What Did This Study Get Wrong?
Author: Dr. Stephen Chaney
 “Killer calcium” is back. Once again, we are seeing headlines saying that calcium supplementation increases our risk of dying from heart disease. If you have seen these headlines, you are probably confused.
“Killer calcium” is back. Once again, we are seeing headlines saying that calcium supplementation increases our risk of dying from heart disease. If you have seen these headlines, you are probably confused.
After all, there have been three major clinical studies looking at the effect of calcium supplementation on heart disease risk. These studies followed close to 100,000 Americans for 10-20 years. And none of the studies found any increase in the risk of developing or dying from heart disease for people taking calcium supplements. For more information on this topic, see an article from “Health Tips From the Professor”.
You are probably wondering, “What is going on? I thought this issue was settled”.
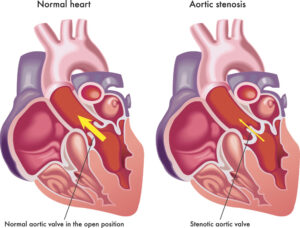
In the first place, this study did not look at heart disease in general, but on a very specific form of heart valve disease called aortic stenosis. Aortic stenosis is a narrowing of the heart valve leading to the aorta. And it is often associated with calcification of the heart valve.
The cause of aortic stenosis is complex, but it is associated with:
- Chronic inflammation.
- High cholesterol levels.
- Tobacco use.
- Dysregulation of calcium metabolism caused by things like elevated parathyroid levels and end-stage kidney disease.
- Elevated blood levels of calcium and/or vitamin D.
Because of the role of calcium and vitamin D in aortic stenosis, the current study (N Kassis et al, Heart, Epub ahead of print, 1-9, 2022) was designed to ask whether calcium and vitamin D supplementation influenced the risk of dying from aortic stenosis.
How Was This Study Done?
 The Cleveland Clinic scanned their Echocardiography Database for patients aged 60 years or more who had been diagnosed with mild to moderate aortic stenosis. 2,657 patients met these criteria (average age = 74, 58% men) and were followed for an average of 59 months in their database.
The Cleveland Clinic scanned their Echocardiography Database for patients aged 60 years or more who had been diagnosed with mild to moderate aortic stenosis. 2,657 patients met these criteria (average age = 74, 58% men) and were followed for an average of 59 months in their database.
In terms of calcium and vitamin D supplementation:
- 49% did not supplement.
- 12.5% supplemented with vitamin D (dose not defined).
- 38.5% supplemented with calcium (500 – 2,000 mg/day) ± vitamin D.
The study looked at the correlation between vitamin D supplementation and calcium supplementation with:
- Aortic valve replacement surgery.
- All-cause mortality* with and without aortic valve replacement surgery.
- Cardiovascular mortality* with and without aortic valve replacement surgery.
*Note: Since all the patients had aortic stenosis at the beginning of the study, both all-cause and cardiovascular mortality were primarily due to aortic stenosis.
Do Calcium Supplements Increase Deaths From Heart Valve Disease?
 Before I describe the results of the study, there are two things you need to know:
Before I describe the results of the study, there are two things you need to know:
- Vitamin D supplementation did not have a significant effect on any outcome studied, so I will not mention vitamin D in the rest of this article.
- In the calcium supplementing group, there were only a few people taking calcium supplements without vitamin D. However, their outcomes were the same as for people taking calcium + vitamin D supplements. Therefore, the authors discussed their results in terms of calcium supplementation, not calcium + vitamin D supplementation. I will do the same.
With those two things in mind, here is what the study found.
With respect to the need for aortic valve replacement surgery:
- Calcium supplementation increased the need for surgery by 50%.
With respect to all-cause mortality:
- Calcium supplementation increased the risk of death by 31%. When you divided the results into patients who did and did not have aortic valve replacement surgery within the 59-month follow-up of this study:
-
- Those who received aortic valve replacement surgery did not have a statistically significant increase in risk of death.
-
- Those who did not receive aortic valve replacement surgery had a 38% increased risk of death.
With respect to cardiovascular mortality:
- Calcium supplementation doubled the risk of death. When you divided the results into patients who did and did not have aortic valve replacement surgery within the 59-month follow-up of this study:
-
- Those who received aortic valve replacement surgery did not have a statistically significant increase in risk of death.
-
- Those who did not receive aortic valve replacement surgery had a 205% increased risk of death.
The authors concluded, “Supplemental calcium … is associated with lower survival and greater AVR [aortic valve replacement surgery] in elderly patients with mild to moderate AV [aortic stenosis].”
What Did This Study Get Wrong?
 Let me start by looking at the limitations of this study.
Let me start by looking at the limitations of this study.
#1: This is a single study. It is a well-designed study, but it is only one study. And, as the authors acknowledge, previous studies have come down on both sides of this issue. Until we have more well-designed studies that come to the same conclusion, we cannot be confident this study is correct.
#2: The results of this study could have been significantly influenced by confounding variables.
For example:
- End-stage kidney disease is associated with a dysregulation of calcium metabolism that can lead to aortic valve calcification. Patients in the calcium supplementation group had a 2-fold higher incidence of chronic kidney disease and a 10-fold higher incidence of kidney dialysis.
- There were also significant differences in several diseases and drugs that influence the risk of developing aortic stenosis between the groups.
In the words of the authors, “Given the degree of clinical differences between the groups, there was a risk of residual confounding that may have impacted our findings; we attempted to mitigate this with our statistical model.”
However, as Mark Twain is quoted as saying, “There are lies. There are damn lies. And then there are statistics.”
That is a humorous way of saying we should not put too much faith in statistical manipulations of the data.
#3: They did not measure parathyroid levels. That is a serious omission because elevated parathyroid levels are a major driver of the type of dysfunctional calcium metabolism that could lead to calcification of the aortic valve.
#4: Serum calcium and vitamin D levels were slightly lower in the calcium supplementation group. This is unexpected because aortic stenosis is usually associated with higher serum calcium and vitamin D levels.
The authors speculated this might be due to transient increases in serum calcium levels following supplementation. This is possible for some calcium supplements, but not others.
Specifically, some calcium supplements are marketed on how quickly they get into the bloodstream. But those same supplements often do not provide all the nutrients needed for bone formation. There is always the possibility that excess calcium not used for bone formation might be deposited where we do not want it (such as in the aortic valve).
What Did This Study Get Right?
 #1: It was a larger, longer lasting study than previous studies on the effect of calcium supplementation on aortic stenosis. Even though it has limitations, we shouldn’t discount it. It might just be correct.
#1: It was a larger, longer lasting study than previous studies on the effect of calcium supplementation on aortic stenosis. Even though it has limitations, we shouldn’t discount it. It might just be correct.
#2: It doesn’t necessarily conflict with the earlier studies showing that calcium supplementation doesn’t increase cardiovascular disease risk. That’s because the design of these studies is very different.
- The health of the people studied was very different.
-
- The earlier studies started with healthy adults and asked whether calcium supplementation increased their risk of developing cardiovascular disease.
-
- This study started with people who already had a form of cardiovascular disease associated with abnormal calcium metabolism and asked whether calcium supplementation increased their risk of dying from the disease.
- The age of the people studied was very different.
-
- The earlier studies started with middle-aged adults and followed them for 10-20 years
-
- This study started with people in their mid-70’s and followed them for almost 6 years.
- The type of cardiovascular disease studied was different.
-
- The earlier studies included all types of cardiovascular disease.
-
- This study focused on a very minor type of cardiovascular disease, aortic stenosis. Aortic stenosis accounts for about 10% of all cardiovascular disease 17% of cardiovascular deaths. There may not have been enough deaths from aortic stenosis in the previous studies to have had a statistically significant effect on the results.
Given all these differences, the results of this study may not be incompatible with the results of previous studies
What Does This Study Mean For You?
 There are three important takeaways from this and previous studies:
There are three important takeaways from this and previous studies:
1) For most Americans calcium supplementation does not increase the risk of cardiovascular disease. That has been shown in three major clinical studies.
2) However, if you have been diagnosed with aortic stenosis, calcium supplementation may increase your risk of needing heart valve replacement or of dying from the disease. This study is not definitive, but I would advise caution.
You may wish to discuss with your doctor how to best balance:
-
- The need for calcium supplementation to prevent osteoporosis…
-
- With the need to limit calcium supplementation to prevent adverse outcomes from your aortic stenosis.
3) Finally, the authors did not discuss a very significant observation from this study, namely that heart valve replacement reduced the risk of dying from aortic stenosis in people taking calcium supplements.
Aortic valve replacement is the only proven treatment for aortic stenosis. If your doctor recommends aortic valve replacement, you should consider it.
The Bottom Line
A recent study looked at the effect of calcium supplementation for people with aortic stenosis, a rare form of heart disease.
The study found:
- Calcium supplementation increased the need for aortic valve replacement surgery by 50%.
- Calcium supplementation increased the risk of all-cause mortality* by 31%. When you divided the results into patients who did and did not have aortic valve replacement surgery during the study:
-
- Those who received aortic valve replacement surgery did not have a statistically significant increase in risk of death.
- Calcium supplementation doubled the risk of cardiovascular mortality*. When you divided the results into patients who did and did not have aortic valve replacement surgery within the 59-month follow-up of this study:
-
- Those who received aortic valve replacement surgery did not have a statistically significant increase in risk of death.
*Note: Since all the patients enrolled in this study had aortic stenosis at the beginning of the study, these deaths were primarily due to aortic stenosis.
The authors concluded, “Supplemental calcium … is associated with lower survival and greater AVR [aortic valve replacement surgery] in elderly patients with mild to moderate AV [aortic stenosis].”
There are three important takeaways from this and previous studies:
1) For most Americans calcium supplementation does not increase the risk of cardiovascular disease. That has been shown in three major clinical studies.
2) However, if you have been diagnosed with aortic stenosis, calcium supplementation may increase your risk of needing heart valve replacement or of dying from the disease. This study is not definitive, but I would advise caution.
- You may wish to discuss with your doctor how to best balance:
-
- The need for calcium supplementation to prevent osteoporosis…
-
- With the need to limit calcium supplementation to prevent adverse outcomes from your aortic stenosis.
3) Finally, the authors did not discuss a very significant observation from this study, namely that heart valve replacement reduced the risk of dying from aortic stenosis in people taking calcium supplements.
Aortic valve replacement is the only proven treatment for aortic stenosis. If your doctor recommends aortic valve replacement, you should consider it.
For more details, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
