Are Low Carb Enthusiasts Right About The Dangers Of Carbohydrates?
Author: Dr. Stephen Chaney
 Low carb enthusiasts have been on the warpath against carbohydrates for years.
Low carb enthusiasts have been on the warpath against carbohydrates for years.
Almost everyone agrees that sugar-sweetened sodas and highly processed, refined foods with added sugar are bad for us. But low carb enthusiasts claim that we should also avoid fruits, grains, and starchy vegetables. Have they gone too far?
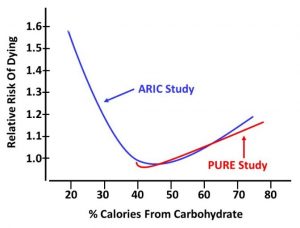
Several recent studies suggest they have. For example, both association studies and randomized controlled studies suggest that total carbohydrate intake is neither harmful nor beneficial for heart health.
In addition, recent studies suggest that free sugar intake is associated with both elevated triglyceride levels and an increase in heart disease risk.
But those studies have mostly looked at free sugar intake from sugar-sweetened sodas. The authors of this study (RK Kelley et al, BMC Medicine, 21:34, 2023) decided to look more carefully at the effect of all free sugars and other types of carbohydrates on triglyceride levels and heart disease risk.
How Was This Study Done?
 The 110,497 people chosen for this study were a subgroup of participants in the UK Biobank Study, a large, long-term study looking at the contributions of genetic predisposition and environmental exposure (including diet) to the development of disease in England, Scotland, and Wales.
The 110,497 people chosen for this study were a subgroup of participants in the UK Biobank Study, a large, long-term study looking at the contributions of genetic predisposition and environmental exposure (including diet) to the development of disease in England, Scotland, and Wales.
The participants in this study were aged between 37 and 73 (average age = 56) on enrollment and were followed for an average of 9.4 years. None of them had a history of heart disease or diabetes or were taking diabetic medications at the time of enrollment.
During the 9.4-year follow-up, five 24-hour dietary recalls were performed, so that usual dietary intake could be measured rather than dietary intake at a single time point. The people in this study participated in an average of 2.9 diet surveys, and none of them had less than two diet surveys.
The averaged data from the dietary recalls were analyzed for the amount and kinds of carbohydrate in the diet. With respect to the types of carbohydrate, the following definitions would be useful.
- The term free sugars includes all monosaccharides and disaccharides added to foods by the manufacturer, cook, or consumer, plus sugars naturally present in honey, syrups, and unsweetened fruit juices.
- The term non-free sugars includes all sugars not in the free sugar category, mostly sugars naturally occurring in fruits, vegetables, and dairy products.
- The term refined grains includes white bread, white pasta, white rice, most crackers and cereals, pizza, and grain dishes with added fat.
- The term whole grains includes wholegrain bread, wholegrain pasta, brown rice, bran cereal, wholegrain cereals, oat cereal, and muesli.
Finally, the study looked at the association of total carbohydrate and each class of carbohydrate defined above with all heart disease, heart attacks, stroke, and triglyceride levels.
Are All Carbs Bad?
 The study looked at total carbohydrate intake, free sugar intake, and fiber intake. In each case, the study divided the participants into quartiles and compared those in the highest quartile with those in the lowest quartile.
The study looked at total carbohydrate intake, free sugar intake, and fiber intake. In each case, the study divided the participants into quartiles and compared those in the highest quartile with those in the lowest quartile.
Using this criterion:
- Total carbohydrate intake was not associated with any cardiovascular outcome measured (total heart disease risk, heart attack risk, and stroke risk).
- Free sugar intake was positively associated with all cardiovascular outcomes measured. Each 5% increase in caloric intake from free sugars was associated with a:
-
- 7% increase in total heart disease risk.
-
- 6% increase in heart attack risk.
-
- 10% increase in stroke risk.
-
- 3% increase in triglyceride levels.
- Fiber intake was inversely associated with total heart disease risk. Specifically, each 5 gram/day increase in fiber was associated with a:
-
- 4% decrease in total heart disease risk.
The investigators also looked at the effect of replacing less healthy carbohydrates with healthier carbohydrates. They found that:
- Replacing 5% of caloric intake from refined grains with whole grains reduced both total heart disease risk and stroke risk by 6%.
- Replacing 5% of caloric intake from free sugars (mostly sugar-sweetened beverages, fruit juices, and processed foods with added sugar) with non-free sugars (mostly fruits, vegetables, and dairy products) reduced total heart disease risk by 5% and stroke risk by 9%.
Are Low Carb Enthusiasts Right About The Dangers Of Carbohydrates?
 With these data in mind let’s look at the claims of the low-carb enthusiasts.
With these data in mind let’s look at the claims of the low-carb enthusiasts.
Claim #1: Carbohydrates raise triglyceride levels. This study shows:
- This claim is false with respect to total carbohydrate intake and high fiber carbohydrate intake (fruits, vegetables, and whole grains. This study did not measure intake of beans, nuts, and seeds, but they would likely be in the same category).
- However, this claim is true with respect to foods high in free sugars (sugar-sweetened beverages, fruit juices, and processed foods with added sugar).
Claim #2: Carbohydrates increase heart disease risk. This study shows:
- That claim is false with respect to total carbohydrate intake and high fiber carbohydrate intake.
- However, this claim is true with respect to foods high in free sugars.
Claim #3: Carbohydrates cause weight gain [Note: Low carb enthusiasts usually word it differently. Their claim is that eliminating carbohydrates will help you lose weight. But that claim doesn’t make sense unless you believed eating carbohydrates caused you to gain weight.] This study shows:
- This claim is false with respect to total carbohydrate intake and high fiber carbohydrate intake.
- Once again, this claim is true with respect to foods high in free sugars.
The data with high fiber carbohydrates was particularly interesting. When the authors compared the group with the highest fiber intake to the group with the lowest fiber intake, the high-fiber group:
- Consumed 33% more calories per day.
- But had lower BMI and waste circumference (measures of obesity) than the low-carbohydrate group.
This suggests that you don’t need to starve yourself to lose weight. You just need to eat healthier foods.
And, in case you were wondering, the high fiber group ate:
- 5 more servings of fruits and vegetables and…
- 2 more servings of whole grain foods than the low fiber group.
This is consistent with several previous studies showing that diets containing a lot of fruits, vegetables, and whole grains are associated with a healthier weight.
The authors concluded, “Higher free sugar intake was associated with higher cardiovascular disease incidence and higher triglyceride concentrations…Higher fiber intake and replacement of refined grain starch and free sugars with wholegrain starch and non-free sugars, respectively, may be protective for incident heart disease.”
In short, with respect to heart disease, the type, not the amount of dietary carbohydrate is the important risk factor.
What Does This Mean For You?
 Forget the low carb “mumbo jumbo”.
Forget the low carb “mumbo jumbo”.
- Carbohydrates aren’t the problem. The wrong kind of carbohydrates are the problem. Fruit juice, sugar-sweetened sodas, and processed foods with added sugar:
-
- Increase triglyceride levels.
-
- Are associated with weight gain.
-
- Increase the risk for heart disease.
- In other words, they are the villains. They are responsible for the bad effects that low carb enthusiasts ascribe to all carbohydrates.
- Don’t fear whole fruits, vegetables, dairy, and whole grain foods. They are the good guys.
-
- They have minimal effect on triglyceride levels.
-
- They are associated with healthier weight.
-
- They are associated with a lower risk of heart disease and diabetes.
So, the bottom line for you is simple. Not all carbs are created equal.
- Your mother was right. Eat your fruits, vegetables, and whole grains.
- Avoid fruit juice, sodas and other sugar-sweetened beverages, and processed foods with added sugar. [Note: Artificially sweetened beverages are no better than sugar-sweetened beverages, but that’s another story for another day.]
And, if you were wondering why low carb diets appear to work for weight loss, it’s because any restrictive diet works short term. As I have noted previously, keto and vegan diets work equally well for short-term weight loss.
The Bottom Line
Low carb enthusiasts have been telling us for years to avoid all carbohydrates (including fruits, starchy vegetables, and whole grains) because carbohydrates:
- Increase triglyceride levels.
- Cause weight gain.
- Increase our risk for heart disease.
A recent study has shown that these claims are only true for some carbohydrates, namely fruit juices, sodas and other sugar-sweetened beverages, and processed foods with added sugar.
Whole fruits, vegetables, and whole grain foods have the opposite effect. They:
- Have a minimal effect on triglyceride levels.
- Are associated with a healthier weight.
- Are associated with a lower risk of heart disease and diabetes.
So, forget the low carb “mumbo jumbo” and be sure to eat your fruits, vegetables, and whole grains.
For more information on this study and what it means for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
___________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance