canada and ola for oil).
- Both cultivars of the oilseed rape plant are still grown. Rapeseed oil is used for industrial purposes, and canola oil is used for human consumption.
- Canola oil is tightly regulated in Canada, the US, and the EU to <2% erucic acid.
- 98% of the canola oil sold in the US is grown in Canada and the northern US.
Myth: Canola oil is unhealthy.
Truth: Because it is one of the least expensive omega-6 oils, canola oil is often found as an ingredient in unhealthy, highly processed, food (the kernel of truth). The solution is simple. Avoid unhealthy foods. Adding a different kind of fat to unhealthy foods is not going to make them healthier.
The Truth About Seed Oils
 By now I have covered most of the myths about seed oils in my sections on omega-6 fats and canola oil, but here is a quick review.
By now I have covered most of the myths about seed oils in my sections on omega-6 fats and canola oil, but here is a quick review.
Myth: All seed oils are…[add your favorite derogatory term here].
Truth: Every seed oil has a unique composition of fats. Each has its unique benefits and unique drawbacks.
Myth: Seed oils are genetically modified.
Truth: The plants producing canola oil and high oleic sunflower oil have been modified (the kernel of truth), but they were modified by conventional plant breeding rather than genetic engineering.
Myth: Seed oils contain toxic ingredients. This myth is most often directed at canola oil.
Truth: Rapeseed oil contains components that can be toxic at high levels (the kernel of truth). However, the rapeseed plant has been bred to produce canola oil with safe levels of those components.
Myth: Seed oils are inflammatory, which increases your risk of inflammatory diseases and heart disease.
Truth: Seed oils contain omega-6 fats which can be converted into one inflammatory prostaglandin (the kernel of truth). But they are also converted to anti-inflammatory prostaglandins. The net effect in well done human clinical trials is a slight anti-inflammatory effect.
Myth: Seed oils cause oxidative damage, which increases your risk of cancer.
Truth: Seed oils (like any polyunsaturated fat) are susceptible to oxidation, especially at high temperatures. This can lead to free radical formation and oxidative damage (the kernel of truth). But this is only true when you use them improperly. The solution is to store them safely and to not overheat them when cooking.
Myth: Saturated fats are healthier than seed oils. Replacing saturated fat with the omega-6 fats found in seed oils increases inflammation and heart disease risk.
Truth: Many studies in this area of research are poorly designed. Well-designed studies show that replacing saturated fat with the omega-6 fats found in seed oils reduces both inflammation and heart disease risk.
Myth: Omega-3 fats are healthier than the omega-6 fats found in seed oils, so we should replace seed oils with omega-3 fats.
Fact: Omega-3 fats are more effective than omega-6 fats at reducing inflammation and heart disease risk (the kernel of truth). However, omega-6 fats are essential for a healthy heart, a healthy brain, and normal fetal growth and development. We can’t make them, so we must get them from our diet. Americans are currently consuming the recommended amount of omega-6 fats. So, we should not decrease the amount of omega-6 fats in our diet. Instead, we would benefit from adding more omega-3s to our diet.
Myth: Seed oils are highly processed. High heat processing alters the oils. Processing also removes beneficial antioxidants and polyphenols from the oils.
Truth: This is mostly true. The solution is to choose your brands carefully.
- For oils choose reputable brands and choose ones that use low-heat processing. Also, look for ones with minimal processing. They may be cloudy rather than clear, but they will also contain naturally occurring antioxidants and polyphenols.
-
- It’s not easy to choose your source carefully. But this difficulty is not unique to seed oils. For example:
-
-
- The term EVO is supposed to mean extra virgin olive oil was used, but cheaper oils are sometimes blended into the olive oil to save money.
-
-
-
- If a company wishes to use the term “grass fed” on their product, they must file a certification with the USDA, but the USDA does not inspect to determine whether the certification is accurate.
-
- Seed oils are also found as an ingredient in unhealthy, highly processed foods. The solution here is simple. Avoid unhealthy foods. Adding a different kind of fat to unhealthy foods is not going to make them healthier.
For more details about each of these Truth statements, read the article above.
The Bottom Line
There are many myths about seed oils. Each myth has a kernel of truth but is mostly false. In this week’s “Health Tips From the Professor” I discuss the myths and truths about seed oils. Because this is a complex subject, I have broken it down into individual topics that address one or more seed oil myths before talking about seed oil myths directly.
The topics I covered are:
- The truth about fats.
- The truth about omega-6 fats.
- The truth about saturated fats.
- The truth about canola oil.
- The truth about seed oils.
For more details read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
______________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.