We Have Been Asking The Wrong Questions
Author: Dr. Stephen Chaney
 Today’s Health Tip is a follow-up to the article I published last month on omega-3s and heart disease risk. In that article I pointed out the reasons why studies of the effect of omega-3s and heart disease risk have been so confusing.
Today’s Health Tip is a follow-up to the article I published last month on omega-3s and heart disease risk. In that article I pointed out the reasons why studies of the effect of omega-3s and heart disease risk have been so confusing.
One of the reasons is that many of the studies have been asking the wrong questions.
- They were asking whether omega-3s reduced the risk of heart disease for everyone. Instead, they should have been asking who benefited from omega-3 supplementation.
- They were asking whether omega-3s reduced the risk of all forms of heart disease combined. Instead, they should have been asking whether omega-3s reduced the risk of specific kinds of heart disease.
I also discussed a large clinical trial, the VITAL study, that was designed to answer those two questions.
The study I will describe today (L Djoussé et al, JACC Heart Failure, 10: 227-234, 2022) mined the data from the VITAL study to evaluate the effect of omega-3 supplementation on congestive heart failure, a form of heart disease that was not discussed in the VITAL study.
Everything You Need To Know About Congestive Heart Failure
 Congestive heart failure is a killer. The term congestive heart failure simply means that your heart no longer pumps blood well. The initial symptoms are relatively non-specific and include things like.
Congestive heart failure is a killer. The term congestive heart failure simply means that your heart no longer pumps blood well. The initial symptoms are relatively non-specific and include things like.
- Shortness of breath.
- Fatigue and weakness.
- Reduced ability to exercise.
- Rapid or irregular heartbeat.
- Persistent cough or wheezing.
However, as it progresses, the symptoms get much worse. Fluid builds up in your tissues.
- Fluid buildup in your legs, ankles, and feet can make it difficult to walk.
- Fluid buildup in your lungs makes it difficult to breathe. In advanced stages it can feel like you are drowning in a room full of air.
According to the CDC:
- 4 million Americans have congestive heart failure (CHF).
-
- It leads to ~380,000 deaths/year.
- 83% of patients diagnosed with CHF will be hospitalized at least once.
-
- 67% will be hospitalized two or more times.
- CHF costs >$30 billion per year in health care costs and lost wages.
The risk of congestive heart failure is not spread evenly across the American population. Black Americans and Americans with type 2 diabetes are at increased risk.
According to the Framingham Heart Study:
- Type 2 diabetes increases the risk of CHF 2-fold in men and 5-fold in women. The reasons are not entirely clear. However:
-
- High blood sugar is thought to either damage cells in heart muscle, weakening it, or damage small blood vessels within the heart, making it more difficult for the heart to pump blood.
-
- Some diabetes drugs that lower blood sugar also appear to increase the risk of congestive heart failure.
According to the CDC:
- Black Americans are 2-fold more likely to develop CHF than White Americans. Again, the reasons are not clear. However:
-
- Some experts feel it could be due to the higher incidence of untreated high blood pressure in Black Americans.
In summary:
- Congestive heart failure is a serious disease. Its symptoms affect your quality of life, and it can lead to hospitalizations and death.
- Black Americans and Americans with type 2 diabetes are at higher risk of developing congestive heart failure.
How Was The Study Done?
The VITAL study, from which these data were extracted, was a placebo-controlled clinical trial designed to measure the effects of 1,000 mg omega-3 supplementation on the risk of developing heart disease. It enrolled 25,871 Americans aged 55 years or older and followed them for an average of 5.3 years.
The participants enrolled in the VITAL study represented a cross-section of the American population. Most were at low risk of heart disease, but there were subsets of the study group who were at higher risk of heart disease. A strength of the VITAL study was that it was designed so the high-risk subgroups could be evaluated separately.
The current study utilized data from the VITAL study to look at the effect of omega-3 supplementation on hospitalizations due to congestive heart failure. It also evaluated the effect of type 2 diabetes and race on the risk of hospitalizations.
Omega-3s And Congestive Heart Failure
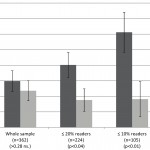
 When the investigators looked at the whole population, most of whom were at low-risk of congestive heart failure, they did not see any effect of omega-3 supplementation on the risk of hospitalizations due to congestive heart failure.
When the investigators looked at the whole population, most of whom were at low-risk of congestive heart failure, they did not see any effect of omega-3 supplementation on the risk of hospitalizations due to congestive heart failure.
However, when they looked at high risk groups, the story was much different.
In patients with type-2 diabetes:
- Omega-3 supplementation reduced the risk of the initial hospitalization for congestive heart failure by 31%
- Omega-3 supplementation reduced the risk of multiple hospitalizations due to congestive heart failure by 47%.
The effect of omega-3 supplementation on hospitalizations was greatest for the Black participants in the study.
In the words of the authors, “Our data show beneficial effects of omega-3 fatty acid supplements on the incidence of heart failure hospitalizations in participants with type 2 diabetes but not in those without type 2 diabetes, and such benefit appeared to be stronger in Black participants with type 2 diabetes.”
We Are Asking The Wrong Questions
 As I said above, there is so much confusion about the effect of omega-3s on heart disease because we scientists have been asking the wrong questions:
As I said above, there is so much confusion about the effect of omega-3s on heart disease because we scientists have been asking the wrong questions:
- We have been asking whether omega-3s reduce the risk of heart disease for everyone. Instead, we should have been asking who benefits from omega-3 supplementation.
- We have been asking whether omega-3s reduced the risk of all forms of heart disease combined. Instead, we should have been asking whether omega-3s reduced the risk of specific kinds of heart disease.
In my “Health Tip” last month I discussed a large clinical study, the VITAL study, that was specifically designed to answer the right questions. Like so many other studies it found that omega-3 supplementation did not significantly reduce the risk of all kinds of heart disease for everyone.
However, what it did find was more important than what it did not find:
- When they looked at the effect of omega-3s on heart disease risk in high-risk groups, they found that major cardiovascular events were reduced by:
-
- 26% in African Americans.
-
- 26% in patients with type 2 diabetes.
-
- 17% in patients with a family history of heart disease.
-
- 19% in patients with two or more risk factors of heart disease.
- When they looked at the effect of omega-3s on heart disease risk in people with low omega-3 intake, they found that omega-3 supplementation reduced major cardiovascular events by:
-
- 19% in patients with low fish intake.
- When they looked at the effect of omega-3s on the risk of different forms of heart disease, they found that omega-3 supplementation reduced:
-
- Heart attacks by 28% in the general population and by 70% for African Americans.
-
- Deaths from heart attacks by 50%.
-
- Deaths from coronary heart disease (primarily heart attacks and ischemic strokes (strokes caused by blood clots)) by 24%.
In other words, when they asked the wrong questions, they got the wrong answer. If they had just looked at the effect of omega-3 supplementation on all forms of heart disease for everyone (like most other omega-3 studies), they would have concluded that omega-3s are worthless.
However, when they asked the right questions, they found that omega-3s were very beneficial for high-risk populations and for certain types of heart disease.
The current study utilized the same data to analyze the effect of omega-3 supplementation on hospitalizations due to congestive heart failure. And the results were similar.
If they had asked the wrong question, “Does omega-3 supplementation reduce congestive heart failure hospitalizations for everyone?”, they would have concluded that omega-3 supplementation was worthless.
However, instead they asked, “Does omega-3 supplementation reduce congestive heart failure hospitalizations for certain high-risk groups” and were able to show that omega-3 supplementation significantly reduced congestive heart failure hospitalizations for people with type 2 diabetes and for Blacks.
We need to change the paradigm for clinical studies of supplements. The old paradigm asks the wrong questions. If we really want to know the role of supplementation for our health, we need to start asking the right questions.
The Bottom Line
There is perhaps nothing more confusing to the average person than the “truth” about omega-3 supplementation and heart disease risk. Much of the confusion is because we have been asking the wrong questions:
- We have been asking whether omega-3 supplementation reduces the risk of heart disease for everyone. Instead, we should have been asking who benefits from omega-3 supplementation.
- We have been asking whether omega-3 supplementation reduces the risk of all forms of heart disease combined. Instead, we should have been asking whether omega-3 supplementation reduces the risk of specific kinds of heart disease.
A recent study on the effect of omega-3 supplementation on hospitalizations due to heart disease is a perfect example.
If they had asked the wrong question, “Does omega-3 supplementation reduce congestive heart failure hospitalizations for everyone?”, they would have concluded that omega-3 supplementation was worthless.
However, instead they asked, “Does omega-3 supplementation reduce congestive heart failure hospitalizations for certain high-risk groups” and were able to show that omega-3 supplementation significantly reduced congestive heart failure hospitalizations for people with type 2 diabetes and for Blacks.
We need to change the paradigm for clinical studies of supplements. The old paradigm asks the wrong questions. If we really want to know the role of supplementation for our health, we need to start asking the right questions.
For more details read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.