What Do These Recommendations Mean For Non-Athletes?
Author: Dr. Stephen Chaney
 I have been following the research on omega-3s for athletes. But I have been reluctant to review that research in “Health Tips From the Professor” because:
I have been following the research on omega-3s for athletes. But I have been reluctant to review that research in “Health Tips From the Professor” because:
- Most of the studies are small.
- Each study measures the effect of omega-3 supplementation on different aspects of exercise and fitness.
- The dose of omega-3s used in the studies varies widely.
- To the casual observer, the studies appear to come to conflicting conclusions.
I have been waiting for a respected organization to do an in-depth analysis of the published studies before commenting. The International Society of Sports Nutrition (ISSN) has just published such a study (R Jager et al, Journal of the International Society of Sports Nutrition, Issue 22 (1), 2441775, 2025) and have provided a position statement on the use of omega-3 supplements by athletes and active adults.
I would add that the ISSN is regarded as a trusted source of nutrition information for athletes.
Do Omega-3s Benefit Athletes?
 The position of the ISSN is summarized below. What I like is they give the best recommendations based on current data and summarize the strength of the data behind each recommendation.
The position of the ISSN is summarized below. What I like is they give the best recommendations based on current data and summarize the strength of the data behind each recommendation.
Statement 1: Athletes may be at higher risk of omega-3 insufficiency, and diets rich in omega-3s, including supplements, are effective for increasing omega-3 levels. In this category, they reported three key findings:
- Omega-3s (ie EPA and DHA) are conditionally essential nutrients.
- Fatty fish and omega-3 supplements are both effective in raising omega-3 levels.
- Athletes belong to the groups at higher risk of omega-3 inadequacy.
My Comments:
-
- This conclusion was primarily based on studies with Division I college football players. More research is needed for high-level athletes in other sports.
-
- The reason for this omega-3 insufficiency was not discussed. However, I suspect it has to do with the recognition that high-level athletes need extra protein, and that fish is not usually included as a recommended source of additional protein for athletes.
-
- The average Omega-3 Index for the football players was 4.4% which is considered at high risk for heart disease. The authors of the ISSN report noted that previous studies have shown that around 1.4 g/day of EPA + DHA is recommended to increase the Omega-3 Index to an optimal 8%.
Statement 2: Omega-3 supplementation, particularly EPA and DHA, has been shown to enhance  endurance capacity and cardiovascular function during aerobic-type exercise. In this category, they reported three key findings:
endurance capacity and cardiovascular function during aerobic-type exercise. In this category, they reported three key findings:
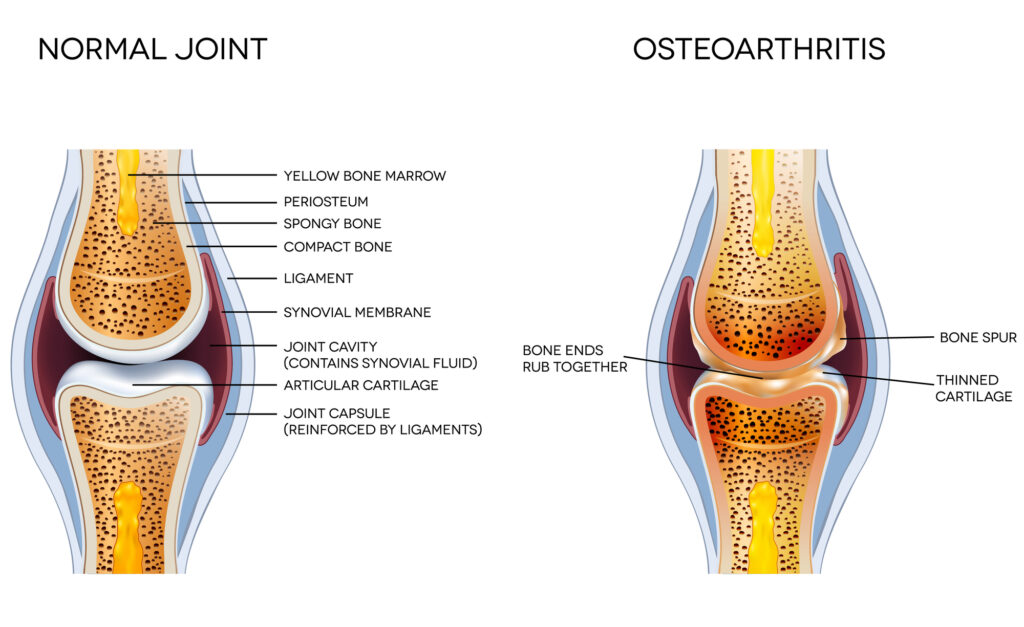
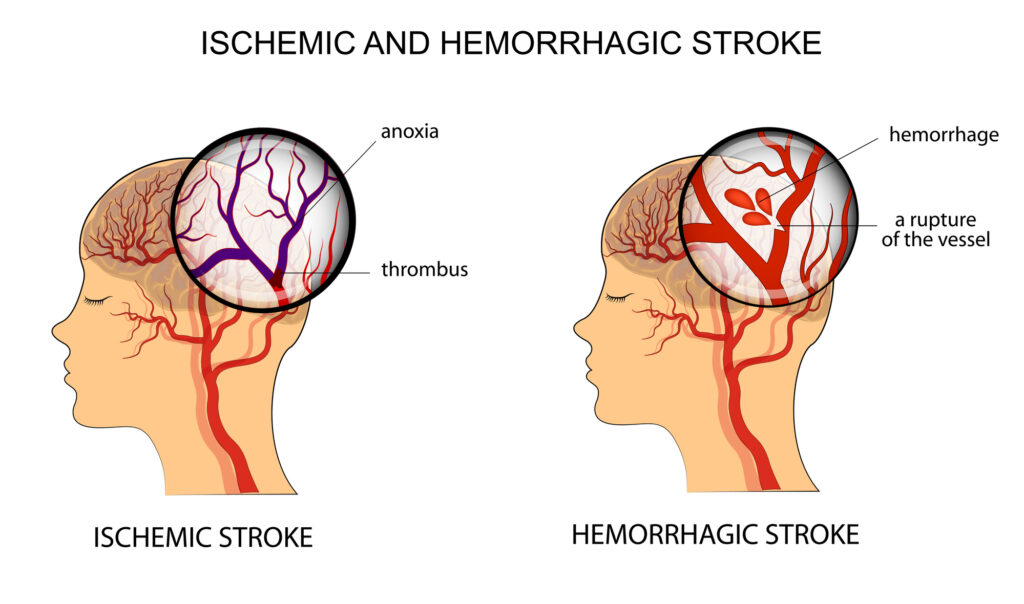
- Omega-3s can improve cardiovascular dynamics during and after exercise as evidenced by enhanced red blood cell deformability, endothelial function, and heart rate recovery after exercise.
- The incorporation of omega-3s into skeletal muscle membranes has been found to result in changes in muscle omega-3 composition, particularly in the sarcolemma, which is essential for muscle remodeling and/or regeneration after endurance exercise.
- While these changes may help the heart pump more efficiently during exercise and muscle recover quicker after exercise, their direct impact on endurance performance remains inconsistent. More studies are needed.
My Comments:
-
- These studies should be interpreted through the lens of your desired outcome. High-intensity exercise is hard on the heart.
-
- If your goal is increased endurance the role of omega-3s is uncertain.
-
- If your goal is to have your heart operate more efficiently during aerobic exercise, omega-3 supplementation may be beneficial.
 Statement 3: Omega-3 supplementation in combination with resistance training may improve strength in a dose- and duration-dependent manner. Specifically, they reported.
Statement 3: Omega-3 supplementation in combination with resistance training may improve strength in a dose- and duration-dependent manner. Specifically, they reported.
- The incorporation of omega-3s into muscle cells may take a minimum of four weeks, and this is dose-dependent. It takes longer to optimize the omega-3 content in muscle cells at lower doses.
- Once the omega-3 content of muscle cells has been optimized, it may take another three to six months until the improvement in strength plateaus.
My Comment:
-
- In short, don’t expect immediate results, but omega-3 supplementation may help increase muscle strength over the long haul.
Statement 4: Omega-3 supplementation may not confer a hypertrophic benefit in young adults. [In plain English they are saying that omega-3s may not stimulate any increase in muscle mass beyond that due to exercise alone for young adults.] They went on to say:
- More high-quality research is warranted to investigate the effects of omega-3 supplementation on body composition.
My Comments:
-
- We need to remember that the ISSN recommendations are for serious athletes and may not apply to the rest of us.
-
- For example, the authors state that omega-3 supplementation may enhance an increase in muscle mass…
-
-
- When protein intake is suboptimal.
-
-
-
- For older adults who are experiencing age-related loss of muscle mass.
-
-
-
- For people who have previous been inactive and are just beginning an exercise program.
-
-
- In other words, omega-3 supplements may help a lot of us non-athletes who are exercising to retain or increase muscle mass and strength.
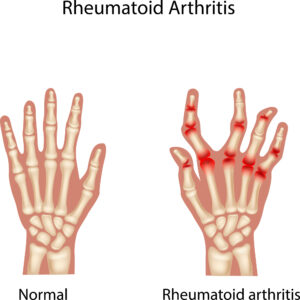
 Statement 5: Omega-3 supplementation may decrease subjective measures of muscle soreness following intensive exercise. In this category, they reported three key findings:
Statement 5: Omega-3 supplementation may decrease subjective measures of muscle soreness following intensive exercise. In this category, they reported three key findings:
- Omega-3 supplementation may attenuate indirect measures of muscle damage following intense exercise.
-
- For example, when muscles are damaged, they release muscle-specific enzymes such as creatine kinase and lactate dehydrogenase into the blood. Some studies have shown that omega-3s reduce the release of these muscle enzymes following intense exercise.
- Omega-3 supplementation is equivocal in decreasing subjective measures of muscle soreness following intense exercise.
- Omega-3 supplementation does not decrease measures of inflammation following exercise-induced muscle damage.
My Comments:
-
- Don’t count on omega-3 supplementation for reducing muscle soreness. But if you experience a decrease in muscle soreness, count it as an unexpected side benefit.
-
- The lack of an effect of omega-3s at reducing inflammation post exercise may be a good thing. Some experts think that the inflammatory response plays a role in stimulating muscle repair following exercise.
Statement 6: Omega-3 supplementation can positively affect various immune cell responses in athletic populations. In this category, they reported three key findings:
- Many athletes develop a compromised immune system due to the stress of high training volumes, which can increase the likelihood of developing acute respiratory infections that negatively impact their ability to train and compete.
- Omega-3 supplementation can affect various immune cell responses in non-athlete, clinical, and athletic populations.
- Many clinical studies conducted in athletic populations have indicated that omega-3 supplementation can influence the production and regulation of various inflammatory cytokines, which may lead to physiological benefits for the athletes [An example would be a reduction in exercise-induced asthma].
My Comments:
-
- These recommendations are based on the effect of omega-3s on blood markers of immune health and inflammation. Clinical studies looking at the effect of omega-3s on exercise-induced respiratory infections or asthma are either nonexistent or conflicting.
-
- So, if you experience decreased respiratory infections or exercise induced asthma when you add omega-3s to your exercise regimen, consider it an unexpected side benefit.
 Statement 7: Omega-3 supplementation may offer neuroprotective benefits in athletes exposed to repeated head impacts. In this category, they reported three key findings:
Statement 7: Omega-3 supplementation may offer neuroprotective benefits in athletes exposed to repeated head impacts. In this category, they reported three key findings:
- Omega-3s are crucial for optimal brain development and functioning.
- Omega-3 supplementation can increase membrane fluidity, neurotransmitter synthesis and release, and cerebral blood flow.
- In humans, a limited amount of evidence suggests that omega-3 supplementation may offer neuroprotective benefits in athletes following repeated head impacts.
My Comments:
- This is an important recommendation. Long-term cognitive decline, associated with repetitive traumatic brain injuries, is a serious concern for many high-impact sports. And there are no established protocols to prevent cognitive decline from occurring.
- I have covered this in more detail in a previous issue of “Health Tips From the Professor”.
Statement 8: Omega-3 supplementation is associated with improved sleep quality. In this category, they reported three key findings:
- Omega-3 supplementation has been linked to improved sleep quality in some studies.
- Omega-3 supplementation may help sleep quality due to anti-inflammatory properties and effects on neurotransmitters like dopamine and serotonin, a precursor of melatonin, which helps regulate sleep-wake cycles.
- However, inconsistency of results indicates more research is needed to fully understand the relationship between omega-3 supplementation and sleep.
My Comment:
- If you experience improved sleep when you add omega-3s to your exercise regimen, consider it an unexpected side benefit.
Summary Of ISSN Recommendations
 A strength of the ISSN recommendations is that they acknowledge where there is good agreement in the studies supporting their recommendations and where the data are scanty or conflicting. Based on the studies behind each recommendation, I would divide their recommendations into three categories.
A strength of the ISSN recommendations is that they acknowledge where there is good agreement in the studies supporting their recommendations and where the data are scanty or conflicting. Based on the studies behind each recommendation, I would divide their recommendations into three categories.
#1: Recommendations backed by a limited number of strong studies. Confidence in these recommendations can be improved with more studies, but the recommendations are strong. These include:
- Statement 1: Athletes are at higher risk of omega-3 insufficiency, and diets rich in omega-3s, including supplements, are effective for increasing omega-3 levels.
- Statement 4: Omega-3 supplementation in combination with resistance training may improve strength in a dose- and duration-dependent manner.
#2: Recommendations where the evidence is weak for athletes, but valuable for non-athletes. I will discuss those in more detail below. These include:
- Statement 2: Omega-3 supplementation has been shown to enhance endurance capacity and cardiovascular function during aerobic-type exercise.
- Statement 3: Omega-3 supplementation may not confer a muscle hypertrophic benefit [increase in muscle mass] in young adults.
#3: Recommendations that are weak and/or conflicting. These fall in the category of “don’t count on it. But if you do experience it, consider it an unexpected side-benefit of omega-3 supplementation”. These include”
- Statement 5: Omega-3 supplementation may decrease subjective measures of muscle soreness following intense exercise.
- Statement 6: Omega-3 supplementation can positively affect various immune cell responses in athletic populations.
- Statement 8: Omega-3 supplementation is associated with improved sleep quality.
Finally, the effect of omega-3 supplementation on preventing the cognitive consequences of repeated head trauma (Statement 7) is a very important topic. I have covered this in more detail in a previous issue of “Health Tips From the Professor”.
What Do These Recommendations Mean For Non-Athletes?
 As their name (International Society of Sports Nutrition) suggests, their recommendations are meant primarily for athletes. But what about those of us who are not athletes but work out on a regular basis for fitness, weight management, maintaining muscle mass as we age, or other reasons?
As their name (International Society of Sports Nutrition) suggests, their recommendations are meant primarily for athletes. But what about those of us who are not athletes but work out on a regular basis for fitness, weight management, maintaining muscle mass as we age, or other reasons?
In general, the recommendations apply equally well for athletes and non-athletes with a couple of caveats:
1) Dosage: Some of the studies with athletes were done with 3 to 6 grams/day of omega-3s. However, in most cases similar results were obtained 1-2 grams/day. Since 1-2 grams/day is enough to increase omega-3 levels to optimal for 90% of the population, I would recommend this dosage rather than the higher doses used in some of the studies with athletes.
2) Different Priorities for athletes and non-athletes: As I described earlier, this applies to two of the ISSN recommendations, namely:
- Statement 2: Omega-3 supplementation has been shown to enhance endurance capacity and cardiovascular function during aerobic-type exercise. As I said above:
-
- Young athletes are primarily interested in endurance, and the evidence for an endurance benefit for omega-3 supplementation is weak.
-
- However, the rest of us are more interested in how efficiently our heart is functioning during high-intensity exercise, especially as we age. And the evidence for that benefit is strong.
- Statement 3: Omega-3 supplementation may not confer a hypertrophic muscle benefit [increase in muscle mass] in young adults.
-
- That is a true statement for young, high-performance athletes who are consuming high protein diets. For the rest of us, we need to remember the authors of the ISSN report stated that omega-3 supplementation may enhance an increase in muscle mass:
-
-
- When protein intake is suboptimal.
-
-
-
- For older adults who are experiencing age-related loss of muscle mass.
-
-
-
- For people who have previous been inactive and are just beginning an exercise program.
-
The Bottom Line
The International Society For Sports Nutrition (ISSN) is recognized as a trusted source of nutrition advice for athletes. They recently reviewed the literature on the value of omega-3 supplementation for athletes and released a position paper with eight statements (recommendations).
I have divided these recommendations into 3 categories:
- Recommendations backed by strong data.
- Recommendations backed by weak data.
- Recommendations that have different significance for high-performing athletes and the rest of us.
For more details about the ISSN recommendations and what they mean for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
______________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.