The Flaws And Blind Spots In This Study
Author: Dr. Stephen Chaney

Has the omega-3 pendulum swung again? The recent headlines are downright scary. For example:
- “Fish Oil May Increase the Risk of Stroke and Heart Conditions.”
- “Fish Oil Supplements May Cause Harm, Study Finds. Is It Time to Ditch Them?”
- “Fish Oil Supplements May Lead to Heart Problems”.
- “Regular Use of Fish Oil Supplements Might Increase, Rather Than Lessen, The Risk of First Time Heart Disease and Stroke Among Those in Good Cardiovascular Health.”
Yikes! That sounds bad. Should we be thinking about giving up our omega-3 supplements?
But wait. Just a few weeks earlier we were reading headlines about the benefits and lack of side effects from omega-3 supplements. That’s confusing. Which headlines are correct?
To answer these questions:
- I will review the study (G Chen et al, BMJ Medicine 2024; 3e000451.doi.10.1136/bmjmed-2022-000451) behind the headlines.
- I will point out the flaws and blind spots in the study.
- I will strip away the hyperbole and put the headlines into perspective.
How Was The Study Done?
 The investigators made use of data from the UK Biobank Study. The UK Biobank Study is a large, long-term study in the United Kingdom which was designed to investigate the contributions of genetic predisposition and environmental exposure [including diet and supplementation] to the development of disease.
The investigators made use of data from the UK Biobank Study. The UK Biobank Study is a large, long-term study in the United Kingdom which was designed to investigate the contributions of genetic predisposition and environmental exposure [including diet and supplementation] to the development of disease.
The UK Biobank Study enrolled 502,461 participants, aged 40-69 years, between January 1st, 2006 and December 31st, 2010. Participants were followed from entry into the program until March 31st 2021, an average of 11.9 years.
The current study excluded any participants who had a diagnosis of atrial fibrillation, heart failure, heart attack, stroke, or cancer at entry into the study, leaving 415,737 participants.
The participants were:
- 55% women.
- Average age of 56 years, with 83.4% of them below 65 years old at entry into the study.
- 94.5% white.
The study was designed in a unique manner, in that it was designed to test the effect of omega-3 supplements on 6 specific transitions:
- Primary prevention. This measured the transition of healthy (no diagnosed heart disease) people to either atrial fibrillation, major cardiovascular events, or death.
- Secondary prevention. This measured the transition from atrial fibrillation to either major cardiovascular events or death.
- Tertiary prevention. This measured the transition from major cardiovascular events to death.
- Major cardiovascular events were further broken down to heart attacks, stroke and heart failure.
Participants were asked whether they used fish oil supplements when they entered the study and were categorized as either regular users or non-users. [Note: The users were not asked the dose or brand of fish oil supplements they used.]
Deaths were obtained from the national death registry and disease diagnosis from the National Health Service.
Are Omega-3 Supplements Safe?
Primary Prevention – For healthy individuals (defined as having no diagnosed heart disease) using omega-3 supplements for an average of 11.9 years:
- Increased the risk of atrial fibrillation by 13%.
- Did not affect the risk of major cardiovascular events and death were unaffected by omega-3 supplementation.
- When major cardiovascular events were broken down to their component parts, omega-3 supplementation:
-
- Decreased the risk of heart failure by 8%.
-
- Increased the risk of stroke by 5% (this was just barely statistically significance).
-
- Did not affect the risk of heart attack.
Secondary Prevention – For individuals with atrial fibrillation omega-3 supplementation:
- Decreased the risk of major cardiovascular events by 9%.
- Decreased the risk of death by 8%.
- When major cardiovascular events were broken down into their component parts, omega-3 supplementation:
- Decreased the risk of heart attacks by 15%.
- Had no effect on the risk of stroke or heart failure.
Tertiary Prevention – For people who suffered major cardiovascular events during the study omega-3  supplementation:
supplementation:
- Decreased the risk of death by 8%.
Since this is a very complex set of data, I have coded positive results in green and negative results in red.
And as if these complexities were not enough, when the investigators broke these effects down by population groups:
- Omega-3 supplementation decreased the transition from healthy to death for men (7% decrease) and participants older than 65 (9% decrease).
I will discuss the significance of these observations below.
The authors concluded, “Regular use of fish oil supplements might be a risk factor for atrial fibrillation and stroke among the general population but could be beneficial for [reducing] progression of cardiovascular disease from atrial fibrillation to major adverse cardiovascular events, and from atrial fibrillation to death.”
In short, they were suggesting that omega-3 supplements should be avoided by the general population because they have no positive benefits and might increase the risk of atrial fibrillation and stroke. But omega-3 supplements may be useful for those who already have heart disease.
Some of the articles you may have read about the study repeated this message. Others just emphasized the negative aspects of the study.
But is this message accurate? Let me start by discussing the flaws, blind spots, and hidden data in this study. Then I will summarize the 3 key findings of the study and tell you what they mean for you.
The Flaws, Blind Spots, And Hidden Data In This Study
 Flaws: As I said above, there were two major flaws in the study.
Flaws: As I said above, there were two major flaws in the study.
Flaw #1: The study did not identify the dose of supplement used. This is important because the increased risk of atrial fibrillation and stroke is primarily seen in clinical trials using high dose omega-3 supplements.
Flaw #2: This was an association study which cannot prove cause and effect. However, the authors of this study reported it as showing that omega-3 supplement use caused atrial fibrillation and stroke – and all the news reports on the study have repeated that claim.
Flaw #3: Other experts have pointed out that the authors inflated the risks associated with omega-3 supplementation by reporting relative risk rather than absolute risk. Let me try to simplify the distinction.
The risk of atrial fibrillation was 4.24% in the non-supplement users and 4.80% in the omega-3 supplement users. That is an absolute increase in risk of 0.56% (4.80% – 4.24%). This is the increase in risk you actually experience. In contrast, 4.80% is 13% greater than 4.24%, which is how relative risk is calculated.
In response to the questions you are probably thinking:
- Yes, this is a perfect example of the Mark Twain quote, “There are lies. There are damn lies. And then there are statistics.”
- Yes, all the percentages reported in this study are based on relative risk and are, therefore, inflated. However, I do not have access to their data, so I cannot tell you the absolute risk associated with their other observations.
Blind Spots: In their paper the investigators recommended against the use of omega-3 supplements to prevent  heart disease because their data showed:
heart disease because their data showed:
- No benefit of omega-3 supplementation for preventing major cardiovascular events and deaths in a healthy population.
- But did suggest an increased risk of atrial fibrillation and stroke in that same population.
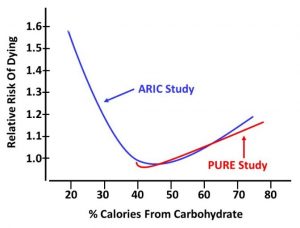
However, their blind spot was in underestimating the difficulty of showing the benefit of any intervention in a healthy population. The example I always use is statin drugs. Statin Drugs:
- Dramatically reduce the risk of a second heart attack and/or death in people who have already had a heart attack.
- Reduce the risk of heart attacks in people who are at high risk of heart attacks.
- Cannot be shown to reduce the risk of heart attacks in a healthy population.
This study suggests that omega-3 supplements are no different. In this study, omega-3 supplements:
- Reduced the risk of death in people who had already experienced a major cardiovascular event like a heart attack or stroke.
- Reduced the risk of major cardiovascular events and death in people with atrial fibrillation, which puts them at high risk for a heart attack or stroke.
- Could not be shown to reduce the risk of major cardiovascular events or deaths in a healthy population.
Hidden Data: There are some important data that were buried in the text and supplemental figures but were  ignored in the concluding remarks of this study and all the articles written about it. For example:
ignored in the concluding remarks of this study and all the articles written about it. For example:
- The original study and all articles written about the study reported that omega-3 supplementation increased the risk of stroke in otherwise healthy individuals but ignored the observation that omega-3 supplementation decreased the risk of heart failure in that same group.
The second example of hidden data likely represents another blind spot of the authors. They concluded that omega-3 supplementation had no benefit for healthy individuals without asking whether omega-3 supplements might benefit higher-risk subpopulations within this group. To help you understand this statement let me start by giving you some perspective.
As I said above, statin drugs cannot be shown to reduce the risk of heart attacks in a healthy population. But when you include people at high risk of heart disease with healthy people in the dataset, you start to see a reduced risk of heart attacks.
Similarly, with supplements you often see no benefits with the general population, which is what is usually reported in the media. But when you look at higher risk groups within that population, the benefits of supplementation emerge.
This study is no different:
- For healthy individuals, omega-3 supplementation had no effect on deaths during the 12-year follow-up period.
- However, omega-3 supplementation reduced the risk of death by 9% for both men and people ≥ 65. These represent two groups with elevated risk of heart disease within the otherwise healthy population.
- Once again, these data were completely ignored.
What Does This Study Mean For You?
 This study made 3 major points:
This study made 3 major points:
Point #1: Let me start with the one you’ve heard the most about. The risk of atrial fibrillation and stroke associated with omega-3 supplementation is real. We should not ignore it.
But what this study and most of the reports on the study didn’t tell you is that the risk is dose dependent. The risk is primarily seen with high doses of omega-3s. While no one has done a comprehensive dose response analysis, I can tell you that these side effects are:
- Seldom reported in clinical studies at doses of 1 gm/day or less.
- Sometimes reported in clinical studies at doses of ≥2 gm/day.
- Frequently reported in clinical studies at doses of ≥4 gm/day.
However, atrial fibrillation and stroke occur in a very small percentage of omega-3 users, even at 4 gm/day. At this point we have no idea why some people are susceptible to these side effects and others are not. More research in this area is clearly needed.
Until we know more about who is at risk, my recommendation for people who are trying to reduce the risk of heart disease is to rely on something called the Omega-3 Index to determine your individual omega-3 needs rather than using high-dose omega-3 supplements.
- The Omega-3 Index measures the amount of omega-3 fatty acids in your tissues. It is determined by the amount of omega-3s you consume and how you metabolize them, so it is individualized to you.
- An Omega-3 Index of 4% is associated with a high risk of heart disease, while an Omega-3 Index of 8% is associated with a low risk of heart disease. There is no evidence that more than 8% provides additional benefit.
- Most importantly, it only takes 1-1.6 gm/day of omega-3s to raise your Omega-3 Index from 4% to 8%. At these doses your risk of atrial fibrillation and stroke is extremely small.
For example, a recent meta-analysis of 29 studies with a total of 183,292 participants reported that people with an 8% Omega-3 Index had:
- Decreased risk of ischemic stroke (stroke due to blood clots) with no detectable increased risk of hemorrhagic stroke (stroke due to bleeding), and…
- No detectable increased risk of atrial fibrillation.
I recommend getting your Omega-3 Index determined, and if it is low, increasing your omega-3 intake to get it into the 8% range. Some people go from 4% to 8% more rapidly than others, so you may need to repeat the test several times to optimize your Omega-3 Index.
If your health professional doesn’t have access to the Omega-3 Index test, you can order it from https://omegaquant.com (I have no financial stake in this company, but I know it as a reputable source of the Omega-3 Index test).
Does The Professor Plan To Reduce His Intake Of Omega-3 Fatty Acids? Three weeks ago, I shared that my wife and I have been taking around 3 gm/day of omega-3 supplements for the past 40 years. Now that the association of atrial fibrillation and stroke with high dose omega-3 intake has been firmly established, some of you may be wondering whether we plan to decrease our intake of omega-3 supplements.
my wife and I have been taking around 3 gm/day of omega-3 supplements for the past 40 years. Now that the association of atrial fibrillation and stroke with high dose omega-3 intake has been firmly established, some of you may be wondering whether we plan to decrease our intake of omega-3 supplements.
The answer is, “No”. Remember that the increased risk of atrial fibrillation and stroke is only seen for a small subset of people taking high-dose omega-3 supplements. If we were part of that subset, we would likely have experienced one of those side effects by now.
However, if you are considering omega-3 supplementation for the first time, you don’t know whether you are part of that subset or not. So, my advice remains the same. Rely on optimizing your Omega-3 Index rather than high-dose omega-3 supplementation.
Point #2: Healthy individuals (those with no symptoms of heart disease) do not benefit from omega-3 supplementation. As I pointed out above, this ignores data from their study, namely.
- Omega-3 supplementation reduced the risk of heart failure in healthy subjects.
- Omega-3 supplementation reduced the risk of death in higher risk groups within the healthy population (namely men and people 65 and older).
 As I discussed above, this is a pattern seen with statin drugs and most nutritional supplements. Simply put, you can’t show any benefit of statin drugs or most nutritional supplements in a “healthy” population, but you can show benefit when you focus on higher risk individuals within the “healthy” population.
As I discussed above, this is a pattern seen with statin drugs and most nutritional supplements. Simply put, you can’t show any benefit of statin drugs or most nutritional supplements in a “healthy” population, but you can show benefit when you focus on higher risk individuals within the “healthy” population.
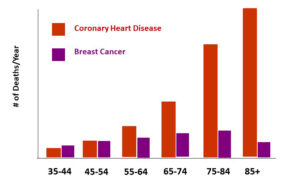
The problem, of course, is that most of us don’t really know whether we are “healthy” or not. For millions of Americans the first indication that they are at risk from heart disease is sudden death from a heart attack or stroke.
With that in mind, I will leave the decision about whether you want to supplement with omega-3s up to you. But if you decide to supplement, I recommend you optimize your Omega-3 Index rather than using a high dose omega-3 supplement.
Point #3: People with heart disease benefit from omega-3 supplementation. This recommendation is becoming non-controversial, so I won’t comment further other than to say high dose omega-3 supplements are probably not needed unless prescribed by your health professional.
The Bottom Line
You have been asking me about recent headlines saying that omega-3 supplements may increase rather than decrease the risk of heart disease. So, I analyzed the study behind the headlines. The study makes 3 claims:
- Omega-3 supplements increase the risk of atrial fibrillation and stroke when taken by healthy people.
- Omega-3 supplements are of no benefit for healthy individuals.
- Omega-3 supplements are beneficial for people who have heart disease.
In the article above I review the flaws, blind spots, and hidden data in the article and discuss what it means for you.
For more details about this study and what it means for you read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
______________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.