Can You Achieve Permanent Weight Loss?
Author: Dr. Stephen Chaney
 Why is the dreaded yo-yo rearing its ugly head again? You tried a new diet this year, and it worked really well. The weight came off easily. But the diet is over, and the pounds are starting to creep up once again.
Why is the dreaded yo-yo rearing its ugly head again? You tried a new diet this year, and it worked really well. The weight came off easily. But the diet is over, and the pounds are starting to creep up once again.
You are beginning to wonder if this diet was just like all the other yo-yo diets you’ve tried in the past. You are wondering whether those pounds you lost will come back and bring their friends with them. If so, you’ll be like 156 million Americans who lose weight and gain it all back each year.
And it’s so frustrating. You are trying to be good. You are still exercising and trying to eat healthily. Why isn’t it working?
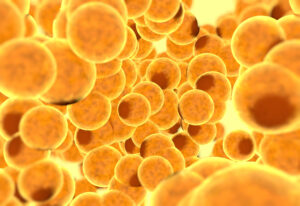
Could it be that your fat cells have a memory? Could it be they like to be big and bulky with lots of stored fat? While that description is a bit fanciful, a new study (LC Hinte et al, Nature Online, 2024) suggests your fat cells may have a memory, which could explain why it is so hard to keep the weight off.
This is a highly technical study. So, before I discuss how the study was done, I should perhaps review a little bit of Biochemistry 101.
Biochemistry101: Epigenetics and Gene Activity
 What Is Epigenetics? When I was a young graduate student (which is more than just a few years ago), I was taught that all genetic information resided in our DNA. During conception, we picked up some DNA from our dad and some from our mom, and that DNA was what made us a unique individual.
What Is Epigenetics? When I was a young graduate student (which is more than just a few years ago), I was taught that all genetic information resided in our DNA. During conception, we picked up some DNA from our dad and some from our mom, and that DNA was what made us a unique individual.
In recent years, the hype has centered on DNA sequencing. It seems like everyone is offering to sequence your genome and tell you what kind of diet is best for you, what foods to eat, and what supplements to take. But can DNA sequencing fulfill those promises?
The problem is that DNA sequencing only tells you what genes you have. It doesn’t tell you whether those genes are active. Simply put, it doesn’t tell you whether those genes are turned on or turned off.
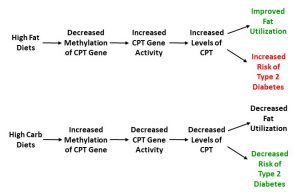
This is where epigenetics comes in. Epigenetics is the science of modifications that alter gene expression. In simple terms, both DNA and the proteins that bind to DNA can be modified. This does not change the DNA sequence. But these modifications can determine whether a gene is active (turned on) or inactive (turned off).
This sounds simple enough, but here is where it really gets interesting. These modifications are affected by our diet, our lifestyle (body weight and exercise, for example), our microbiome (gut bacteria), and our environment.
And if that weren’t complicated enough, some of these epigenetic changes (DNA modifications) can be transitory and others are long-lasting.
The authors of this study hypothesized that obesity causes long-lasting epigenetic changes to certain critical genes in our fat cells that slow metabolism and promote fat accumulation, even after we have lost weight. In other words, these epigenetic changes “prime” our fat cells to regain all the weight we’ve lost.
How Do You Measure the Effect of Epigenetic Changes? As you might expect this study measured epigenetic modifications to critical genes in fat cells. But that’s only part of the story. Epigenetic modification can turn genes on, turn them off, or have no effect on gene activity.
So, the investigators also needed to monitor the activity of the genes to determine the effect of the epigenetic modifications. Fortunately, one fact you may have learned in high school or college biology is mostly unchanged by the passage of time.
It is that the genetic sequence of DNA is translated into messenger RNA and that messenger RNA is used to code for proteins. If epigenetic modifications turned on a gene, we would expect higher levels of the corresponding messenger RNA and corresponding protein in those cells. Conversely, if epigenetic modifications turned off a gene, we would expect the opposite.
It turns out that it is much easier to measure changes in messenger RNA levels than individual protein levels that correspond to specific genes. So, the investigators used cellular messenger levels to measure the effect of epigenetic modifications on gene activity.
How Was This Study Done?
 The investigators measured the effect of obesity and subsequent weight loss on fat cell gene expression in a limited set of human subjects and supplemented those results with a more expansive set of experiments with mice.
The investigators measured the effect of obesity and subsequent weight loss on fat cell gene expression in a limited set of human subjects and supplemented those results with a more expansive set of experiments with mice.
I don’t normally report on animal studies or very small human studies because these studies often lead to misleading results that are not supported by subsequent long-term, large clinical studies.
However, I am making an exception for this study because it leads to an interesting paradigm shift which, if true, changes the way we think about how to keep weight off long term.
Human Study: The investigators determined messenger RNA levels for key genes in fat cells from human volunteers who were:
- At a healthy weight.
- Obese both before and 2 years after bariatric surgery that resulted in at least 25% weight loss.
The groups were small (10-16 total), in part because obtaining fat cell samples is an invasive and painful procedure.
Mouse study: The investigators determined both messenger RNA levels and epigenic modifications for key genes in fat cells from 6-week-old male mice who were:
- Fed either a low-fat or high-fat chow diet for 25 weeks. As expected, the mice fed the low-fat diet remained lean and the mice fed the high-fat diet became obese.
- Subsequently, the obese mice were put on low-fat chow for 8 weeks during which time their weight returned to normal.
- Finally, both the ‘always lean’ and ‘formerly obese’ mice were put on high-fat chow to compare how rapidly they gained weight.
What Happens To Fat Cells During Obesity And Weight Loss?
 This study is best viewed as a story of what happens to fat cells during obesity and subsequent weight loss. There are two parts – what happens to human fat cells and what happens to mouse fat cells:
This study is best viewed as a story of what happens to fat cells during obesity and subsequent weight loss. There are two parts – what happens to human fat cells and what happens to mouse fat cells:
Human Fat Cells: When obese individuals were compared to lean individuals:
- Genes coding for fat storage and inflammation (which is known to be associated with obesity) were more active.
- Fat-burning genes were less active.
- These changes in gene expression were retained even after the obese individuals lost substantial weight through bariatric surgery.
[Note: The measurements of gene expression were based on the amount of messenger RNA produced by those genes.]
The human study had a couple of important limitations, which is why the investigators also did a similar study with mice.
#1: Because the study did not include a habitually lean group who became obese after going on a high-fat diet (no clinical review board would approve such a study), it could not determine whether the differences in gene expression were caused by the onset of obesity or whether they caused obesity.
Simply put, we know some individuals are genetically predisposed to obesity. The differences in gene expression between lean and obese individuals could have simply represented a genetic predisposition to obesity.
The mouse experiments did not suffer from that limitation because it was possible to put lean mice on a high fat diet until they became obese.
#2: The study did not measure epigenetic changes that may have caused the changes in gene expression. That is because humans are genetically heterogeneous. Consequently, you need population studies with hundreds of individuals to reliably determine epigenetic differences between groups.
The mouse experiments did not suffer from that limitation because laboratory mice are genetically homogeneous.
Mouse Fat Cells:
 When the investigators looked at the physical effects of obesity:
When the investigators looked at the physical effects of obesity:
- When mice became obese on a high-fat diet:
-
- Blood glucose levels rose.
-
- Insulin levels rose, indicating the mice had become insulin resistant.
-
- Fat accumulated in their livers.
- When the obese mice lost the excess weight on a low-fat diet all these parameters returned to normal.
- When the ‘always lean’ and ‘previously obese’ mice were put back on a high fat diet at the end of the study, the previously obese mice gained weight more quickly than the always lean mice.
In other words, mice responded to obesity in the same way that humans do except none of these effects could be explained by genetics. This strain of mice was genetically homogeneous.
When the investigators compared gene expression (as measured by messenger RNA levels) in mice who had become obese to ‘always lean’ mice:
- Genes coding for fat storage and inflammation were more active.
- Fat-burning genes were less active.
- These changes in gene expression were retained even after the obese mice lost weight.
In other words, mice responded to obesity in the same ways as humans with respect to gene expression. However, in this case it was clear that obesity caused the changes in gene expression.
When the investigators looked at epigenetic modifications:
- They identified epigenetic modifications to the regulatory regions of genes whose activity was increased or decreased when the mice became obese.
- These epigenetic modifications were retained even after the mice lost weight.
These data suggest, but do not prove, that the epigenetic modifications were responsible for the changes in gene activity.
The authors concluded, “We show that both human and mouse adipose tissues retain transcriptional changes after appreciable weight loss.
Furthermore, we find persistent obesity induced alterations in the epigenome of mouse adipocytes that negatively affect their function and response to metabolic stimuli. Mice carrying this obesogenic memory show accelerated rebound weight gain…in response to high-fat diet feeding.
In summary, our findings indicate the existence of an obesogenic memory, largely on the basis of stable epigenetic changes, in mouse adipocytes and probably other cell types. These changes seem to prime cells for pathological response [weight gain] in an obesogenic environment, contributing to the problematic ‘yo-yo’ effect often seen with dieting.”
More simply put, the investigators concluded that obesity causes epigenetic modifications to the DNA of fat cells that prime them to regain their fat stores. They said that this may contribute to the ‘yo-yo’ effect often seen with dieting and explain why keeping weight off is so hard.
Why Is Keeping Weight Off So Hard?
 You are not alone. You are like millions of other Americans. You lose weight effectively, but you struggle to keep it off. You just look at a donut and the fat jumps from the donut to your hips. You try to eat right, but the pounds keep creeping back on.
You are not alone. You are like millions of other Americans. You lose weight effectively, but you struggle to keep it off. You just look at a donut and the fat jumps from the donut to your hips. You try to eat right, but the pounds keep creeping back on.
Experts have told us for years that our fat cells (and perhaps other cells in our body) are the culprit. Those cells have switched from a fat burning mode to a fat storage mode. There have been lots of attempts to explain that phenomenon, but my favorite is one that hypothesizes that our metabolism was designed for paleolithic times when it was either feast or famine.
Simply put, the theory is that our bodies were designed to store energy reserves in times of plenty and hold on to those energy reserves as long as possible in times of famine. Holding on to energy reserves was essential for prehistoric man to survive cold winters when food was hard to come by. And our number one energy reserve is, you guessed it, fat.
That is an appealing hypothesis, but it doesn’t tell us how our bodies manage to do that.
That’s what makes this study so intriguing. It may be wrong. It needs to be substantiated by large scale clinical trials. But the idea that epigenic changes occur during obesity and persist after substantial weight loss is novel. More importantly, it may explain the “feast or famine” response and why it is so hard to keep weight off after substantial weight loss.
Can You Achieve Permanent Weight Loss?
By now you may be thinking, “I thought my weight loss woes were due to my genetics. Now you’re telling me that they could be due to my epigenetics. Am I doubly cursed? Is there nothing I can do to keep my weight off?”
I can tell you science doesn’t have a simple answer, but there are two big clues that offer hope.
 #1: Slow and steady wins the race. Obesity experts have known for years that slow weight loss often results in permanent weight loss.
#1: Slow and steady wins the race. Obesity experts have known for years that slow weight loss often results in permanent weight loss.
- If you are counting calories, that means a reduction of around 500 calories per week (That’s 71 calories per day, which is equivalent to one small apple, one hard-boiled egg, or 1.5 ounces of chicken breast). And a 500-calorie deficit maintained each week for a year can lead to a 20-25 pound weight loss.
- If you are thinking of diets, it could amount to switching to a diet of unprocessed or minimally processed foods consisting of fruits, vegetables, whole grains, and primarily plant-based proteins without worrying about calories or serving sizes. Again, clinical studies show that switching from the typical American diet to this kind of diet can lead to substantial weight loss over a period of years.
Neither approach is popular in the weight loss world, but they work. Why do they work? It could be because the daily reduction in calories is so small that it never triggers the famine response.
If we look at the two parts of the study I reported on above:
- In the human study weight loss was achieved through bariatric surgery which causes a huge reduction in caloric intake and rapid weight loss.
- In the mouse study going from high-fat chow to low-fat chow represented a large decrease in calories. And again, weight loss was very rapid. It took the mice 25 weeks to become obese and only 4-8 weeks to lose the weight they had gained.
When viewed from this perspective, the epigenetic modifications observed after weight loss in this study may have been due to the famine response rather than a retention of the modifications observed during obesity.
And when you think about it, most popular diets feature major restrictions (calories, fats, carbs, forbidden foods, time of eating) and cause rapid weight loss. They are likely to trigger a famine response as well.
 #2: The secrets of the National Weight Control Registry. There are some people who manage to keep their weight off and avoid the yo-yo effect. They don’t have any genetic or epigenetic advantage over the rest of us. They have lost weight on every diet imaginable – including rapid weight loss fad diets.
#2: The secrets of the National Weight Control Registry. There are some people who manage to keep their weight off and avoid the yo-yo effect. They don’t have any genetic or epigenetic advantage over the rest of us. They have lost weight on every diet imaginable – including rapid weight loss fad diets.
Yet they have managed to keep the weight off. What are their secrets? How did they avoid regaining their weight? How did they avoid the yo-yo diet effect?
An organization called the National Weight Control Registry was established to answer that question. It has enrolled more than 10,000 people who have lost weight and kept it off. On average people in this group have lost 66 pounds and kept it off for at least 5 years.
The National Weight Control Registry kept track of what they did to keep the weight off. Everyone’s approach was a little different, but the National Weight Control Registry summarized the ones that were most frequently mentioned. Here is what they do that you may not be doing:
#1: They consume a reduced calorie, whole food diet.
#2: They get lots of exercise (around 1 hour/day).
#3: They have internalized their eating patterns. In short, this is no longer a diet. It has become a permanent part of their lifestyle. This is the way they eat without even thinking about it.
#4: They monitor their weight regularly. When they gain a few pounds, they modify their diet until they are back at their target weight.
#5: They eat breakfast on a regular basis.
#6: They watch less than 10 hours of TV/week.
#7: They are consistent (no planned cheat days).
The good news is that participants in the National Weight Control Registry reported that while maintaining weight loss was difficult at first, it became easy after 2 years.
Of course, we don’t know whether is due to epigenic modifications being reset to “lean” by these behaviors or whether the new behaviors became automatic and overrode epigenetics.
It doesn’t matter. It means you can end the ‘yo-yo’ cycle forever. You can keep weight off, and you know how to do it.
The Bottom Line
A recent study in both humans and mice suggests that epigenetic modifications to key genes in your fat cells make it hard to keep weight off. These epigenetic changes may explain why so many people struggle with yo-yo dieting.
For more details on this study and how you may be able to override these epigenetic modifications and prevent weight regain read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
_____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.