Why Do Clinical Studies Disagree?
Author: Dr. Stephen Chaney

Six weeks ago, the title of my “Health Tips From the Professor” article was, “Are Omega-3 Supplements Safe?” That’s because I was reviewing a study that claimed long-term use of omega-3 supplements increased the risk of atrial fibrillation and stroke. And it had led to headlines like, “Omega-3 Supplements May Increase the Risk of Heart Disease” and “Fish Oil Supplements May Increase The Risk of Stroke and Heart Conditions”.
This week, the title of my article is, “Omega-3 Supplements Are Safe”. I did not choose this title to express my opinion, although I am in general agreement with the statement. I chose that title because the omega-3 pendulum has swung again. The article (M Javaid et al, Journal of The American Heart Association, Volume 13, Number 10: e032390, 2024) I am reviewing today came to the conclusion that omega-3 supplements don’t increase the risk of stroke.
I understand your confusion. You are wondering how scientists can tell you one thing today and the total opposite tomorrow. It is conflicting results like this that cause the public to lose faith in science. And when people lose faith in science they are easily influenced by “snake oil” charlatans on the internet.
So, after I describe this study, I will discuss why scientific studies come up with conflicting results and compare these two studies in detail. That is probably the most important part of this article.
How Was This Study Done?
 Scientists from Freeman Hospital and Newcastle University in the UK conducted a meta-analysis combining the data from 120,643 patients enrolled in 11 clinical trials that evaluated the effects of omega-3 supplementation. The inclusion criteria for this meta-analysis were as follows:
Scientists from Freeman Hospital and Newcastle University in the UK conducted a meta-analysis combining the data from 120,643 patients enrolled in 11 clinical trials that evaluated the effects of omega-3 supplementation. The inclusion criteria for this meta-analysis were as follows:
- The studies were randomized trials that compared omega-3 supplements with placebo or standard treatment. Half the patients received the omega-3 supplement.
- The patients were either previously diagnosed with heart disease or were at high risk of developing heart disease.
- The studies reported the incidence of bleeding events.
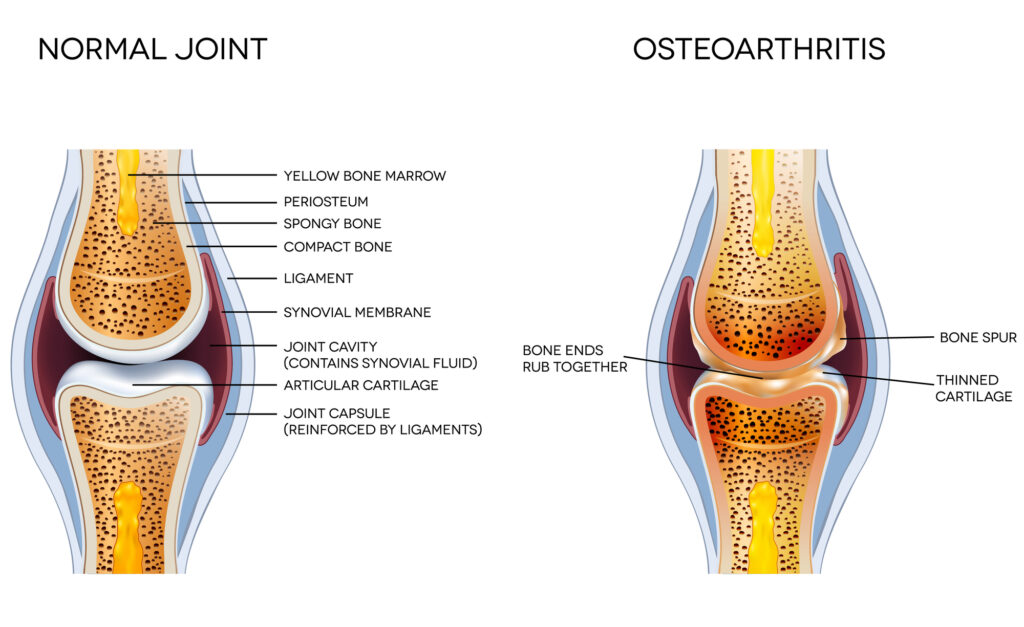
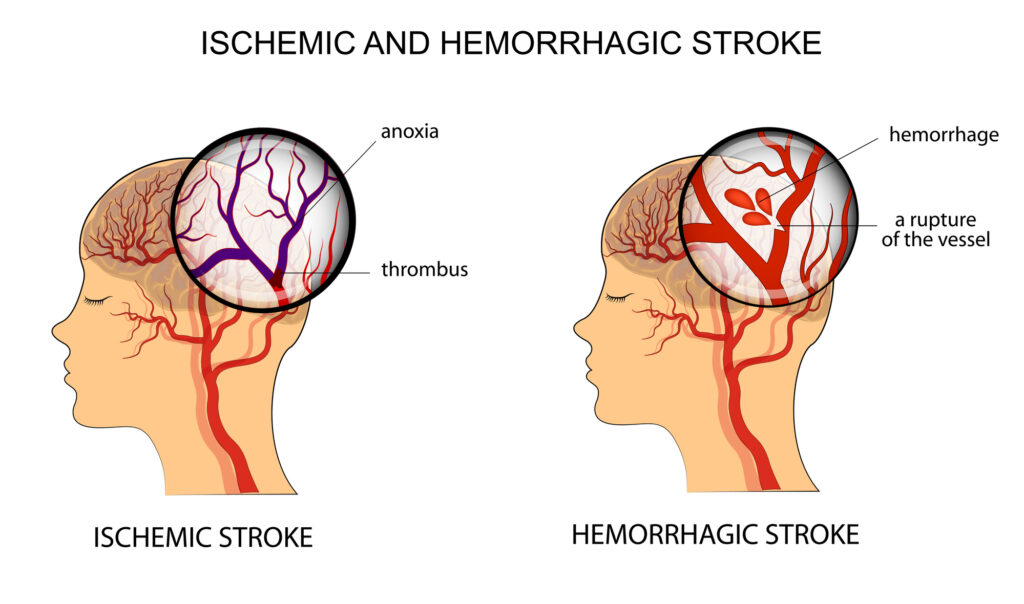
The study asked whether omega-3 supplementation increased the risk of bleeding events (defined as hemorrhagic stroke, intracranial bleeding, or gastrointestinal bleeding) compared to a placebo or standard treatment.
Omega-3 Supplements Are Safe
 The results were reassuring for omega-3 supplement users. When compared to a placebo or standard treatment, omega-3 supplements.
The results were reassuring for omega-3 supplement users. When compared to a placebo or standard treatment, omega-3 supplements.
- Did not increase the risk of overall bleeding events.
- Did not increase the risk of hemorrhagic stroke, intracranial bleeding, or gastrointestinal bleeding.
- Did not increase the risk of bleeding in patients who were also taking blood thinners (Blood thinners reduce the ability of blood to clot and can lead to bleeding events. This study found that adding omega-3 supplements to these drugs did not increase bleeding risk.
But here is where it gets interesting. One of the 11 studies included in the meta-analysis used a high dose (4 grams/day) of Vascepa, a highly purified ethyl ester of EPA produced by the pharmaceutical company Amarin. When the authors analyzed the data from this study alone, they found that Vascepa:
- Increased the relative risk of bleeding by 50% compared to the control group.
-
- While this sounds scary, the absolute risk of bleeding was only increased by 0.6% compared to the control group.
-
- I will explain the difference between relative risk and absolute risk below. But for now, you can think of absolute risk as a much more accurate estimate of your actual risk.
The authors of the meta-analysis speculated that the increased bleeding risk associated with the use of Vascepa could be due to the:
- High dose of EPA (4 gm/day) or…
- Lack of DHA and other naturally occurring omega-3s in the formulation. The authors said:
-
- The effect of DHA on the endothelial lining is weaker than that of EPA (EPA makes the endothelial lining “less sticky” which reduces its ability to trigger blood clot formation. This is one of the mechanisms by which EPA is thought to decrease blood clot formation.)
-
- The ability of DHA to inhibit oxidation of Apo-B-containing particles was less sustained than that of EPA (Oxidized Apo-B-containing particles increase the risk of blood clot formation. Inhibition of that oxidation by EPA is another of the mechanisms by which EPA is thought to decrease blood clot formation.)
The authors concluded, “Omega-3 PUFAs [polyunsaturated fatty acids] were not associated with increased bleeding risk. Patients receiving high-dose purified EPA [Vascepa] may incur additional bleeding risk, although its clinical significance is very modest.”
What Is The Difference Between Relative And Absolute Risk?
 Relative risk is best defined as the percentage increase or decrease in risk compared to the risk found in a control group. Absolute risk, on the other hand, is the actual increase or decrease in risk in the group receiving the intervention.
Relative risk is best defined as the percentage increase or decrease in risk compared to the risk found in a control group. Absolute risk, on the other hand, is the actual increase or decrease in risk in the group receiving the intervention.
Relative risk is an excellent tool for identifying risks. However, it magnifies the extent of the risk, so it can be misleading. For example,
- If the absolute risk of some event occurring in the general population was 40%, a 50% increase in relative risk would increase the absolute risk by 20% (40% X 0.5 = 20%) to give a total risk of 60% (40% + 20%). In this case, both the relative and absolute risk are significantly large numbers.
- However, if the absolute risk in the general population was 1%, a 50% increase in relative risk would only increase the absolute risk to 1.5%, a 0.5% increase in absolute risk. In this case, the increase in relative risk appears significant, but it is misleading because the absolute increase in risk is a modest 0.5%.
- The latter resembles the situation in this study when the authors compared bleeding events in patients receiving Vascepa to those receiving a placebo. The absolute risk of bleeding events in the control group was 1.2%. The risk of bleeding events in the Vascepa group was 1.8%. That is a 50% increase in relative risk but only a 0.6% increase in absolute risk.
Why Do Clinical Studies Disagree?
 As I have said many times before, there is no perfect clinical study. Every study has its strengths and its flaws. So, it is perhaps instructive to compare this study and the previous study I reviewed 6 weeks ago. Here are some of the questions I ask when evaluating the strengths and weaknesses of clinical studies.
As I have said many times before, there is no perfect clinical study. Every study has its strengths and its flaws. So, it is perhaps instructive to compare this study and the previous study I reviewed 6 weeks ago. Here are some of the questions I ask when evaluating the strengths and weaknesses of clinical studies.
#1: What kind of study is it?
- The previous study was an association study. It can only report on associations. It cannot determine cause and effect. Outcomes like atrial fibrillation and strokes could have been caused by unrelated variables in the population studied.
- The current study was a meta-analysis of 11 randomized controlled clinical trials. Because the only difference between the two groups is that one received omega-3 supplements, it can determine cause and effect.
#2: How many people were in the study?
- Both studies were very large, so this was not a factor.
#3: How long was the study?
- The previous study lasted 12 years. The clinical trials within this meta-analysis lasted one to five years. This is a slight advantage for the previous study because it might be better able to detect risks of chronic use of omega-3 supplements.
#4: How were participants selected?
- Participants in the previous study had no previous diagnosis of heart disease while participants in the current study either had a previous diagnosis of heart disease or were at high risk of developing heart disease.
This difference would be relevant if both studies were looking at the benefits of omega-3 supplements. However, the current study was only looking at the side effects of omega-3 supplements, so this is not an important consideration.
 #5: How was omega-3 intake monitored?
#5: How was omega-3 intake monitored?
- This was a significant flaw of the previous study. Use of omega-3 supplements was determined by a questionnaire administered when the subjects entered the study. No effort was made to determine whether the amount of omega-3s consumed remained constant during the 12-year study.
- The clinical studies within the current meta-analysis were comparing intake of omega-3 supplements to placebo and monitored the use of the omega-3 supplements throughout the study.
#6: What is the dose-response?
- This was another serious flaw of the previous study. There was no dose-response data.
- The current study provided limited dose-response data. From the data they presented it appeared that the risk of bleeding events was only slightly dose-dependent except for the clinical study with the high dose (4 gm/day) EPA-only Vascepa drug. It was a clear outlier, which is why they analyzed the data from that study independently from the other studies.
#7: What outcomes were measured?
- The only common outcome measured in the two studies was hemorrhagic stroke.
- The previous study reported that omega-3 supplementation increased the risk of stroke by 5% in the general population. However:
-
- That result just barely reached statistical significance.
-
- It was a 5% increase in relative risk. The authors did not report absolute risk.
-
- It was an association study, so it could not determine cause and effect.
- The current study found omega-3 supplementation had no effect on the risk of stroke in a population that either had heart disease or were at high risk of heart disease.
-
- The exception, of course, was the group taking the high dose Vascepa drug (see below).
 #8: Was the risk clinically significant?
#8: Was the risk clinically significant?
- As I said above, the previous study only reported relative risk, which can be misleading. However, absolute risk can be calculated from their data. For example,
-
- The risk of developing atrial fibrillation in the group taking omega-3 supplements was 4.4% (calculated from Table 2 of the manuscript). The authors said that represented a 13% increase in relative risk compared to the group not taking omega-3 supplements. This means the absolute (actual) increase in risk is about 0.6%.
-
- The risk of stroke in the group taking omega-3 supplements was 1.5% (calculated from Table 2 of the manuscript). The authors said that represented a 5% increase in relative risk compared to the group not taking omega-3 supplements. This means the absolute (actual) increase in risk is about 0.08%.
- In the current study the increased risk of stroke in the group taking the high-dose (4 gm/day) EPA-only Vascepa drug was 50% for relative risk, but only 0.6% for absolute risk.
-
- The authors of the current study argued that, based on absolute risk, the risk of stroke for people taking Vascepa was “clinically insignificant”. I would argue the same is true for the results reported in the previous study and the headlines they generated.
#9: Who sponsored the study?
- The previous study was supported by the Bill and Melinda Gates Foundation, an organization that has no obvious interest in the outcome of the study.
- The current study is sponsored by Amarin, the pharmaceutical company that manufactures and markets Vascepa.
-
- However, to their credit, the authors made no effort to hide the negative data about Vascepa.
-
-
- In fact, they highlighted the negative data, noted that the increased bleeding risk with Vascepa was different from the omega-3 supplements studied, and offered possible explanations for why a high potency, EPA-only supplement might increase the risk of bleeding more than a lower potency omega-3 supplement containing both EPA and DHA.
-
-
- They did, however, choose to emphasize the 0.6% absolute increase in bleeding risk rather than the 50% relative increase in bleeding risk. However, as I noted above absolute risk is a more accurate way to report risk, especially when the risk in the control group is only 1.2%.
Perspective On This Comparison:
 You may be tempted to conclude that the previous study was garbage. Before you do, let me provide some perspective.
You may be tempted to conclude that the previous study was garbage. Before you do, let me provide some perspective.
- The data for that study came from the UK Biobank, which is a long-term collection of data by the British government from over 500,000 residents in the United Kingdom. The data are made available to any researcher who wants to study links between genetic and environmental exposure to the development of disease. However, the data were not collected with any particular study in mind.
This is why omega-3 intake was only determined at the beginning of the study and there was no dose-response information included. The experimental design would have been different if the study were specifically designed to measure the influence of omega-3 supplementation on health outcomes. However, because of cost, the sample size would have been much smaller, which would have made it difficult to show any statistically significant results.
- Relative risk rather than absolute risk is almost universally used to describe the results of clinical studies because it is a larger number and draws more attention. However, as I described above, relative risk can be misleading. In my opinion, both relative and absolute risk should be listed in every publication.
What Does This Study Mean For You?
 Scientists know that every study has their flaws, so we don’t base our recommendations on one or two studies. Instead, we look at the totality of data before making recommendations. When looking at the totality of data two things stand out.
Scientists know that every study has their flaws, so we don’t base our recommendations on one or two studies. Instead, we look at the totality of data before making recommendations. When looking at the totality of data two things stand out.
- The bleeding risk with Vascepa is not unique. There are some studies suggesting that high dose (3-4 gm/day) omega-3 supplements containing both EPA and DHA may increase bleeding risk, although probably not to the same extent as Vascepa.
- An optimal Omega-3 Index of 8% is associated with a decreased risk of heart disease and does not appear to increase the risk of atrial fibrillation or bleeding events such as hemorrhagic stroke. And for most people, an 8% Omega-3 Index can be achieved with only 1-2 gm/day of omega-3s.
So, my recommendations are the same as they were 6 weeks ago.
- Be aware that high-dose (3-4 gm/day) of omega-3 supplements may cause an increased risk of atrial fibrillation and stroke, but the risk is extremely small.
- Omega-3 supplementation in the 1-2 gm/day range appears to be both safe and effective.
- I recommend getting your Omega-3 Index determined, and if it is low, increasing your omega-3 intake to get it into the 8% range.
The Bottom Line
A recent meta-analysis concluded that omega-3 supplementation does not increase the risk of bleeding events, including hemorrhagic stroke, intracranial bleeding, and gastrointestinal bleeding.
The exception was the high-dose (4 gm/day), EPA-only drug Vascepa, which increases bleeding risk from 1.2% to 1.8%, a 0.6% increase in absolute risk.
This study contradicts a previous study I shared with you only six weeks ago, so I made a detailed comparison of the strengths and weaknesses of each study.
For more details on these studies and what they mean for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
_____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
 Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.