Why Is There So Much Confusion About Soy?
Author: Dr. Stephen Chaney
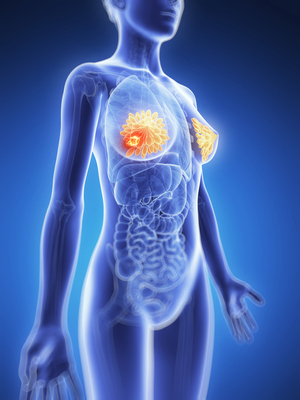
 What is the truth about soy and breast cancer? Does it increase the risk of breast cancer, or is that just a myth? If you are a woman, particularly a woman with breast cancer, it is an important question.
What is the truth about soy and breast cancer? Does it increase the risk of breast cancer, or is that just a myth? If you are a woman, particularly a woman with breast cancer, it is an important question.
Some experts say soy should be avoided at all costs. They say that soy will increase your risk of breast cancer. Other experts say soy is perfectly safe and may even reduce your risk of breast cancer. Who is right?
If you are a breast cancer survivor, the question of whether soy increases or decreases your risk of disease recurrence is even more crucial. You have already endured surgery, chemotherapy, and/or radiation. You never want to go through that again.
Why Is There So Much Confusion About Soy?
 Soy isoflavones decrease estrogen production, strengthen the immune system, inhibit cell proliferation, and reduce the production of reactive oxygen species. These are all effects that might reduce breast cancer risk.
Soy isoflavones decrease estrogen production, strengthen the immune system, inhibit cell proliferation, and reduce the production of reactive oxygen species. These are all effects that might reduce breast cancer risk.
On the other hand, soy isoflavones also bind to estrogen receptors and exhibit weak estrogenic activity. This effect has the potential to increase breast cancer risk.
Cell culture and animal studies have only confused the issue. Soy isoflavones stimulate the growth of breast cancer cells in a petri dish. Soy isoflavones also stimulate breast cancer growth in a special strain of mice lacking an immune system. However, in studies in both mice and rats with a functioning immune system, soy isoflavones decrease breast cancer risk.
The confusion has been amplified by claims and counterclaims on the internet. There are bloggers who are more interested in the spectacular than they are in accuracy (Today we call this fake news). They have taken the very weak evidence that soy isoflavones could possibly increase breast cancer risk and have blown it all out of proportion.
Their blogs claim that soy definitely increases breast cancer risk and should be avoided at all costs. Their claims have been picked up by other web sites and blogs. Eventually, the claims have been repeated so many times that people started to believe them. A “myth” has been created. I call it a myth because it was never based on convincing scientific evidence.
In the meantime, scientists looked at the cell culture and animal studies and took a more responsible approach. They said “If this is true, it is an important public health issue. We need to do clinical trials in humans to test this hypothesis.”
What Have Previous Clinical Studies Shown?
 The question of whether soy consumption increased the risk of developing breast cancer was settled a long time ago. Some studies have shown no effect of soy consumption on breast cancer risk. Others have reported that soy consumption decreased breast cancer risk. A meta-analysis of 18 previous clinical studies found that soy slightly decreased the risk of developing breast cancer (J Natl Cancer Inst, 98: 459-471, 2006). None of those studies found any evidence that soy increased the risk of breast cancer.
The question of whether soy consumption increased the risk of developing breast cancer was settled a long time ago. Some studies have shown no effect of soy consumption on breast cancer risk. Others have reported that soy consumption decreased breast cancer risk. A meta-analysis of 18 previous clinical studies found that soy slightly decreased the risk of developing breast cancer (J Natl Cancer Inst, 98: 459-471, 2006). None of those studies found any evidence that soy increased the risk of breast cancer.
What about recurrence of breast cancer in women who are breast cancer survivors? There have been five major clinical studies looking at the effects of soy consumption on breast cancer recurrence in both Chinese and American populations. Once again, the studies have shown either no effect of soy on breast cancer recurrence or a protective effect. None of them have shown any detrimental effects of soy consumption for breast cancer survivors.
A meta-analysis of all 5 studies was published in 2013 (Chi et al, Asian Pac J Cancer Prev., 14: 2407-2412, 2013). This study combined the data from 11,206 breast cancer survivors in the US and China. Those with the highest soy consumption had a 23% decrease in recurrence and a 15% decrease in mortality from breast cancer.
What Did The Most Recent Study Show?
 In earlier clinical studies the protective effect of soy has been greater in Asian populations than in North American populations. This could have been because Asians consume more soy. However, it could be due to other population differences as well.
In earlier clinical studies the protective effect of soy has been greater in Asian populations than in North American populations. This could have been because Asians consume more soy. However, it could be due to other population differences as well.
To better evaluate the effect of soy consumption on breast cancer survivors in the North America, a group of investigators correlated soy consumption with all-cause mortality in breast cancer survivors in the US and Canada (Zhang et al, Cancer, DOI: 10.1002/cncr.30615, March 2017).
The data were collected from The Breast Cancer Family Registry, an international research infrastructure established in 1995. The women enrolled in this registry either have been recently diagnosed with breast cancer or have a family history of breast cancer.
This study included 6235 breast cancer survivors from the registry who lived in the San Francisco Bay area and the province of Ontario in Canada. The women represented an ethnically diverse population and had a median age of 51.8 at enrollment. Soy consumption was assessed either at the time of enrollment or immediately following breast cancer diagnosis. The women were followed for 9.4 years, during which time 1224 of them died.
The results were as follows:
- There was a 21% decrease in all-cause mortality for women who had the highest soy consumption compared to those with the lowest soy consumption.
- The protective effect of soy was strongest for those women who had receptor negative breast cancer. This is significant because receptor-negative breast cancer is associated with poorer survival rates than hormone receptor-positive cases.
- The protective effect was also greatest (35% reduction in all-cause mortality) for women with the highest soy consumption following breast cancer diagnosis. This suggests that soy may play an important role in breast cancer survival.
- The authors concluded “In this large, ethnically diverse cohort of women with breast cancer, higher dietary intake of [soy] was associated with reduced total mortality.”
In an accompanying editorial, Omer Kucuk, MD, of the Winship Cancer Institute of Emory University, noted that the United States is the number 1 soy producer in the world and is in a great position to initiate changes in health policy by encouraging soy intake. He said “We now have evidence that soy foods not only prevent breast cancer but also benefit women who have had breast cancer. Therefore, we can recommend women to consume soy foods because of soy’s many health benefits.”
The Soy Myth
 Every clinical study has its limitations. If there were only one or two studies, the question of whether soy increases breast cancer risk might still be in doubt. However, multiple clinical studies have come to the same conclusion. Either soy has no effect on breast cancer risk and breast cancer recurrence, or it has a protective effect.
Every clinical study has its limitations. If there were only one or two studies, the question of whether soy increases breast cancer risk might still be in doubt. However, multiple clinical studies have come to the same conclusion. Either soy has no effect on breast cancer risk and breast cancer recurrence, or it has a protective effect.
Not a single clinical study has found any evidence that soy increases breast cancer risk. It is clear that consumption of soy foods is safe, and may be beneficial, for women with breast cancer. The myth that soy increases breast cancer risk needs to be put to rest.
On the other hand, we should not think of soy as a miracle food. Breast cancer risk is also decreased by a diet that:
- Contains lots of fruits and vegetables.
- Is low in processed grains & sweets and high in whole grains.
- Is low in saturated & trans fats and high in omega-3 and monounsaturated fats.
- Is low in red & processed meats and high in beans, fish & chicken.
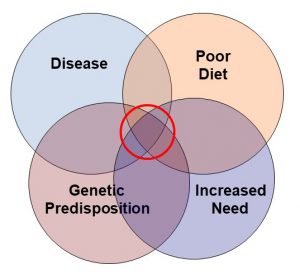
Furthermore, diet is just one component of a holistic approach for reducing the risk of breast cancer. In addition to a healthy diet, the American Cancer Society recommends that you:
- Control your weight
- Be physically active
- Limit alcohol
- Don’t smoke
- Limit hormone replacement therapy unless absolutely necessary.
- Reduce stress
The Bottom Line
1) It is time to put the myth that soy increases breast cancer risk to rest. This myth is based on cell culture and animal studies, and those studies were inconclusive.
2) Multiple clinical studies have shown that soy either has no effect on breast cancer risk, or that it reduces the risk.
3) Multiple clinical studies have also shown that soy either has no effect on breast cancer recurrence in women who are breast cancer survivors, or that it reduces recurrence.
4) The most recent clinical study is fully consistent with previous studies. It reports:
- There was a 21% decrease in all-cause mortality for women who had the highest soy consumption compared to those with the lowest soy consumption.
- The protective effect of soy was strongest for those women who had receptor negative breast cancer. This is significant because receptor-negative breast cancer is associated with poorer survival rates than hormone receptor-positive cases.
- The protective effect was also greatest (35% reduction in all-cause mortality) for women with the highest soy consumption following breast cancer diagnosis. This suggests that soy may play an important role in breast cancer survival.
- No clinical studies have provided any evidence to support the claim that soy increases either breast cancer risk or breast cancer recurrence.
For more information on this study and other things you can do to reduce the risk of breast cancer read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
______________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading Biochemistry textbooks for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading Biochemistry textbooks for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 53 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.