What Does Increase Breast Cancer Risk?
Author: Dr. Stephen Chaney
 It seems like every time you turn around there are new headlines warning us that a particular food or supplement increases your risk of cancer. If you believe all those headlines, there would be little you could eat. You might starve to death trying to avoid eating anything that increases your risk of cancer.
It seems like every time you turn around there are new headlines warning us that a particular food or supplement increases your risk of cancer. If you believe all those headlines, there would be little you could eat. You might starve to death trying to avoid eating anything that increases your risk of cancer.
So, it’s important to ask which of those warnings are true and which are just myths.
For example, a few days ago, a friend called me and said, “I just heard that resveratrol is estrogenic and causes breast cancer. Should I read the labels of the herbal supplements I take and avoid anything with resveratrol in it.”
I assured her that this was just a myth. The likelihood that resveratrol and related polyphenols cause breast cancer is very low. And if she was concerned about breast cancer, there were much more important things to worry about.
But as I started to explain why it was a myth, I realized the explanation was complex. I was able to explain it to my friend in a 20-minute discussion. But it was then I realized I needed to write a “Health Tips From the Professor” article to help explain it to the general public.
Why Are We Concerned?
 You might be asking, “Why is this such a big deal? Why do we care if something has estrogenic properties?” Let me start at the beginning.
You might be asking, “Why is this such a big deal? Why do we care if something has estrogenic properties?” Let me start at the beginning.
When I first started teaching medical students in 1972, hormone replacement therapy (a combination of estrogen and progesterone) was thought to be a safe and effective treatment for menopausal symptoms and post-menopausal bone loss, and it was very widely prescribed.
That practice came to a screeching halt in 2002 when the Woman’s Health Initiative study showed that it increased the risk of breast, endometrial, and ovarian cancer. Today,
- The hormone composition of hormone replacement therapy has been changed.
- It is only prescribed for severe menopausal symptoms. And drugs are the treatment of choice to reduce post-menopausal bone loss.
- It is prescribed for the shortest possible time to limit exposure.
These simple changes in hormone replacement therapy represent the single most important intervention for reducing breast cancer risk in the past 50 years. Yes, you heard that right. These changes were more effective than any other medication or preventative strategy for reducing the number of women developing and dying from breast cancer.
This lesson made a big impression on the medical community. So, it is easy to understand why anything resembling estrogen is immediately suspected of increasing the risk of breast cancer. But the reality is far more complicated. So, it’s time for another of my “Biochemistry 101” segments.
Biochemistry 101: What Does Estrogenic Mean?
 Let’s start at the beginning with what polyphenols are. They comprise a diverse group of compounds with these common features.
Let’s start at the beginning with what polyphenols are. They comprise a diverse group of compounds with these common features.
- If you look at their structures, they contain multiple rings (A chemist would tell you they have more than one phenol group, hence the term polyphenol. But that terminology is only useful if you are a chemist).
- They are found in plants. Specifically, they are found in fruits, vegetables, herbs, spices and beverages (coffee, tea, and cocoa, for example).
- They have antioxidant properties.
Types of polyphenols include flavonoids, phenolic acids, lignans, and stilbenes. I mention this only because soy isoflavones, which I will talk about later, are flavonoids.
Some of these compounds have structures that resemble estrogen. If they bind to estrogen receptors and have the same effect as estrogen in cultured human cells, they are said to have “estrogenic properties”.
That’s why you see blogs warning about foods and herbal ingredients we should avoid because of their “estrogenic” properties. Some of these blogs are written by people with “Dr” on front of their name. But they aren’t biochemists and don’t know what biochemists know.
Let’s dig a little deeper. Here are some of the complexities that most bloggers either don’t know about or ignore.
- There is more than one kind of estrogen receptor.
- Different estrogen receptors have different effects in the cell. For example, some estrogen receptors activate pathways that increase cancer risk. Other receptors activate pathways that decrease cancer risk.
- The same estrogen receptor can have different effects in different cell types. That’s why estrogen replacement therapy reduced menopausal symptoms and post-menopausal bone loss AND increased cancer risk in other tissues.
The Estrogenic Myth
 A couple of weeks ago I talked about “The Soy Myth”, specifically the myth that soy isoflavones increase breast cancer risk. Of course, that myth was based on the observation that soy isoflavones have estrogenic properties and a simplistic interpretation of what that means. But in fact, soy isoflavones:
A couple of weeks ago I talked about “The Soy Myth”, specifically the myth that soy isoflavones increase breast cancer risk. Of course, that myth was based on the observation that soy isoflavones have estrogenic properties and a simplistic interpretation of what that means. But in fact, soy isoflavones:
- Are found naturally in most soy foods unless they are highly processed.
- Bind strongly to the estrogen receptors that decrease cancer risk.
- Bind weakly to the estrogen receptors that increase breast cancer risk.
In contrast, estrogen:
- Binds strongly to the estrogen receptors that increase breast cancer risk.
- Binds weakly to the estrogen receptors that decrease breast cancer risk.
- Soy isoflavones compete with estrogen for binding to the receptors that increase breast cancer risks. This helps protect breast cells from the cancer-promoting effects of estrogen.
So, it is true that soy isoflavones bind to estrogen receptors, but on the balance, you would predict that soy isoflavones decrease, rather than increase breast cancer risk.
The key word here is “predict” breast cancer risk. If you are a woman, you don’t want a prediction, you want to know one way or the other.
That’s why multiple human clinical studies have been conducted to determine the effect of soy foods on breast cancer risk. As I told you two weeks ago:
- Some studies showed no effect of soy consumption on the risk of getting breast cancer or breast cancer recurrence if you have previously had breast cancer.
- Other studies found that soy consumption reduced the risk of breast cancer occurrence and recurrence.
- No studies found that soy consumption increased the risk of breast cancer occurrence or recurrence.
So, for soy the answers are clear.
- Yes, soy isoflavones have estrogenic properties.
- No, soy consumption is not associated with an increased risk of breast cancer. That is a myth.
 The situation with resveratrol is similar:
The situation with resveratrol is similar:
- It is found naturally in grapes and many other fruits.
- It has estrogenic properties.
- Cell culture experiments show that it activates pathways that reduce cancer risk.
- Animal studies predominantly show that it reduces cancer risk. The only exceptions are a few animal studies with very high doses of resveratrol.
- The few clinical studies that have been done show that it either has no effect on breast cancer risk or reduces cancer risk.
- No human clinical trials have shown that resveratrol increases cancer risk.
The take home lesson is clear. Knowing that a food or herbal ingredient has estrogenic properties is meaningless unless you have data from human clinical trials on cancer outcomes.
So, the next time you see headlines telling you that you should avoid a food or herbal ingredient because it has “estrogenic properties” treat them skeptically. Unless the claim is backed up by human clinical trials showing an increased cancer risk, the claim is probably a myth.
What Does Increase Breast Cancer Risk?
 The take home lesson is clear. If you are concerned about your risk of breast cancer or any other form of cancer you should ignore the social media posts, podcasts, and blogs about the cancer risks of estrogenic foods and herbal ingredients.
The take home lesson is clear. If you are concerned about your risk of breast cancer or any other form of cancer you should ignore the social media posts, podcasts, and blogs about the cancer risks of estrogenic foods and herbal ingredients.
Unless they are backed by human clinical trials showing they increase cancer risks, the claims are likely to be mythical rather than real.
If they have any effect on cancer risk, it is likely to be small. Instead, focus on the important risk factors.
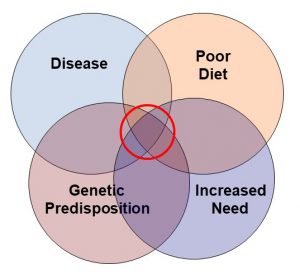
According to the American Cancer Society, the top 5 risk factor for breast cancer, and most other cancers, are:
#1: Overweight and obesity. The American Cancer Society recommends that you get and stay at a healthy weight.
Let me put this in perspective for you. Even if things like soy and resveratrol increased your risk of breast cancer, their effect is very small compared to estrogen and you are only exposed to them briefly once or twice a day.
In contrast, fat cells produce estrogen, and if you are overweight, fat cells accumulate in your breasts. Those fat cells are bathing your breast cells in a bath of pure estrogen 24/7.
#2: Inactivity. The American Cancer Society recommends that adults get at least 150 to 300 minutes of moderate intensity or 75 to 150 minutes of vigorous intensity activity each week (or a combination of these), preferably spread throughout the week.
#3: Alcohol use. The American Cancer Society says it is best not to drink alcohol at all. For women who do drink, they should have no more than 1 alcoholic drink a day.
#4: Hormone use after menopause. The American Cancer Society recommends talking to your health care provider about non-hormonal options to treat menopausal symptoms.
#5: Poor diet. The American Cancer Society recommends a diet low in fat, processed and red meat, and sugary drinks, but high in fruits and vegetables.
The Bottom Line
It seems like every day you hear about another food or supplement you should avoid because it has “estrogenic properties” and is likely to cause cancer. I call this the estrogenic myth because those claims are generally mythological rather than factual. In this article:
- I discuss why these claims are myths rather than facts using soy isoflavones and resveratrol as examples.
- Tell you what the American Cancer Society tells you to focus on if you want to decrease your risk of breast cancer and other cancers.
For more details on these studies and what they mean for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_____________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading Biochemistry textbooks for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading Biochemistry textbooks for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 53 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.