The Race To The Bottom Continues
Author: Dr. Stephen Chaney
 Big Food Inc is not your friend. Big Food Inc follows the latest trends and is only too happy to give consumers what they want.
Big Food Inc is not your friend. Big Food Inc follows the latest trends and is only too happy to give consumers what they want.
You want low-fat? No problem. You want low-carb, natural, organic, non-GMO, gluten-free, Paleo, Keto? No problem. However, their motive is a healthy bottom line, not your health.
They know humans are hardwired to desire sugar, salt, and fat. Foods with those ingredients sell. Convenience sells. At the end of the day, they are more interested in sales than they are in your health.
They don’t want you to buy whole foods and cook them from scratch. They don’t make money from whole foods. They want you to buy their pre-packaged convenience foods instead.
A prime example of how Big Food Inc of how Big Food takes a healthy food and turns it into a nutrition disaster is what I call “The Breakfast Cereal Scandal”.
The Breakfast Cereal Scandal
 It’s hard to believe that breakfast cereals started as health food, but they did. Dr. John Harvey Kellogg was a Seventh-day Adventist who took over the Western Reform Health Institute in 1877 and renamed it the Battle Creek Sanitarium.
It’s hard to believe that breakfast cereals started as health food, but they did. Dr. John Harvey Kellogg was a Seventh-day Adventist who took over the Western Reform Health Institute in 1877 and renamed it the Battle Creek Sanitarium.
It gained prominence as a health resort where people went to be healed through a combination of physical activity and healthy eating.
Dr. Kellogg invented Corn Flakes in 1878 as a healthier alternative to the high-fat breakfasts most Americans were consuming at that time. Corn Flakes had less than 5% sugar. It was a great idea for its time, but what happened next is nothing short of appalling.
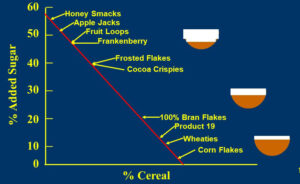
It is a perfect example of how Big Food Inc leads us astray. The graphic above that I created illustrates what the major food companies have done to breakfast cereals over the decades since then.
It all started with Corn Flakes. Then other food companies started bringing out competing products. Cereals like Wheaties and Rice Krispies were still pretty healthy, but they had a bit more sugar, which gave them better consumer appeal.
As soon as the food companies figured out that sugar increased their sales, the race was on. The percentage sugar increased to 40%, then to 50%, and now to almost 60%.
No sane parent would fill their child’s cereal bowl half full of sugar, but that is exactly what they are doing when they feed them some of today’s breakfast cereals. The food companies are hiding the outrageous sugar content of their cereals with slogans like “Just a touch of honey.”
Speaking of deception, can anyone tell me how you label a product with 20% sugar 100% Bran Flakes?
I created the graphic above in the 1990’s. At that time, I assumed breakfast cereals couldn’t get much worse. But I was wrong. Big Food’s “race to the bottom” continues.
A recent study (A Zhao et al, JAMA Network Open, 8(5): e2511699, 2025) examined the nutritional content of children’s cereals introduced to the US market between 2010 and 2023.
How Was This Study Done?
 The investigators used data from the Mintel Global New Products Database, which tracks new product launches for foods and beverages. From this database they identified 1,200 new children’s cereals introduced in the US market from 2010 through 2023.
The investigators used data from the Mintel Global New Products Database, which tracks new product launches for foods and beverages. From this database they identified 1,200 new children’s cereals introduced in the US market from 2010 through 2023.
Children’s cereals were defined as breakfast cereal products explicitly marketed (through packaging or branding) to children between 5 and 12 years old.
Using product label information, they compared the total fat, sodium, total carbohydrate, sugar, protein, and dietary fiber per serving and analyzed the trends between 2010 and 2023.
The Race To The Bottom Continues
![]() If the previous decline in nutritional value of breakfast cereals between the 1870s and 1970s can be described can be described as “appalling”, the latest results can only be described as disastrous.
If the previous decline in nutritional value of breakfast cereals between the 1870s and 1970s can be described can be described as “appalling”, the latest results can only be described as disastrous.
For newly introduced children’s breakfast cereals in the 13 years between 2010 and 2023,
- Fat content increased 34%.
- Sodium (salt) content increased 32%.
- Sugar content increased by 11%.
- Protein content decreased by 11%.
- Fiber content decreased by 30%.
The authors of the study concluded, “Analysis of newly launched children’s RTE (ready to eat) cereals from 2010 to 2023 revealed concerning nutritional shifts: notable increases in fat, sodium, and sugar along decreases in protein and fiber.
Children’s cereals contain high levels of added sugar, with a single serving exceeding 45% of the American Heart Association’s daily recommended limit for children.
These trends suggest a potential prioritization of taste over nutritional quality in product development, contributing to childhood obesity and long-term cardiovascular health risks.”
In short, despite the American public’s increasing interest in a healthy diet, Big Food is still prioritizing sales over healthy foods. The race to the bottom continues.
What Does This Mean For You?

The take home lesson is clear. Don’t trust Big Food with your health. Their priority is sales, not your health.
Even when they claim their processed foods are healthy because they have removed fat or sugar, they have simply replaced them with a witches brew of chemicals so they look, taste, and smell delicious.
And breakfast cereals are just the tip of the iceberg. For most Americans 60-70% of their diet comes from highly processed foods.
If you value health, the choice is clear. Choose whole, unprocessed food whenever possible.
The Bottom Line
The dramatic decline in the nutritional quality of breakfast cereals between the 1870s and 1970s is well documented. By the turn of the century most breakfast cereals had gotten so bad, you might assume they couldn’t get any worse. You would be wrong. Big Food’s race to the bottom continues.
A recent study evaluated the nutritional value of newly introduced children’s breakfast cereals between 2010 and 2023. In those 13 years,
- Fat content increased 34%.
- Sodium (salt) content increased 32%.
- Sugar content increased by 11%.
- Protein content decreased by 11%.
- Fiber content decreased by 30%.
The authors of the study said, “These trends suggest a potential prioritization of taste over nutritional quality in product development, contributing to childhood obesity and long-term cardiovascular health risks.”
I agree. And this is just the tip of the iceberg. For most Americans 60-70% of their diet comes from highly processed foods.
If you value health, the choice is clear. Choose whole, unprocessed food whenever possible.
For more details on this study and what it means for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
_________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
___________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 53 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.