A Holistic Approach For Preventing Dementia
Author: Dr. Stephen Chaney
 You already know that processed foods are not your friend. In previous issues of “Health Tips From the Professor” I have covered the linkage between processed food consumption and obesity, diabetes, heart disease, cancer, stroke, and premature death.
You already know that processed foods are not your friend. In previous issues of “Health Tips From the Professor” I have covered the linkage between processed food consumption and obesity, diabetes, heart disease, cancer, stroke, and premature death.
I have also covered the linkage between processed food consumption and mood, particularly anxiety and depression.
If you want to read some of those articles, just go to https://chaneyhealth.com/healthtips/ and put processed foods in the search box.
But what if they also affect cognition? What if they increase your risk of dementia?
Of all the diseases associated with aging, dementia is perhaps the scariest. What use is it to reach your “golden years” if you can’t recognize friends and family, you lose your precious memories, and you cannot perform the most basic functions for yourself.
That’s why I found the study (H Li et al, Neurology, 99(10)e1056-e1066, 2022) I am discussing today so interesting. It looks at the association of ultraprocessed food consumption and dementia.
I realized that “ultraprocessed food” is not a familiar term for most of you. So, before I discuss the article, I will describe how scientists define ultraprocessed food.
What Are Ultraprocessed Foods?
 Before I proceed with describing the findings of this study, I should probably contrast the common definition of processed foods with the current scientific definition of ultraprocessed foods.
Before I proceed with describing the findings of this study, I should probably contrast the common definition of processed foods with the current scientific definition of ultraprocessed foods.
The scientific community has recently developed something called “The NOVA food classification system” to describe the various levels of food processing.
The NOVA system categorizes foods into four groups according to the extent of processing they have undergone:
#1: Unprocessed or minimally processed foods.
- This category includes foods like fruit, vegetables, milk, and meat.
#2: Processed culinary ingredients.
- This category includes foods you might find in restaurants or prepare yourself to which things like sugar, vegetable oils, butter, or cream were added in the preparation.
#3: Processed foods.
- This category includes foods like canned vegetables, freshly made breads, and cheeses.
#4: Ultraprocessed foods.
- This category includes foods like soft drinks, chips, packaged snacks, most breakfast cereals, chicken nuggets & fish sticks, fast food burgers, hot dogs, and other processed meats.
The actual list is much longer, but you get the idea. What we call processed foods; scientists call ultraprocessed foods. Since the term “ultraprocessed foods” has not yet entered the popular vocabulary, I will use the term “processed foods” in describing the results of this study because it is more understandable to the average reader.
How Was This Study Done?
 The authors used information from the UK Biobank Study. The UK Biobank Study enrolled 500,000 people from England, Scotland, and Wales between 2006-2010 and has followed them continuously until the present. The participants were aged 40-69 on enrollment. The UK Biobank study collects health, lifestyle, environmental, and biological data from participants and makes the data available for studies such as this one.
The authors used information from the UK Biobank Study. The UK Biobank Study enrolled 500,000 people from England, Scotland, and Wales between 2006-2010 and has followed them continuously until the present. The participants were aged 40-69 on enrollment. The UK Biobank study collects health, lifestyle, environmental, and biological data from participants and makes the data available for studies such as this one.
This study included 72,083 participants from the UK Biobank study who:
- Were 55 years or older on enrollment.
- Were free from dementia on enrollment.
- Had completed at least two 24-hour dietary assessments during the study.
The participants were followed for an average of 10 years.
Newly diagnosed cases of dementia were obtained through electronic linkages to hospital and mortality records (Yes, Big Brother is watching, especially in countries like England).
Ultraprocessed food intake (defined as described above) was determined from the 24-hour dietary recalls. Participants were divided into quartiles (4 groups) based on the amount of ultraprocessed foods in their diet.
The study measured the association between ultraprocessed food consumption and dementia. The data were statistically corrected for other lifestyle factors that affect cognition, such as age, sex, family history, and obesity.
As I said above, since the term “ultraprocessed foods” has not yet entered the popular vocabulary, I will use the term “processed foods” in describing the results of this study because it is more understandable to the average reader.
Can Processed Foods Cause Dementia?
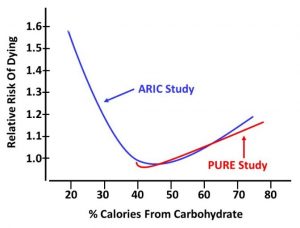
For every 10% increase in calories from processed foods, the risk of:
- Dementia from all causes increased by 25%.
- Alzheimer’s disease increased by 14%.
- Vascular dementia (dementia caused by a blood clot or brain bleed) increased by 29%.
When they compared those in the highest quartile of processed food consumption with those in the lowest quartile:
- The risk of dementia from all causes increased by 51%.
The only good news from the study was that replacing 10% calories from processed food with an equal proportion of unprocessed or minimally processed foods decreased the risk of dementia by 19%.
The authors hypothesized that the increase in dementia caused by processed foods could be due to:
- Displacement from the diet of whole, unprocessed foods that have been shown to decrease dementia risk.
- The high sodium content of processed foods can cause hypertension, which decreases cerebral blood flow and has been shown to increase the risk of dementia.
- Diets high in processed foods promote systemic inflammation, which accelerates neurodegeneration and increases the risk of dementia.
- Processed foods contain food additives and molecules formed during processing which have been shown to have negative effects on cognition and memory.
The authors concluded, “[Our study shows]…higher consumption of ultraprocessed foods was associated with higher risk of dementia, and substituting unprocessed or minimally processed foods for ultraprocessed foods was associated with a lower risk of dementia.”
What Does This Study Mean For You?
 You already know that a diet high in processed foods:
You already know that a diet high in processed foods:
- Is associated with obesity.
-
- Increases your risk of:
-
- Diabetes
-
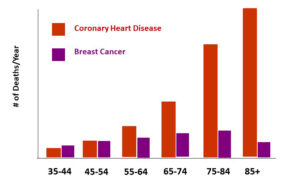
- Heart Disease
-
- Cancer
-
- High Blood Pressure
-
- Stroke
-
- Premature death
- Can increase your risk of anxiety and depression.
Their effect on dementia is just one more reason to do away with processed foods and replace them with whole, unprocessed foods.
But that is a tall order for most Americans who get 55% of their calories from processed foods. It is difficult to make wholesale changes in your diet, so I will leave you a bit of good news.
The authors reported that even minor improvements in diet could have beneficial effects. For example:
- Replacing as little as 50 grams of processed food with 50 grams of unprocessed foods (equivalent to half an apple, a serving of corn, or a bowl of bran cereal) decreases your risk of dementia by 3%.
That may not seem like much. But what if you make that change in month one? Then in month 2 replace another 50 grams of processed food with unprocessed food and keep repeating that process month after month. At the end of a year:
- You would have decreased your risk of dementia by 36%.
- You may have lost weight without going on a restrictive weight loss diet.
- You would have significantly decreased your risk of diabetes, heart disease, cancer, and several other diseases.
- You might even be calmer and happier.
A Holistic Approach For Preventing Dementia
 Of course, for best results you want to do more than just avoid processed foods. A holistic approach is best.
Of course, for best results you want to do more than just avoid processed foods. A holistic approach is best.
- Eat a healthy diet.
-
- As the study suggested, replace processed foods with whole, unprocessed fruits, vegetables, fish, nuts, legumes, and low-fat dairy.
-
- Red meats and unprocessed foods high in saturated fat are better than highly processed foods, but they are not optimal.
-
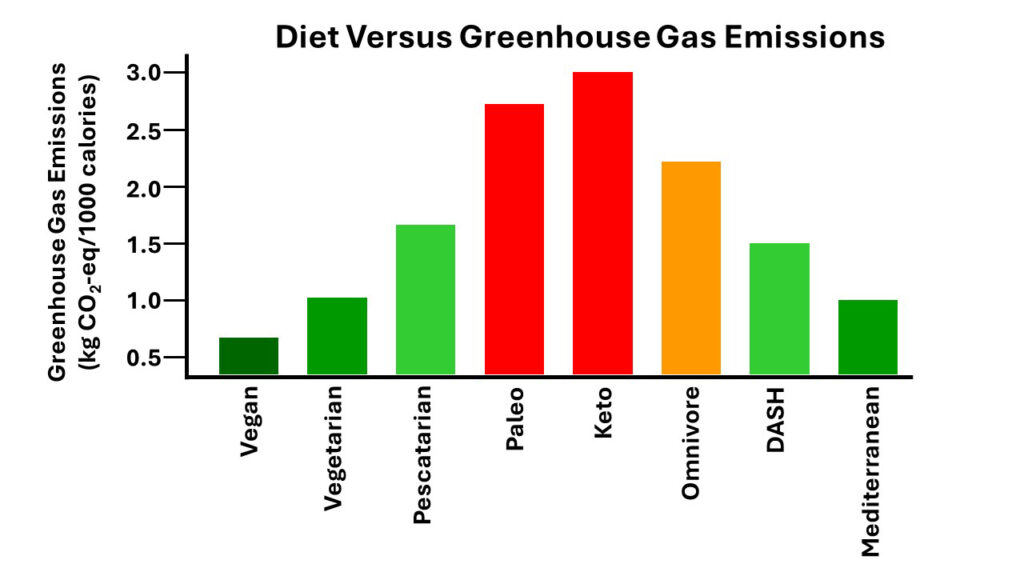
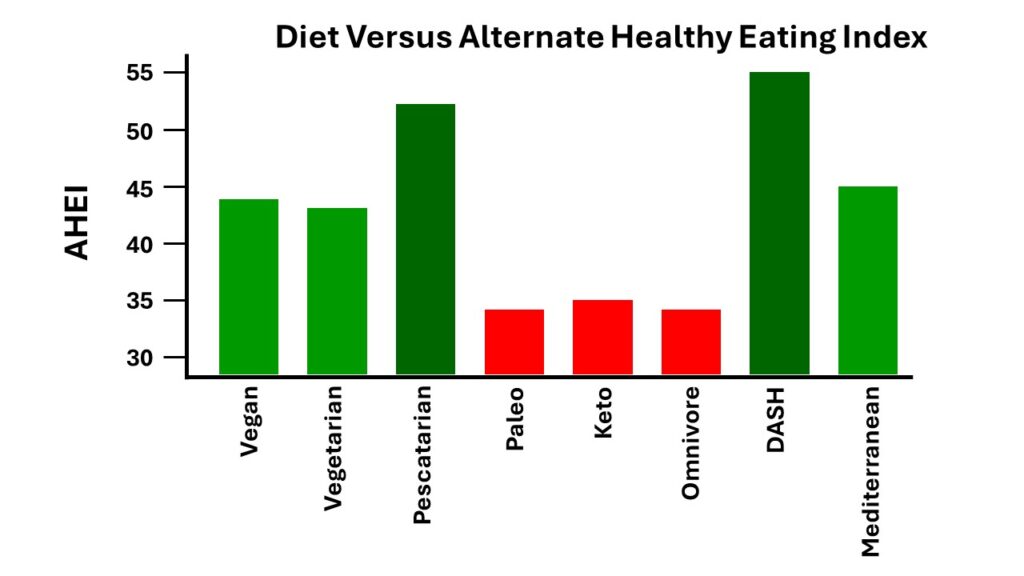
- As for specific diets, the Mediterranean, DASH, and MIND diets are backed by clinical studies showing that they slow cognitive decline and reduce dementia risk.
- Get plenty of omega-3 fatty acids.
-
- Some of those omega-3s can come from fatty, cold-water fish, but most people will need an omega-3 supplement providing 500-1,000 mg of EPA and DHA.
-
- Some studies claim DHA works best. Others report that EPA works best. I would recommend a supplement that provides both.
- Exercise regularly.
-
- Exercise improves blood flow to the brain, and that is a good thing.
- Control your weight.
-
- Obesity increases chronic inflammation and the risk of dementia.
-
- You don’t need to become ‘twiggy”. Even small decreases in body weight help slow cognitive decline.
- Socialize with friends and family.
-
- Scientists don’t know how this works, but it does.
-
- This requires physical interactions. Facebook friends don’t count.
- Exercise your mind.
-
- This can be things like crossword puzzles, sudoku, or new projects that require creativity.
-
- Learn new things. It could be a new language, new dance step, or new skill.
The Bottom Line
You already knew that diets high in processed foods increase your risk of obesity, diabetes, heart disease and several other diseases. And diets high in processed foods may leave you feeling anxious and depressed.
A recent study added to the bad news about processed foods. It looked at the association of processed foods and dementia. It found that:
- Diets high in processed foods increase the risk of dementia by as much as 51%.
- The only good news from the study was that replacing 10% calories from processed food with an equal proportion of unprocessed or minimally processed foods decreased the risk of dementia by 19%.
For more details about the study, what it means for you, and a holistic approach for brain health read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 53 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.