What Is A Mind-Healthy Lifestyle?
Author: Dr. Stephen Chaney
 Most of us look forward to our golden years – that mystical time when we will be free from the workday pressures and have more time to spend with friends and family doing the things we love.
Most of us look forward to our golden years – that mystical time when we will be free from the workday pressures and have more time to spend with friends and family doing the things we love.
But cognitive decline can cast a dark cloud over those expectations.
- By the age of 65, 11% of adults suffer from some degree of cognitive impairment.
- And by the age of 80 the percentage of adults suffering from cognitive impairment has increased to 26-30%, depending on which study you cite.
The results of cognitive decline can be devastating.
- First you start to lose the cherished memories of a lifetime.
- Then comes confusion and an inability to perform basic tasks and participate in your favorite activities.
- Eventually you may reach a stage where you no longer recognize the ones you love.
In short, cognitive decline can rob you of everything that makes you you.
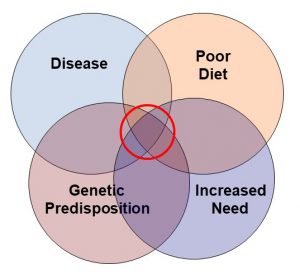
The causes of cognitive decline are complex, but recent studies have pointed to the role of chronic inflammation in cognitive decline. If that is true, it is a good news – bad news situation.
- The bad news is:
-
- Some increase in chronic inflammation appears to be an inevitable consequence of aging.
-
- Chronic inflammation can be caused by certain diseases that are beyond our control.
-
- Chronic inflammation can be triggered by viral or bacterial infections.
- The good news is that chronic inflammation is also controlled by your diet and lifestyle. For example, as I said above, chronic inflammation is often triggered by a viral infection, but whether the inflammation is mild or severe is strongly influenced by diet and lifestyle.
In this issue of “Health Tips From the Professor” I share a study (S Charisis et al, Neurology, In Press, November 10, 2021) showing that diets high in inflammatory foods increase the risk of dementia. Then, I answer 3 important questions.
- Can your diet cause you to lose your mind?
- What is a mind-healthy diet?
- What is a mind-healthy lifestyle?
How Was This Study Done?
 The data for this study were taken from the first three years of the Hellenic Longitudinal Investigation of Aging and Diet (HELIAD), a study designed to look at the effect of diet on dementia and other neuropsychiatric conditions in the Greek population.
The data for this study were taken from the first three years of the Hellenic Longitudinal Investigation of Aging and Diet (HELIAD), a study designed to look at the effect of diet on dementia and other neuropsychiatric conditions in the Greek population.
There were 1059 participants (40% male, average age = 75 at the beginning of the study) in this study. At the beginning of the study the participants completed a food frequency questionnaire administered by a trained dietitian. The foods were broken down into individual nutrients using the USDA Food Composition tables adapted for foods in the Greek diet.
The diet of each participant was then rated on a 15-point scale ranging from pro-inflammatory to anti-inflammatory based on something called the Diet Inflammation Index (DII).
Simply put, the DII is a validated assessment tool based on the effect of food nutrients on 6 inflammatory biomarkers found in the blood (IL-1β, IL-4, IL-6, IL-10, TNF-α, and CRP). Nutrients that decrease these markers are considered anti-inflammatory. Nutrients that increase these inflammatory biomarkers are considered pro-inflammatory.
For example, anti-inflammatory nutrients include:
- Carotenoids and flavonoids (found in fruits and vegetables).
- Omega-3 polyunsaturated fatty acids (found in cold-water fish, walnuts, flaxseeds, and chia seeds).
- Monounsaturated fatty acids (found in olive, avocado, and peanut oils).
- Fiber (found in minimally processed plant foods).
- Antioxidants, most B vitamins, and vitamin D.
- Magnesium and zinc.
- Garlic, onions, most herbs & spices.
Pro-inflammatory nutrients include:
- Refined carbohydrates.
- Cholesterol.
- Total fat.
- Saturated fats.
- Trans fats.
The participants were followed for 3 years, and all new diagnoses of dementia were recorded. The diagnoses were confirmed by a panel of neurologists and neuropsychologists.
Can Your Diet Cause You To Lose Your Mind?
 As described above, the diet of each participant in the study was rated on a 15-point DII (Diet Inflammatory Index) scale ranging from pro-inflammatory to anti-inflammatory. The association of the DII score of the participant’s diets with the onset of dementia was evaluated in two ways.
As described above, the diet of each participant in the study was rated on a 15-point DII (Diet Inflammatory Index) scale ranging from pro-inflammatory to anti-inflammatory. The association of the DII score of the participant’s diets with the onset of dementia was evaluated in two ways.
- Each one-point increase from an anti-inflammatory diet to a pro-inflammatory diet was associated with a 21% increase in the risk for dementia.
- In other words, even small changes in your diet can have a significant impact on your risk of developing dementia.
The investigators then divided the participants into three equal-sized groups based on the DII score of their diets.
- The group with the highest DII scores were 3 times more likely to develop dementia than the group with the lowest DII scores.
- In other words, a major change in your diet can have a major effect on your risk of developing dementia.
The authors concluded, “In the present study, higher DII scores (indicating greater pro-inflammatory diet potential) were associated with an increased risk for incident dementia [newly diagnosed dementia]. These findings may avail the development of primary dementia strategies through tailored and precise dietary interventions.”
What Is A Mind-Healthy Diet?
 This and other studies show that an anti-inflammatory diet is good for the mind. It helps protect us from cognitive decline and dementia. But what does an anti-inflammatory diet look like?
This and other studies show that an anti-inflammatory diet is good for the mind. It helps protect us from cognitive decline and dementia. But what does an anti-inflammatory diet look like?
One hint comes from analyzing the diets of participants in this study:
- Those with the lowest DII scores (most-anti-inflammatory diets) consumed 20 servings of fruit, 19 servings of vegetables, 4 servings of beans or other legumes, and 11 servings of coffee or tea each week. That’s almost 3 servings of fruit and 3 servings of vegetables every day!
- Those with the highest DII scores (most pro-inflammatory diets) consumed only half as many fruits, vegetables, and legumes.
- In short, a diet rich in fruits, vegetables, and legumes is a good start.
I have described anti-inflammatory diets in more detail in a previous issue of “Health Tips From the Professor.” Let me summarize that article briefly.
Anti-inflammatory foods include:
- Colorful fruits and vegetables.
- Whole grains.
- Beans and other legumes.
- Nuts, olive oil, avocados, and other sources of monounsaturated fats.
- Fatty fish and other sources of omega-3 fatty acids.
- Herbs and spices.
Pro-inflammatory foods include:
- Refined carbohydrates, sodas, and sugary foods.
- Foods high in saturated fats including fatty and processed meats, butter, and high fat dairy products.
- Foods high in trans fats.
- French fries, fried chicken, and other fried foods.
- Foods you are allergic or sensitive food. For example, gluten containing foods are pro-inflammatory only if you are sensitive to gluten.
If your goal is to reduce chronic inflammation and keep your mind sharp as a tack as you age, you should eat more anti-inflammatory foods and less pro-inflammatory foods.
Of course, we don’t just eat random foods, we follow dietary patterns. It should be apparent from what I have  covered above that whole food, primarily plant-based diets are anti-inflammatory. This is true for diets ranging from vegan through semi-vegetarian, to the Mediterranean, DASH, and MIND diets.
covered above that whole food, primarily plant-based diets are anti-inflammatory. This is true for diets ranging from vegan through semi-vegetarian, to the Mediterranean, DASH, and MIND diets.
All these diets are anti-inflammatory and likely protect the brain from cognitive decline. However, the best evidence for brain protection is for the Mediterranean, DASH, and MIND diets.
- The Mediterranean and DASH diets have been shown to prevent cognitive decline in multiple studies.
- The MIND diet is a combination the Mediterranean and DASH diets that was specifically designed to prevent cognitive decline. It has been shown to cut the risk of developing Alzheimer’s disease in half.
What Is A Mind-Healthy Lifestyle?
 Diet is just one aspect of a holistic approach for reducing cognitive decline as we age. Other important factors include:
Diet is just one aspect of a holistic approach for reducing cognitive decline as we age. Other important factors include:
- Reduce excess body weight.
- Exercise regularly.
- Get adequate sleep.
- Reduce and/or manage stress.
- Eliminate smoking and reduce alcohol consumption.
- Socialize with friends and family who support you. Numerous studies have shown that a strong support network reduces dementia risk in the elderly.
- Keep your brain active. Work crossword puzzles. Learn new things. An active brain is forced to lay down new neural pathways.
The Bottom Line
Recent studies have suggested that chronic inflammation increases the risk of cognitive decline and dementia as we age. Some causes of chronic inflammation are beyond our control, but others, such as diet, we can control.
Recently, a precise scoring system called the Diet Inflammatory Index (DII) has been developed. This scoring system allows studies to look at the correlation between the inflammatory potential of the diet and cognitive decline.
A recent study enrolled 1,000 participants with an average age of 75 in a 3-year study to determine the impact of diet on cognitive decline. The association of the DII score of the participant’s diets with the onset of dementia was evaluated in two ways.
- Each one-point increase from an anti-inflammatory diet to a pro-inflammatory diet was associated with a 21% increase in the risk for dementia.
- In other words, even small changes in your diet can have a significant impact on your risk of developing dementia.
The investigators then divided the participants into three equal-sized groups based on the DII score of their diets.
- The group with the highest DII scores were 3 times more likely to develop dementia than the group with the lowest DII scores.
- In other words, a major change in your diet can have a major effect on your risk of developing dementia.
The authors concluded, “In the present study, higher DII scores (indicating greater pro-inflammatory diet potential) were associated with an increased risk for incident dementia [newly diagnosed dementia]. These findings may avail the development of primary dementia strategies through tailored and precise dietary interventions.”
For more details and a description of mind-healthy diets and a mind-healthy lifestyle read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.