Nutritional Inadequacies Of The American Diet
Author: Dr. Stephen Chaney
 If you are like most Americans, you are probably confused by the conflicting information about the nutritional adequacy of the American diet.
If you are like most Americans, you are probably confused by the conflicting information about the nutritional adequacy of the American diet.
- On the on hand, many bloggers, websites, and the Dr. Strangeloves of the world are telling you the American diet is woefully inadequate, and you need supplements.
- On the other hand, the pharmaceutical and medical industry are telling you that you get all the nutrients you need from your diet. They tell you supplements are a waste of money.
As usual, the truth lies somewhere in between.
- There are certain nutrients that are often present in inadequate amounts in our diets, and these should be targeted for correction.
The nutritional inadequacies of the American diet have been well documented, and I will discuss those below.
But nutritional inadequacies on a global perspective are less well documented. That was the purpose of the study (S Passarelli et al, Lancet Global Health, 12: e1590-e1599, 2024) that I will review today.
But first, I should discuss how nutritional inadequacies are defined and their implications for our health.
What Are Nutrient Inadequacies And How Are They Defined?
 Nutrient Deficiencies are defined as nutrient intakes that are below the level needed to maintain normal metabolic and physiological functions. Nutrient deficiencies can lead to health consequences such as anemia (iron or B12 deficiency), scurvy (vitamin C deficiency), or pellagra (B6 deficiency).
Nutrient Deficiencies are defined as nutrient intakes that are below the level needed to maintain normal metabolic and physiological functions. Nutrient deficiencies can lead to health consequences such as anemia (iron or B12 deficiency), scurvy (vitamin C deficiency), or pellagra (B6 deficiency).
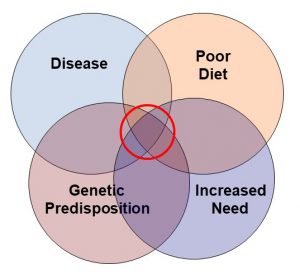
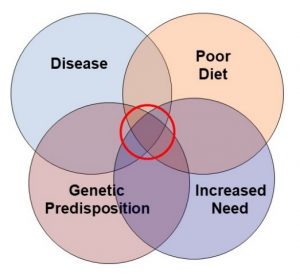
Nutrient Inadequacies are defined as nutrient intakes that are below dietary intake recommendations but above the levels associated with nutrient deficiency.
While nutrient inadequacies do not lead to clearly defined deficiency symptoms such as scurvy, they are not benign.
- They lead to symptoms that are difficult to diagnose because they could have many causes such as:
-
- Fatigue
-
- Increased susceptibility to viral and bacterial diseases like flu and COVID.
-
- Impaired cognitive functions like attention, focus, and memory.
-
- Mood disorders like anxiety and depression.
- And if they persist long enough, they can increase the risk of chronic diseases.
When estimating nutrient inadequacies, it is also important to consider the standard for dietary intake recommendations they are being compared to.
The Recommended Daily Intake (DRI) is defined as the level of a nutrient that is likely to meet the needs of 97-98% of individuals based on age, gender, and other factors such as pregnancy and lactation.
The Estimated Average Requirement (EAR) is defined as the level of a nutrient that is likely to meet the needs of 50% of individuals based on age, gender, and other factors such as pregnancy and lactation.
This distinction is important because the standard chosen has a large impact on the percentage of people within a population group who are deemed to have an inadequate diet.
- The data I will discuss in this article refer to the percentage of individuals in a particular group who do meet the EAR standard.
- Obviously, the percentage of people with nutrient inadequacies would have been much higher if the DRI standard had been used.
How Was This Study Done?
The authors obtained their data from the WHO Global Dietary Database (GDD). They compared nutrient intake for 15 micronutrients with a standard that was based on the needs of 50% of healthy people. Each country sets their own standards for nutrient intakes, so they used “harmonized average requirements” from all the countries in the GDD database as the standard for comparisons.
They then segmented the data into estimates for 34 age-sex groups from 185 countries in the database.
A Global Perspective Of Dietary Inadequacies
![]() The data are alarming. Let’s start with nutrient intakes that were inadequate for more than 50% of the world’s population:
The data are alarming. Let’s start with nutrient intakes that were inadequate for more than 50% of the world’s population:
- Iodine, 68%.
- Vitamin E, 67%.
- Calcium, 66%.
- Iron, 65%.
- Riboflavin, 55%.
- Folate, 54%.
- Vitamin C, 53%.
- Vitamin B6, 51%.
Nutrient intakes that were inadequate for between 20% and 50% of the world’s population were:
- Vitamin A, 48%.
- Zinc, 46%
- Vitamin B12, 39%.
- Selenium, 38%.
- Magnesium, 31%.
- Thiamin, 30%.
- Niacin, 22%.
[Note: some micronutrients like vitamin D were not included in this study.]
Within the same country and age group, nutrient inadequacies were:
- Higher for women than men for iodine, vitamin B12, iron, and selenium.
- Higher for men than women for magnesium, vitamin B6, zinc, vitamin C, vitamin A, thiamin, and niacin.
Other important observations were:
- Two thirds of women aged 15-49 had inadequate intakes of iron, zinc, and/or folate. These are the childbearing years, and adequate intake of iron and folate are important for a healthy pregnancy.
- Over half of children under age 5 had inadequate intakes of iron, zinc, and vitamin A. Deficiencies of iron and vitamin A can have devastating health consequences during this important developmental period.
The authors concluded, “These findings show empirically that most of the global population has inadequate intake of at least one nutrient…Estimates of inadequate global micronutrient intakes [like this one] can help public health researchers and practitioners to identify which age and sex groups in which countries might be in greatest need of intervention for [which] micronutrients.”
Nutrient Inadequacies Of The American Diet
 The global distribution of nutritional inadequacies was presented as a color-coded map of the world, so I can’t give you exact percentages of nutrient inadequacies in the United States from this study. However, based on the color coding, nutrient inadequacies in the United States are:
The global distribution of nutritional inadequacies was presented as a color-coded map of the world, so I can’t give you exact percentages of nutrient inadequacies in the United States from this study. However, based on the color coding, nutrient inadequacies in the United States are:
- ≥75% for iodine and vitamin E.
- ≥50% for vitamin C.
- ≥30% for iron and magnesium.
- ≥25% for calcium and vitamin A.
These percentages of nutrient inadequacies may seem a little lower than estimates you have seen elsewhere. That’s because:
- These numbers represent the percentage of the US population that is getting less than the EAR, the amount that meets the needs of 50% of healthy adults. If the percentages were based on the DRI, the amount that meets the needs of 97-98% of healthy adults, the percentages would be higher.
- These numbers are the average of men and women in all age groups in the United States. When you break the numbers down further:
-
- Women of childbearing age are much more likely to have low intakes of iron, and iodine than other groups. And these are nutrients that are important for a healthy pregnancy.
-
- Teens of both sexes are much more likely to have inadequate intakes of iron and calcium than other age groups.
Do Nutrient Inadequacies Matter?
 Statistics like these are provocative. They are alarming. But there are two important questions we need to ask:
Statistics like these are provocative. They are alarming. But there are two important questions we need to ask:
- Do these nutrient inadequacies matter?
- Who do they matter for?
The answer to these questions depends on two things – the percentage of people with inadequate nutrient intake and the likelihood that it has significant health consequences.
Simply put:
- If 80% of the population has an inadequate intake of a particular nutrient, but inadequate intake of that nutrient has no known health consequences, it is not particularly worrying.
- On the other hand, if 40% of the population has an inadequate intake of a particular nutrient, but inadequate intake of that nutrient has significant health consequences, it is a cause for concern.
The USDA’s 2020-2025 US Dietary Guidelines list nutrients that are of “public health concern” for each age group. Nutrients of public health concern are nutrients that:
- Are consumed in inadequate amounts in the American diet.
- Are associated with health concerns when their intake is low.
Here is their list of nutrients of public health concern for each age group:
- General population.
- Nutrients of public health concern are calcium, dietary fiber, and vitamin D.
2) Breast Fed Infants.
-
- Vitamin D3. And supplementation with 400 IU/day of vitamin D is recommended shortly after birth.
3) Vegetarian Toddlers.
-
- Iron and vitamin B12 are nutrients of concern.
4) Children & Adolescents.
-
- Calcium and vitamin D are nutrients of concern.
-
- Iron, folate, vitamin B6, vitamin B12, and magnesium are also nutrients of concern for adolescent females.
5) Adults (Ages 19-59).
-
- 30% of men and 60% of women do not consume enough calcium and 90% of both men and women do not get enough vitamin D. These are nutrients of concern for this age group.
6) Pregnant & Lactating Women:
-
- Calcium, vitamin D, and fiber are nutrients of concern for all women in this age group.
-
- In addition, women who are pregnant have special needs for folate/folic acid, iron, iodine, and vitamin D.
7) Older Adults (≥ 60).
-
- Nutrients of concern for this age group include calcium, vitamin D, fiber, vitamin B12, and protein.
-
-
- In fact, about 50% of women and 30% of men in this age group do not get enough protein in their diet.
-
What Does This Study Mean For You?
 Nutrient inadequacies are a serious concern, both here in the United States and across the world.
Nutrient inadequacies are a serious concern, both here in the United States and across the world.
There are 3 possible solutions to this problem.
1) Governments can provide dietary guidelines for the general population and food assistance for the needy.
In our country dietary guidelines have been an abysmal failure. Only 3% of the US population paid any attention to the food guide pyramid. It was deemed too complicated and was replaced by MyPlate which engaged a whopping 5% of the US population.
2) The food industry can fortify popular foods with “nutrients of concern”.
The most recent food fortification in the United States occurred in 1998 with the addition of folic acid to refined grains. The only other food fortifications in the United States are iodine in salt, vitamin D in milk, and some B vitamins in refined grains. There are no plans for further food fortification currently.
3) Supplementation.
Supplementation is the best option for most of us. It is an inexpensive way to eliminate nutrient inadequacies and their accompanying health concerns. It is something that each of us can control.
We don’t need to wait for the government or the food industry to get their act together. We can take our nutrition and our health into our own hands.
The Bottom Line
A recent study looked at nutrient inadequacies across the globe. It reported the following nutrient intakes were inadequate for more than 50% of the world’s population:
- Iodine, 68%.
- Vitamin E, 67%.
- Calcium, 66%.
- Iron, 65%.
- Riboflavin, 55%.
- Folate, 54%.
- Vitamin C, 53%.
- Vitamin B6, 51%.
The authors concluded, “These findings show empirically that most of the global population has inadequate intake of at least one nutrient…Estimates of inadequate global micronutrient intakes [like this one] can help public health researchers and practitioners to identify which age and sex groups in which countries might be in greatest need of intervention for which micronutrients.”
For more details on this study, nutrient inadequacies in the United States, and what this means for you read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
_____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.