Leading Causes Of Maternal Deaths
Author: Carolyn Curtis, MSN, CNM, RN, FACNM, FAAN
Editor: Dr. Steve Chaney
Maternal Mortality In The United States
Between 2018 and 2021, the maternal mortality (death) rate in the United States nearly doubled, placing the country last among developed nations in maternal health outcomes. The maternal mortality ratio (MMR) is a key indicator of a nation’s overall health, making this rapid increase a cause for serious concern.
Understanding Maternal Mortality
Maternal mortality refers to the number of women who die during pregnancy or within 42 days (six weeks) after childbirth for every 100,000 live births. As per the Government Accounting Office, 25% of the increase in maternal mortality from 2020 to 2021 was due to Covid-19, which contributed to the doubling of the maternal mortality ratioi.
The maternal mortality ratio is used globally to assess the state of a country’s health. A rising MMR signals the need for urgent action.
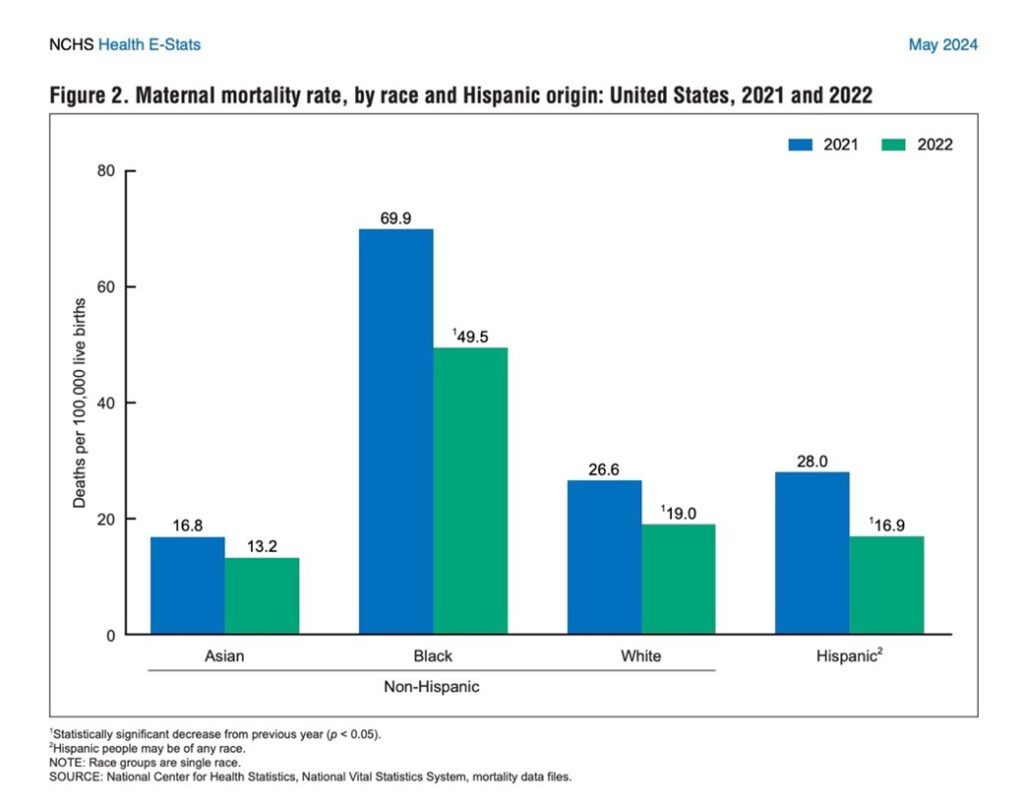
In 2022, the U.S. recorded an overall maternal mortality ratio 22.3 deaths per 100,000 live birthsii. This decreased by about 10 deaths per 100,000 from 2021 (32 deaths per 100,000 live births in 2021). However, stark racial disparities continued to exist as demonstrated through 2018 to 2021.
- Black women: 49.5 deaths per 100,000 live births (more than 2.5 times the rate for white women)
- White women: 19.0 deaths per 100,000 live births
- Hispanic women: 16.9 deaths per 100,000 live births
- Asian women: 13.2 deaths per 100,000 live births
 Maternal Mortality versus Pregnancy Related Deaths
Maternal Mortality versus Pregnancy Related Deaths
What Is The Difference?
While maternal mortality measures deaths that occur from the onset of pregnancy to six weeks post-delivery, pregnancy-related deaths extend further. Pregnancy-related deaths are the number of deaths per 100,000 live births up to 12 months (one year) after birth or the first birthday.
Does The Age Of The Mother Make A Difference?
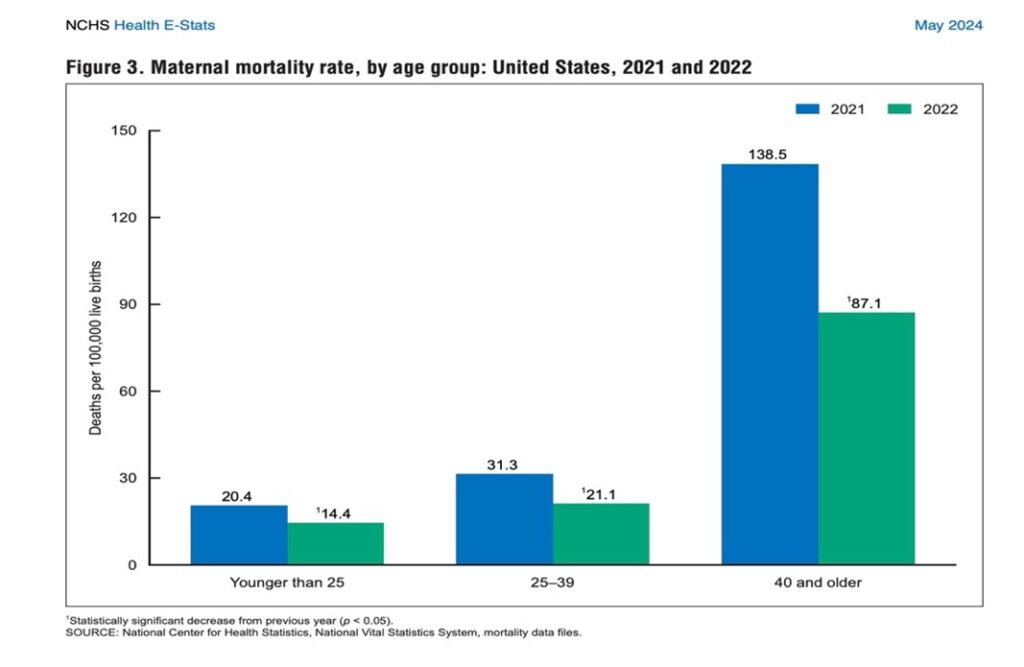
The age of the mother significantly affects the risk of dying during pregnancy. The ratio of deaths among women younger than 25 years of age is 14.4 deaths per 100,000 live births. Women aged 25 to 39 have a rate of 21.1/100,000 live births, while those aged 40 and older face a staggering 87.1 deaths per 100,000 live birthsiii. This means that women over 40 are dying at six times the rate of those under 25 and four times the rate of women aged 25 to 29iv.
 When Are The Deaths Occurring?
When Are The Deaths Occurring?
Surprisingly, a little under half (47%) of maternal deaths occur during pregnancy or within the first week postpartum (Maternal Mortality). And a little over half (53%) happen between one week and one year after childbirth or the baby’s first birthday (Pregnancy-Related Deaths).
Leading Causes Of Maternal Deaths
The primary causes of maternal mortality in the U.S. are largely preventablev. The six main causes of maternal death include:
- Mental Health Conditions (23%) – Suicide, overdose, and substance-related poisoning are the leading causes, this affects White and Hispanic women more than Black or Asian women.
- Hemorrhage (14%) – Severe postpartum bleeding remains one of the top causes of maternal deaths not only in the Unites States but throughout the world with Asian women being more susceptible. Hemorrhage is defined as bleeding about one half quart of blood.
- Cardiac Conditions (13%) – Heart disease disproportionately affects Black women.
- Blood Clots (9%) – A major contributor to maternal deaths.
- Cardiomyopathy (9%) – A condition affecting the heart muscle, making it harder to pump blood efficiently.
- Hypertensive Disorders of Pregnancy (7%) – relating to high blood pressure
Contributors to maternal death include familial, societal, health care system issues and one’s personal health. it is possible to reduce the risks of maternal death by understanding one’s personal health history and your family’s health history.
This information informs nutritional, behavioral and lifestyle changes that can be made prior to and during pregnancy to reduce health risks, enabling a healthier pregnancy outcome.
The Bottom Line
- The United States has the highest maternal mortality rate amongst all developed countries in the world.
- The maternal mortality rate in the U.S. has nearly doubled between 2018 and 2021; Covid-19 caused a 25% increase of maternal deaths from 2020 to 2021 which contributed to the doubling of maternal deaths. Black women have been disproportionately affected, with mortality rates 2.5x that of White women.
- Women aged 40 and over die at four times the rate of women ages 25 to 39 and six times more than women under 25 years of age.
- The leading causes of maternal deaths include mental health conditions, hemorrhage, cardiac conditions, blood clots, and cardiomyopathy— most of which are preventable.
- Almost half of maternal deaths occur throughout pregnancy and the first week after childbirth. A little more than half of maternal deaths occur from the first week following birth up to the first year after birth. It’s important to continue monitoring mothers with home visits once they return home from the hospital and up until one year after birth.
References
i General Accounting Office, Maternal Health: Outcomes Worsened and Disparities Persisted During the Pandemic. Oct, 2022.
ii Hoyert DL. Maternal mortality rates in the United States, 2022. NCHS Health E-Stats. 2024. DOI:https://dx.doi.org/10.15620/cdc/152992.
iii Ibid
iv Ibid.
vFour in five pregnancy related deaths in the US are preventable – https://www.cdc.gov/media/releases/2022/p0919-pregnancy-related-deaths.html.
For More Information
Feel free to visit my website, subscribe to my YouTube channel and learn more about my online coaching program, “Mastering Pregnancy and Birth”.
You-Tube Channel – Over 80 videos exploring pregnancy, labor, birth, postpartum and contraception
www.thecarabcompany.com – Website with free downloadable pregnancy and birth information
Mastering Pregnancy and Birth Coaching Program – A program that prepares Dads and Mom’s-to-be for a healthier pregnancy and safer birth. This course also provides information for Doulas to provide enhanced support to families.
Carolyn Curtis
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
About The Author
 Carolyn Curtis, MSN, CNM, RN, FACNM, FAAN, has:
Carolyn Curtis, MSN, CNM, RN, FACNM, FAAN, has:
- More than 40 years’ experience in the oversight of domestic and international programs and the provision of nursing and midwifery integrated service delivery in maternal child health, family planning, reproductive and women’s health care.
- Twenty years’ experience in teaching, mentoring, and providing clinical oversight to undergraduate and graduate public health, medical, nursing and midwifery students.
About The Editor
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.
