What Does This Study Mean For You?
Author: Dr. Stephen Chaney
 Yes, you read the headline correctly. Everyone talks about postnatal depression. But prenatal depression is also a “thing”, especially during the third trimester.
Yes, you read the headline correctly. Everyone talks about postnatal depression. But prenatal depression is also a “thing”, especially during the third trimester.
- Worldwide, 4-20% of women experience some degree of depression during the third trimester – with pregnant women in high-income countries at the lower end (4-10%) of depression risk.
- In contrast, the incidence of postnatal depression is 10-15%.
It is probably no coincidence that the incidence of depression is greatest during the third trimester and during the postnatal period.
- The third trimester is the most difficult part of pregnancy for many women.
- When a woman brings her baby home from the hospital her orderly life becomes chaotic.
But what role does nutrition play?
- While not definitive, many studies suggest that supplementation with B vitamins, especially folic acid, B6, and B12; omega-3 fatty acids; vitamin D; and iron reduce the risk of postnatal depression.
- However, there is much less information on which nutrients reduce the risk of prenatal depression.
Based on studies suggesting both iron and vitamin D deficiencies may negatively impact mental health, the authors of this study (JL Evanchuk et al, The Journal Of Nutrition. 154, 174-184, 2024) set out to determine whether iron and/or vitamin D deficiencies increase the risk of prenatal depression during the first trimester.
How Was This Study Done?
 The authors recruited 2189 newly pregnant mothers from Calgary and Edmonton in Ontario Canada between 2009 and 2012. Participants in the study visited clinics in the area upon entry into the study; midway through the first, second, and third trimesters; and at multiple timepoints up to 3 months during the postpartum period.
The authors recruited 2189 newly pregnant mothers from Calgary and Edmonton in Ontario Canada between 2009 and 2012. Participants in the study visited clinics in the area upon entry into the study; midway through the first, second, and third trimesters; and at multiple timepoints up to 3 months during the postpartum period.
In addition to the usual pregnancy wellness tests, participants filled out a 24-hour dietary recall and a Supplemental Intake Questionnaire to determine intakes of iron and vitamin D.
Note: The participants were all advised to take some form of prenatal supplement during the study. That’s because prenatal supplements are considered “the standard of care” for pregnant woman, so it would be considered unethical not to include a prenatal supplement in this study.
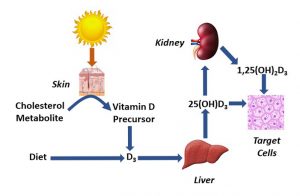
At the mid-point of the second trimester blood samples were drawn and analyzed for biomarkers of iron and vitamin D insufficiency. For iron the biomarkers were serum ferritin, soluble transferrin receptor, and hepcidin. For vitamin D, the biomarkers were 25-hydroxyvitamin D, 1,25-dihydroxyvitamin D, and 3-epi-25-hydroxyvitamin D.
Iron deficiency was defined as serum ferritin levels <15 µg/L. Vitamin D insufficiency was defined as 25-hydroxyvitamin D levels < 75nmol/L. The other biomarkers were used to confirm these diagnoses.
Maternal depression was measured midway through the third trimester and ~3 months postpartum using 10-item questionnaire called the Edinburg Postnatal Depression Scale (EPDS). The EPDS ranks depression on a scale of 0 to 30, with a score of ≥13 considered an indication of likely depression.
The characteristics of the women enrolled in this study were:
- Average age = 31.5
- Average prepregnancy BMI = 23 (healthy weight).
- Married or cohabitating with a partner = 97%.
- Highly educated (college or postgraduate degree) = 68%.
- Income above $70,000/year = 78%.
- First child = 54%.
- White = 80%.
Based on the Edinburg Depression Scale, probably depression for the 1822 women who completed the study was 5.6% during the third trimester and 4.4% 3 months postpartum.
Note: The low incidence of depression seen in this study was probably due to:
- The women in this study were of high socioeconomic status and were receiving excellent healthcare.
- The women in this study were taking prenatal supplements that provided both iron and vitamin D.
Which Nutrients Prevent Prenatal Depression?
 As I mentioned when describing how the study was designed, all participants in this study were advised to take a prenatal supplement. Consequently:
As I mentioned when describing how the study was designed, all participants in this study were advised to take a prenatal supplement. Consequently:
- 94% of the women in this study were taking a supplement containing iron with an average supplemental iron intake of 26 mg/day.
-
- Note: The RDA for iron during pregnancy is 30 mg/day and most prenatal supplements provide 27 mg/day.
- 68% of the women in this study were taking a supplement containing vitamin D, with an average supplemental vitamin D intake of 330 IU/day.
-
- Note: The RDA for vitamin D during pregnancy is 600 IU/day, but most prenatal supplements provide far less than that.
When the investigators looked at iron and vitamin D status during the second trimester:
- 63.3% of the women had adequate levels of both iron and vitamin D.
- 14.8% of the women were low in vitamin D but had adequate iron levels.
- 18.4% of the women were low in iron but had adequate levels of vitamin D.
- 3.5% of the women were low in both iron and vitamin D.
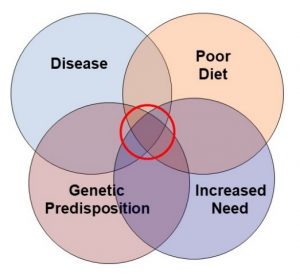
RDAs are supposed to be enough to meet the nutrient requirements of 97-98% of healthy individuals, so it is perhaps surprising to see so many women with insufficient levels of iron (21.9%) and/or vitamin D (18.3%) in this study. This could be due to:
- Insufficient intake.
-
- This is a likely explanation for vitamin D because the supplements women were using in this study provided around half the recommended RDA for vitamin D and the women lived at a northern latitude where sun exposure makes a small contribution to vitamin D levels.
-
- However, this is a less likely explanation for insufficient iron levels because the supplements provided 87% of the RDA for iron.
- Inadequate RDAs. Studies like this one provide a rigorous test for the adequacy of existing RDAs. This study suggests the existing RDA for iron is adequate to meet the needs of ~80% of pregnant women, which is reassuring. However, it may need to be increased to reach the goal of meeting the iron requirements for 97-98% of pregnant women.
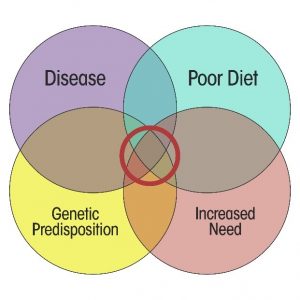
But the important question is whether the iron and vitamin D insufficiencies seen in this study mattered. The data suggested that they did.
- For pregnant women with low iron, but adequate vitamin D levels in the second trimester, there was a small, but significant, increased risk of experiencing depression symptoms in the third trimester.
- For pregnant women with low iron and vitamin D levels in the second trimester, the risk of experiencing depression symptoms in the third trimester increased by 2.2 points in the 30-point Edinburg Depression Scale.
-
- This is equivalent to a 7.4% increased risk of depression from deficiencies of iron and vitamin D alone – and these are only 2 of at least 8 nutrients thought to be associated with maternal depression.
The authors concluded, “Maternal iron and vitamin D biomarkers, measured during midpregnancy, were independently associated with third trimester maternal depression symptoms…This investigation is one of the first to report on the combined adequacy of maternal iron and vitamin D status during pregnancy and its impact on maternal depression.
The novelty of this work reinforces the need to ask similar questions [with other nutrients and] in other pregnant populations. Future investigations should report on the status of multiple nutrients and explore their independent and combined impact on health outcomes of pregnant individuals and their children.”
What Does This Study Mean For You?
 Depression during pregnancy is bad for you. And because your fetus can sense your mood, it is bad for your baby. So, what should you do?
Depression during pregnancy is bad for you. And because your fetus can sense your mood, it is bad for your baby. So, what should you do?
You can consult with your doctor about which antidepressants are safe to take during pregnancy. But the truth is there are no good choices. There are some antidepressants that are off limits. There are other antidepressants that appear to have little short-term risks, but we have no idea if there are long-term risks for your child.
So, what about natural approaches? Let’s start with nutrition.
The biggest takeaway from this study is that prenatal supplements may not be sufficient to prevent nutritional deficiencies that may cause prenatal depression for pregnant women.
- This does not mean that every pregnant woman suffering prenatal depression should increase their iron and vitamin D levels.
- However, if you are experiencing prenatal depression, you might want to ask your doctor about checking your iron and vitamin D status to determine if extra iron and/or vitamin D would be beneficial.
And to put this study into its proper perspective we need to remember that iron and vitamin D deficiencies are only two of many nutrients that may increase the risk of prenatal depression.
For example, in addition to iron and vitamin D, prenatal depression is associated with deficiencies of:
- B vitamins, especially folate, B6 and B12. Most prenatal supplements provide the recommended RDA of folate for pregnant women, but not all contain RDA amounts of B6 and B12.
- Calcium and magnesium. Very few prenatal supplements provide the recommended RDA for calcium and magnesium.
- Omega-3s, especially DHA. Very few prenatal supplements provide DHA, and the few that do usually provide inadequate amounts of DHA.
So, when you are having your nutrition conversation with your doctor, you might not want to limit your conversation to iron and vitamin D.
Alternately, as I suggested last week’s issue of “Health Tips From the Professor”, you might wish to add a multivitamin supplement and an omega-3 supplement providing at least 300 mg of DHA plus EPA. This simple step would be sufficient to assure you have adequate levels of nutrients thought to be important for reducing the risk of prenatal depression.
And, of course, there are other lifestyle factors, as well. For example:
- Diets high in highly processed foods are known to increase the risk of depression. And whole food, primarily plant-based diets decrease the risk of depression.
- Overweight and obesity increase the risk of depression.
- Regular exercise decreases the risk of depression.
The Bottom Line
A recent study looked at whether taking a prenatal supplement was sufficient to eliminate deficiencies of iron and vitamin D during pregnancy and whether deficiencies of these two nutrients during the second trimester of pregnancy increased the risk of depression during the third trimester.
When the investigators looked at iron and vitamin D status during the second trimester:
- 14.8% of the women were low in vitamin D but had adequate iron levels.
- 18.4% of the women were low in iron but had adequate levels of vitamin D.
- 3.5% of the women were low in both iron and vitamin D.
But the important question is whether the iron and vitamin D insufficiencies seen in this study mattered. The data suggested that they did.
- For pregnant women with low iron, but adequate vitamin D levels in the second trimester, there was a small, but significant, increased risk of experiencing depression symptoms in the third trimester.
- For pregnant women with low iron and vitamin D levels in the second trimester, the risk of experiencing depression symptoms in the third trimester increased by 2.2 points in the 30-point Edinburg Depression Scale.
- This is equivalent to a 7.4% increased risk of depression from deficiencies of iron and vitamin D alone.
When you consider that iron and vitamin D are just two of 8 or more nutrients thought to be important for preventing depression during pregnancy, the question becomes what you can do to decrease your risk of developing depression during pregnancy and after the birth of your child.
For more details about the study and what it means for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
___________________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
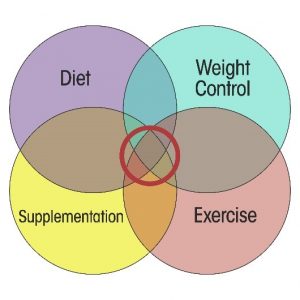
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.