Why Is Folate Needed For Strong Bones?
Author: Dr. Stephen Chaney
 When most people think of the nutrients required to build strong bones, they just think of calcium and vitamin D. This is understandable because these two nutrients are essential for building healthy bone.
When most people think of the nutrients required to build strong bones, they just think of calcium and vitamin D. This is understandable because these two nutrients are essential for building healthy bone.
But in reality “it takes a village” to build strong bones.
- The bone matrix also contains magnesium, zinc, copper, and manganese. They are also needed.
-
- Fun fact: As an undergraduate at the University of Southern California my wife, Suzanne, worked for Dr. Paul Saltman, the biochemist who discovered the importance of these nutrients for building healthy bone.
- Vitamin C is required to build collagen, the foundation on which bone is built, and the cartilage that helps bones resist fractures.
- Vitamin K delivers calcium to osteoblasts, the cells responsible for building bone.
But a new study (L Zhou et al, BMC Musculoskeletal Disorders, 25: 487, pages 1-9, 2024) suggests that folate is also important for building strong bones and preventing osteoporosis as we age. I didn’t see that one coming. So, let me start by explaining why folate may be important for bone health before I review the study.
Why Is Folate Needed For Strong Bones?
 There are four facts we need to know about human metabolism to understand the effect of folate on bone health.
There are four facts we need to know about human metabolism to understand the effect of folate on bone health.
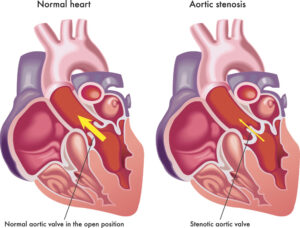
Fact 1: We tend to think of bone as a permanent, unchanging part of our body. But that’s not true. As we move about our bones experience wear and tear. As they age they become more brittle and susceptible to fracturing.
So, our bodies have a process for continuously removing old bone and replacing it with new bone. Although you don’t notice the change, your bones today are not the same bones you had 10 or 15 years ago. They are continually being renewed.
The cells responsible for removing the old bone are called osteoclasts, and the cells responsible for building new bone are called osteoblasts. It is the perfect balance between osteoclast and osteoblast activity that keeps our bones strong.
Fact 2: When cellular folate levels are low, an amino acid metabolite called homocysteine accumulates in our cells and in our blood.
Fact 3: (This is the one I didn’t know until I looked it up): Homocysteine increases osteoclast activity and decreases osteoblast activity.
This tips the balance towards breaking down our bones. For young people that makes it more difficult to build strong, healthy bones. For older people that increases the risk of osteoporosis.
Fact 4: To clear up any confusion before we get started, I should tell you that the term “dietary folates” often includes folates from foods and folic acid from supplements. That is because folic acid is efficiently taken up by our cells and converted to folates in the cell.
And when methyl folate and folic acid are compared head to head in clinical studies, methyl folate offers no advantage over folic acid, even in individuals with mutations in the MTHFR gene. For more detail on this statement, go to https://www.chaneyhealth.com/healthtips/ and type “methy folate” in the search box.
How Was The Study Done?
 The investigators used data from the CDC’s 2017-2020 NHANES (National Health And Nutrition Examination Survey) database. The NHANES program has been obtaining health and nutrition data from approximately 5,000 US citizens a year since 1969. Every 4 years the data are compiled into a database that can be used for studies like this one.
The investigators used data from the CDC’s 2017-2020 NHANES (National Health And Nutrition Examination Survey) database. The NHANES program has been obtaining health and nutrition data from approximately 5,000 US citizens a year since 1969. Every 4 years the data are compiled into a database that can be used for studies like this one.
The investigators excluded participants who were missing important information such as calcium, vitamin D, or folate intake and bone density measurements. This left 2297 participants for the current study.
The participants were 49.9% female, 73% white, and the average age was 64 years. The prevalence of osteoporosis in this group was 6.92%, which is similar to other estimates of osteoporosis prevalence in this age group.
Dietary intake was based on two 24-hour dietary recalls. Bone density in the femur region was assessed by DXA radiological imaging. Osteoporosis was defined as a bone mineral density of <0.64 g/cm2 for women and <0.68 g/cm2 for men.
The study measured the correlation between dietary folate intake and prevalence of osteoporosis.
Is Folate Needed For Strong Bones?
 The investigators separated the participants into 3 groups based on dietary folate intake: lowest (<264 mcg/day), middle (264-390 mcg/day), and highest (>390 mcg/day). For reference the daily value (DV) for folate is 400 mcg/day for adults in this age group.
The investigators separated the participants into 3 groups based on dietary folate intake: lowest (<264 mcg/day), middle (264-390 mcg/day), and highest (>390 mcg/day). For reference the daily value (DV) for folate is 400 mcg/day for adults in this age group.
When adjusted for other factors that affect bone density such as calcium, vitamin D, smoking, and alcohol consumption, those with the highest dietary intake of folates compared to those with the lowest dietary intake of folates:
- Decreased their risk of osteoporosis by 70%.
And when the data were broken down by gender and age, the highest intake of dietary folates:
- Decreased the risk of osteoporosis by 82% for women.
-
- Also, decreased the risk of osteoporosis for men. But the decrease was not statistically significant (Because men are less likely to develop osteoporosis than women, a much larger study would likely be required to show a statistically significant decreased risk for men.)
- Decreased the risk of osteoporosis by 70% for people over 60.
-
- Did not significantly decrease the risk of osteoporosis for people under 60 (Osteoporosis is rare in people under 60.)
- In short, adequate intake of folates (including folic acid) significantly decreases the risk of osteoporosis for those who are at highest risk, namely postmenopausal women over 60.
When the investigators did a dose response plot they found an L-shaped relationship between dietary folate and the risk of osteoporosis. They concluded that:
- Dietary folate intake between 264 and 569 mcg/day was effective in preventing osteoporosis in post-menopausal women. Intakes above 569 mcg/day provided little or no additional benefit.
The authors concluded, “This finding suggests the potential importance of dietary folate for preventing and managing osteoporosis.”
“However, further longitudinal research and randomized controlled trials are necessary to elucidate the causal association between dietary folate intake and the risk of osteoporosis.”
What Does This Study Mean For You?
 I am not suggesting that you should throw out your calcium and vitamin D supplement and rely on a folic acid supplement to build strong bones and prevent osteoporosis.
I am not suggesting that you should throw out your calcium and vitamin D supplement and rely on a folic acid supplement to build strong bones and prevent osteoporosis.
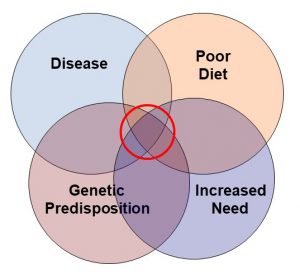
Calcium and vitamin D are absolutely essential for building strong bones. But they are not sufficient by themselves. It takes a holistic approach to build strong bones.
I have previously alerted you to the importance of vitamin C, vitamin K, magnesium, zinc, copper, and manganese for building strong bones. This study suggests I may need to add folic acid to the list. And who knows how many additional nutrients may play a role we don’t yet know about.
And it’s not just nutrients. There are many other lifestyle factors that influence the health of our bones. I have described what it takes to have a “bone healthy lifestyle” in a previous issue of “Health Tips From the Professor”.
This is why so many studies looking at the effect of calcium/vitamin D supplements on the risk of developing osteoporosis have come up empty. These studies were asking if calcium and vitamin D were “magic bullets” that could prevent osteoporosis on their own.
The answer to that question appears to be, “No”. But it isn’t the right question. As I have said before, “When clinical studies ask the wrong question, they get the wrong answer.”
Calcium and vitamin D are essential for bone formation, but they aren’t sufficient by themselves. It takes a village. Any study that ignores that is doomed to failure.
What does that mean for you? My recommendation is simple. If you want to build strong bones and reduce your risk of osteoporosis:
- Start with a comprehensive multivitamin/multimineral supplement to make sure your bases are covered.
- If your intake of calcium and vitamin D are below DV values (1,300 mg of calcium and 600-800 IU of vitamin D for adults in this age range), consider a calcium/vitamin D supplement.
- Follow a “bone healthy lifestyle”.
The Bottom Line
A recent study suggests that dietary folate is important for building strong bones and preventing osteoporosis in post-menopausal women.
In this article I review the study, put it into perspective, and discuss what it means for you.
For more details about this study and what it means for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
______________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
____________________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.