The Influence Of Genetics And Diet On Type 2 Diabetes
Author: Dr. Stephen Chaney
 Does it ever feel like you have drawn the short straw?
Does it ever feel like you have drawn the short straw?
Everyone in your family has succumbed to heart disease, diabetes, or cancer at a young age. Are you doomed to the same fate?
You ordered a DNA test. It sounded like fun. But when the gene report came back it said you had a “bad” genetic profile. You were told you are at high risk of diabetes, heart attack, stroke, cancer, or dementia. Are you doomed to a short and sickly life?
In both cases, you are probably wondering, “Is there anything I can do to improve my odds of a healthy life? What if I lost some of those extra pounds, exercised more, and ate a healthier diet? Would that make a difference?”
The study (J Merino et al, PLoS Medicine 19(4): e1003972, April 26, 2022) I will describe today was designed to answer these questions.
But before I describe the study, I should probably cover what I call Genetics 101: “How Genes Affect Your Health”.
Genetics 101: How Genes Affect Your Health
 If you studied genetics in school, you probably learned about diseases like sickle cell anemia, which is caused by a single mutation in a single gene. If you get two copies of the “bad” gene, you will have sickle cell anemia. If you get one copy of the “bad” gene and one copy of the normal gene, you have sickle cell trait, which is much less severe.
If you studied genetics in school, you probably learned about diseases like sickle cell anemia, which is caused by a single mutation in a single gene. If you get two copies of the “bad” gene, you will have sickle cell anemia. If you get one copy of the “bad” gene and one copy of the normal gene, you have sickle cell trait, which is much less severe.
Simply put, you either have the disease or you don’t. It’s dependent on your genetics, and you can’t do much about it.
If you know someone who has been treated for breast cancer, you are probably familiar with a more complex relationship between genetics and health. There are several “bad” genes that increase the risk of breast cancer. And knowing which gene is involved is important for selecting the best treatment regimen.
But most of the diseases that shorten our lives (like diabetes, heart disease, most cancers, and dementia) are what we call polygenetic diseases. Simply put, that means that there are dozens of genes that increase the risk of these diseases. Each gene makes a small contribution to the increased risk. So, we can only measure the genetic contribution to these diseases by measuring hundreds of mutations in dozens of genes, something called a polygenetic risk score.
The study I will be describing today looked at the relative effect of genetics (measured as the type 2 diabetes polygenic risk score) and diet quality (measured as the Alternative Healthy Eating Index (AHEI)) on the risk of developing type 2 diabetes.
How Was This Study Done?
 The data for this study were obtained from 3 long-term clinical studies conducted in the United States – the Nurses’ Health Study (121,700 participants), the Nurses’ Health Study II (116,340 participants), and the Health Professionals Follow-Up Study (51,529 participants).
The data for this study were obtained from 3 long-term clinical studies conducted in the United States – the Nurses’ Health Study (121,700 participants), the Nurses’ Health Study II (116,340 participants), and the Health Professionals Follow-Up Study (51,529 participants).
These studies measured lifestyle factors (including diet) every 4 years and correlated them with disease outcomes over 20+ years.
The study I will be discussing today was performed with 35,759 participants in these 3 studies for whom DNA sequencing data was available.
- The DNA sequence data were used to generate a type 2 diabetes polygenic risk score for each participant in this study.
- Food frequency questionnaires obtained every 4 years in these studies were used to calculate the Alternative Healthy Eating Index (AHEI) score for each participant.
-
- The AHEI is based on higher intake of fruits, whole grains, vegetables, nuts and legumes, polyunsaturated fatty acids, long-chain omega-3 fatty acids, moderate intake of alcohol, and lower intake of red and processed meats, sugar sweetened drinks and fruit juice, sodium, and trans-fat).
The investigators used these measurements to estimate the relative effect of genetics and diet quality on the risk of developing type 2 diabetes.
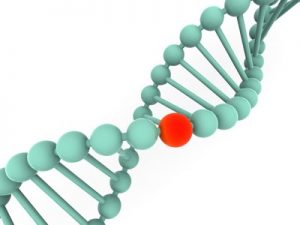
The Influence Of Genetics And Diet On Type 2 Diabetes
 The participants were divided into low, intermediate, and high genetic risk based on their type 2 diabetes polygenic risk score.
The participants were divided into low, intermediate, and high genetic risk based on their type 2 diabetes polygenic risk score.
Compared with low genetic risk:
- Intermediate genetic risk increased the risk of developing type 2 diabetes by 26%.
- High genetic risk increased the risk of developing type 2 diabetes by 75%.
Put another way, each 1 standard deviation increase in the polygenetic risk score:
- Increased the risk of developing type 2 diabetes by 42%.
Simply put, bad genes can significantly increase your risk of developing type 2 diabetes. That’s the bad news. But that doesn’t mean you should think, “Diabetes is in my genes. There is nothing I can do.”
The investigators also divided the participants into those who had a high-quality diet, those who had an intermediate quality diet, and those who had a low-quality diet based on their AHEI (Alternative Healthy Eating Index) score.
Finally, they divided the participants into groups depending on their BMI, a measure of obesity.
Compared to an obese person consuming a low-quality diet, a lean person consuming a high-quality diet:
- Reduced their risk of developing type 2 diabetes by around 43% for each category of genetic risk.
- More specifically, a lean person consuming a high-quality diet reduced their risk of developing type 2 diabetes:
-
- By 41% if they were at low genetic risk.
-
- By 50% if they were at intermediate genetic risk.
-
- By 38% if they were at high genetic risk.
The investigators then made a statistical adjustment to remove BMI from their calculations, so they could focus on  the effect of diet alone on the risk of developing type 2 diabetes.
the effect of diet alone on the risk of developing type 2 diabetes.
Compared to a low-quality diet, a high-quality diet:
- Reduced the risk of developing type 2 diabetes by around 33% for each category of genetic risk.
- More specifically, a high-quality diet reduced the risk of developing type 2 diabetes:
-
- By 31% for those at low genetic risk.
-
- By 39% for those at intermediate genetic risk.
-
- By 29% for those at high genetic risk.
Looking at it another way:
- When people at high genetic risk consumed a high-quality diet, their risk of developing type 2 diabetes was only 13% higher than people at intermediate genetic risk who consumed a low-quality diet (such as the typical American diet).
- When people at intermediate genetic risk consumed a high-quality diet, their risk of developing type 2 diabetes was 5% less than people at low genetic risk who consumed a low-quality diet.
Simply put:
- If you are at intermediate genetic risk, a high-quality diet may completely reverse your risk of developing type 2 diabetes.
- If you are at high genetic risk, a high-quality diet can partially reverse your risk of developing type 2 diabetes.
In short, the good news is that bad genes do not doom you to type 2 diabetes.
- The investigators did not provide similar information for the effect of an ideal weight on the risk of developing type 2 diabetes, but it is likely that the combination of diet plus weight management would result in an even more significant reduction in risk of developing type 2 diabetes for individuals in the even the highest risk category.
The authors concluded, “These data provide evidence for the independent associations of genetic risk and diet quality with incident type 2 diabetes and suggest that a healthy diet is associated with lower diabetes risk across all levels of genetic risk.”
Do Bad Genes Doom You To Bad Health?
 At the beginning of this article I posed the question, “Do bad genes doom you to bad health?”
At the beginning of this article I posed the question, “Do bad genes doom you to bad health?”
Based on this study, the good news is that bad genes don’t doom you type 2 diabetes. And just because most of your relatives are diabetic doesn’t mean that must be your fate.
- This study shows that a healthy diet significantly reduces your risk of developing type 2 diabetes at every genetic risk level.
- And the study suggests that a healthy diet plus a healthy weight is even more beneficial at reducing your risk of type 2 diabetes.
- While not included in this study, other studies have shown that exercise also plays a role in reducing type 2 diabetes risk.
None of this information is new. What is new is that a healthy diet is equally beneficial at reducing type 2 diabetes risk even in individuals with a high genetic risk of developing the disease. Simply put, you can reverse the effects of bad genes.
“And what is this magic diet?”, you might ask. In this study, it was based on AHEI score. Someone with a high AHEI score consumes:
- Lots of fruits, whole grains, vegetables, nuts and legumes, polyunsaturated fatty acids, and long-chain omega-3 fatty acids.
- Moderate or no amounts of alcohol.
- Little or no red and processed meats, sugar sweetened drinks, fruit juices, sodium, and foods with trans-fat.
Any whole food, primarily plant-based diet from vegan to Mediterranean or DASH fits the bill.
Finally, while this study focused just on type 2 diabetes, other studies have come to similar conclusions for other diseases.
Should You Get Your DNA Tested?
If you are looking for guidance on how to reduce your risks, the answer is, “No”. In this study, the same diet and lifestyle changes lowered the risk of type diabetes at every genetic risk level. Despite what some charlatans may tell you, there is no special diet or magic potion for people with a high genetic risk for developing type 2 diabetes.
If you are looking for motivation, the answer may be, “Yes”. If knowing you are at high risk makes it more likely that you will make the diet and lifestyle changes needed to lower your risk of type 2 diabetes, a DNA test may be just what you need
The Bottom Line
If a serious disease runs in your family or if you have had your DNA tested and found out you are at high risk for some disease, you are probably wondering whether there is anything you can do or whether your bad genes have doomed you to a short and sickly life.
A recent study answered that question for type 2 diabetes. It showed a healthy diet significantly reduces the risk of type 2 diabetes even in people at high genetic risk of developing the disease.
Other studies have come to similar conclusions for other diseases. In short, bad genes don’t doom you to bad health.
For more details about the study and what it means for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
_____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.