Lifestyle, Genetics, And Dementia Risk
Author: Dr. Stephen Chaney
 Alzheimer’s disease and other forms of dementia are among the most feared diseases of aging. What use is it to have a healthy body, a loving family, and a successful career if you can’t remember any of it? You should be able to enjoy your Golden years, not see them slip through your fingers.
Alzheimer’s disease and other forms of dementia are among the most feared diseases of aging. What use is it to have a healthy body, a loving family, and a successful career if you can’t remember any of it? You should be able to enjoy your Golden years, not see them slip through your fingers.
If you have a family history of dementia or have sent your DNA off for testing and learned you are genetically predisposed to dementia, you are probably worried.
Perhaps the scariest thing about Alzheimer’s is that the medical community has no answers. There are no drugs to prevent or cure Alzheimer’s and brain transplants are out of the question. Some medical professionals will tell you nothing can be done, but is that true?
Before I answer that question let me share a fictional story because it provides a clue. In 1997, when I was still a relatively young scientist, I saw a film called GAATACA. [If you are looking for an entertaining film to watch, it is  still available on some streaming services.]
still available on some streaming services.]
This film envisioned a future society in which parents had their sperm and eggs sequenced so that their children would be genetically perfect. In that society the term “love child” had been redefined as a child who had been conceived without prior DNA sequencing.
The hero of this film was, of course, a love child. He was born with a genetic predisposition for heart disease. He was considered inferior, a second-class citizen of this future world.
Without giving away the plot of the film (I don’t want to spoil the enjoyment for you if you are thinking of watching it), he overcame his genetic inferiority. With a strict regimen of diet and physical fitness he became stronger and healthier than many of his genetically perfect peers.
This is when I first began to realize that our genes do not have to determine our destiny. We have the power to overcome bad genetics. We also have the power to undermine good genetics.
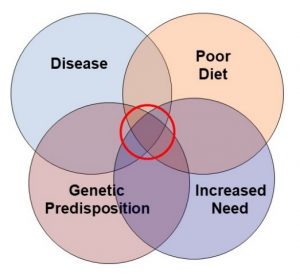
With that in mind, let’s return to Alzheimer’s. Studies have suggested that a healthy lifestyle can help reduce your risk of developing Alzheimer’s and other forms of dementia. But what about genetics? Will a healthy lifestyle only reduce your risk of dementia if your genetic risk is low, or will it be equally effective when your genetic risk is high? Can lifestyle overcome genetics?
The current study (A Tin et al, Neurology, 99: e154-e163, 2022) was designed to answer these questions.
How Was This Study Done?
 This study included 11,561 participants from the Atherosclerosis Risk In Communities (ARIC) study. The ARIC study recruited middle-aged adults (average age of 54) from both urban and rural areas of the United States and followed them for 26 years. The participants were 57% female and 53% white.
This study included 11,561 participants from the Atherosclerosis Risk In Communities (ARIC) study. The ARIC study recruited middle-aged adults (average age of 54) from both urban and rural areas of the United States and followed them for 26 years. The participants were 57% female and 53% white.
Simply put, the study was designed to look at the effect of a healthy lifestyle on the genetic risk of developing dementia.
A healthy lifestyle was defined based on something called “Life’s Simple 7” (LS7) score.
- The LS7 score was developed by the American Heart Association to define the effect of lifestyle on the risk of developing heart disease. However, it works equally well for defining the effect of lifestyle on risk of developing dementia.
- The LS7 score consists of 7 modifiable health factors.
-
- The factors are diet, physical activity, BMI (a measure of obesity), smoking, total cholesterol, blood pressure, and fasting blood glucose.
- The data for deriving the LS7 scores were derived from data gathered from each participant when they enrolled in the ARIC study.
-
- Diet was assessed by a 66-item food frequency questionnaire.
-
- Physical activity and smoking were assessed in separate questionnaires.
-
- BMI, blood pressure, total cholesterol, and fasting blood glucose were measured during a visit to a designated clinic at the beginning of the study.
- Each modifiable health factor was separated into 3 categories (ideal, intermediate, and poor) and the highest score was assigned to the ideal category. The LS7 score was the sum of the scores from all 7 modifiable health factors.
Genetic risk of developing dementia was defined based on something called “The Genetic Risk Score” (GRS).
- We have known for years that individuals of European descent who have the APOE ɛ4 gene variant have a 2 to 5-fold increased lifetime risk of developing dementia.
- In recent years scientists have discovered several additional gene variants that increase the risk of dementia.
- These have been combined with APOE ɛ4 to create a Genetic Risk Score for dementia.
- The Genetic Risk Score for each participant was determined by DNA sequencing at the beginning of the study, with the highest score indicating the greatest risk for developing dementia.
The onset and severity of dementia were determined based on 7 clinic visits during the study.
- Questionnaires were administered at each visit to assess self-reported dementia symptoms.
- Cognitive tests were administered at visits 2 and 4.
- Detailed cognitive and functional assessments were conducted at visits 5, 6, and 7.
- The data were reviewed by an expert committee of physicians and neuropsychologists to determine dementia status.
Lifestyle, Genetics, And Dementia Risk
 At the end of the 26-year study:
At the end of the 26-year study:
- When participants with the highest Genetic Risk Scores were compared to those with the lowest Genetic Risk Scores:
-
- European American participants were 2.7-fold more likely to develop dementia.
-
- African American participants were 1.55-fold more likely to develop dementia.
- When participants with the highest LS7 (healthy lifestyle) scores were compared to those with the lowest LS7 scores:
-
- European American participants were 40% less likely to develop dementia.
-
- African American participants were 17% less likely to develop dementia.
-
- A healthy lifestyle decreased the risk of developing dementia to a comparable extent at all levels of genetic risk for dementia.
The authors concluded, “Higher LS7 scores [a measure of a healthy lifestyle] are largely associated with a lower risk of incident dementia across strata of genetic risk [at all levels of genetic risk], supporting the use of LS7 [a healthy lifestyle] for maintaining brain health and offsetting genetic risk. More studies with larger study populations are needed…”
I should briefly comment on why African Americans were less responsive to both genetic risk and a healthy lifestyle than European Americans. The reasons for these discrepancies are not known, but:
- There are socioeconomic factors and health disparities that increase the risk of dementia that are not included in the LS7 score.
- A recent study has identified genetic risk factors for dementia that are unique to African Americans that are not included in the genetic risk score used in this study.
Can Lifestyle Overcome Bad Genes?
Dr. James Watson, who was co-discoverer of the DNA double helix and was heavily involved in the sequencing of the human genome, asked that he not be told about his risk of developing Alzheimer’s when his own DNA was sequenced in the early 2000’s. His reasoning was, “Why know the risk if you can’t change it?”
 If the study I discussed today is true, you can modify the risk. Your genes don’t have to be your destiny. But is it true?
If the study I discussed today is true, you can modify the risk. Your genes don’t have to be your destiny. But is it true?
There is good reason to believe it might be true. Multiple studies have shown that each of the health factors included in LS7 score reduce the risk of developing dementia. However, most of those studies have not looked at the interaction between a healthy lifestyle and genetic risk.
Fortunately, there is another recent study that looked at the interaction between a healthy lifestyle and genetic risk of developing dementia.
- This study used a different database (The UK Biobank study which enrolled 500,000 participants) and different criteria for defining a healthy lifestyle (diet, physical activity, smoking, and alcohol use).
However, the conclusions of this study were very similar:
- People at high genetic risk were almost twice as likely to develop dementia as those at low genetic risk.
- A healthy lifestyle decreased the risk of developing dementia by about 40% for both people at high genetic risk and for people at low genetic risk.
But this study went one step further than the study I discussed in this article. The British study reported that:
- People at low genetic risk and an unhealthy lifestyle (the typical American) were just as likely to develop dementia as people at high genetic risk and a healthy lifestyle.
In other words, bad genetics does not doom you to Alzheimer’s and dementia. A healthy lifestyle can cut your risk almost in half. Conversely, good genetics is not a “Get Out of Jail Free” card. You can squander the advantage of good genetics with an unhealthy lifestyle.
And, just like the hero of the movie I discuss at the beginning of this article, a healthy lifestyle may be able to overcome bad genes and make you just as healthy (with respect to the risk of developing dementia) as people with good genes and an unhealthy lifestyle – which includes most Americans.
The Bottom Line
Alzheimer’s disease and other forms of dementia are among the most feared diseases of aging. What use is it to have a healthy body, a loving family, and a successful career if you can’t remember any of it?
If you have a family history of dementia or have sent your DNA off for testing and learned you are genetically predisposed to dementia, you are probably worried.
Perhaps the scariest thing about Alzheimer’s is that the medical community has no answers. There are no drugs to prevent or cure Alzheimer’s and brain transplants are out of the question. Some medical professionals will tell you nothing can be done, but is that true?
Studies have suggested that a healthy lifestyle can help reduce your risk of developing Alzheimer’s and other forms of dementia. But what about genetics? Will a healthy lifestyle only reduce your risk of dementia if your genetic risk is low, or will it be equally effective when your genetic risk is high? Can lifestyle overcome genetics?
A recent study was designed to answer these questions. It found:
- When participants with the highest Genetic Risk Scores were compared to those with the lowest Genetic Risk Scores:
-
- They were 1.5 to 2.7-fold more likely to develop dementia.
- When participants with the highest LS7 (healthy lifestyle) scores were compared to those with the lowest LS7 scores:
-
- They were 17% to 40% less likely to develop dementia.
- A healthy lifestyle decreased the risk of developing dementia to a comparable extent at all levels of genetic risk for dementia.
The authors concluded, “Higher LS7 scores [a measure of a healthy lifestyle] are largely associated with a lower risk of incident dementia across strata of genetic risk [at all levels of genetic risk], supporting the use of LS7 [a healthy lifestyle] for maintaining brain health and offsetting genetic risk. More studies with larger study populations are needed…”
This, and other studies discussed in this issue of “Health Tips For The Professor” suggest that your genes don’t have to determine your destiny. You can overcome bad genes with a healthy lifestyle.
For more details on this study, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.