Who Benefits Most From A Healthy Diet?
Author: Dr. Stephen Chaney
 Fad diets abound. High protein, low carb, low fat, vegan, keto, paleo – the list is endless. They all claim to be backed by scientific studies showing that you lose weight, lower your cholesterol and triglycerides, lower your blood pressure, and smooth out your blood sugar swings.
Fad diets abound. High protein, low carb, low fat, vegan, keto, paleo – the list is endless. They all claim to be backed by scientific studies showing that you lose weight, lower your cholesterol and triglycerides, lower your blood pressure, and smooth out your blood sugar swings.
They all claim to be the best. But any reasonable person knows they can’t all be the best. Someone must be lying.
My take on this is that fad diet proponents are relying on “smoke and mirrors” to make their diet look like the best. I have written about this before, but here is a brief synopsis:
- They compare their diet with the typical American diet.
-
- Anything looks good compared to the typical American diet.
-
- Instead, they should be comparing their diet with other weight loss diets. That is the only way we can learn which diet is best.
- They are all restrictive diets.
-
- Any restrictive diet will cause you to eat fewer calories and to lose weight.
-
- As little as 5% weight loss results in lower cholesterol & triglycerides, lower blood pressure, and better control of blood sugar levels.
Simply put, any restrictive diet will give you short-term weight loss and improvement in blood parameters linked to heart disease, stroke, and diabetes. But are these diets healthy long term? For some of them, the answer is a clear no. Others are unlikely to be healthy but have not been studied long term. So, we don’t know whether they are healthy or not.
What if you started from the opposite perspective? Instead of asking, “Is a diet that helps you lose weight healthy long term?”, what if you asked, “Can healthy eating help you lose weight?” The study (S Schutte et al, American Journal of Clinical Nutrition, 115: 1-18, 2022) I will review this week asked that question.
More importantly, it was an excellent study. It compared a healthy diet to an unhealthy diet with exactly the same degree of caloric restriction. And it compared both diets to the habitual diet of people in that area. This study was performed in the Netherlands, so both weight loss diets were compared to the habitual Dutch diet.
How Was The Study Done?
 This was a randomized controlled trial, the gold standard of clinical studies. The investigators recruited 100 healthy, abdominally obese men and women aged 40-70. At the time of entry into the study none of the participants:
This was a randomized controlled trial, the gold standard of clinical studies. The investigators recruited 100 healthy, abdominally obese men and women aged 40-70. At the time of entry into the study none of the participants:
- Had diabetes.
- Smoked
- Had a diagnosed medical condition.
- Were on a medication that interfered with blood sugar control.
- Were on a vegetarian diet.
The participants were randomly assigned to:
- A high-nutrient quality diet that restricted calories by 25%.
- A low-nutrient-quality diet that restricted calories by 25%.
- Continue with their habitual diet.
The study lasted 12 weeks. The participants met with a dietitian on a weekly basis. The dietitian gave them the foods for the next week and monitored their adherence to their assigned diet. They were advised not to change their exercise regimen during the study.
At the beginning and end of the study the participants were weighed, and cholesterol, triglycerides, and blood pressure were measured.
Can Healthy Eating Help You Lose Weight?
 To put this study into context, these were not healthy and unhealthy diets in the traditional sense.
To put this study into context, these were not healthy and unhealthy diets in the traditional sense.
- Both were whole food diets.
- Both included fruits, vegetables, low-fat dairy, and lean meats.
- Both restricted calories by 25%.
The diets were designed so that the “high-nutrient quality” diet had significantly more plant protein (in the form of soy protein), fiber, healthy fats (monounsaturated and omega-3 fats), and significantly less fructose and other simple sugars than the “low-nutrient-quality” diet.
At the end of 12 weeks:
- Participants lost significant weight on both calorie-restricted diets compared to the group that continued to eat their habitual diet.
-
- That is not surprising. Any diet that successfully restricts calories will result in weight loss.
- Participants on the high-nutrient quality diet lost 33% more weight than participants on the low-nutrient-quality diet (18.5 pounds compared to 13.9 pounds).
- Participants on the high-nutrient quality diet lost 50% more inches in waist circumference than participants on the low-nutrient-quality diet (1.8 inches compared to 1.2 inches).
-
- This is a direct measure of abdominal obesity.
When the investigators measured blood pressure, fasting total cholesterol levels, and triglyceride levels:
- These cardiovascular risk factors were significantly improved on both diets.
-
- Again, this would be expected. Any diet that causes weight loss results in an improvement in these parameters.
- The reduction in total serum cholesterol was 2.5-fold greater and the reduction in triglycerides was 2-fold greater in the high-nutrient quality diet group than in the low-nutrient-quality diet group.
- The reduction in systolic blood pressure was 2-fold greater and the reduction in diastolic blood pressure was 1.67-fold greater in the high-nutrient quality diet group than in the low-nutrient-quality diet group.
The authors concluded, “Our results demonstrate that the nutrient composition of an energy-restricted diet is of great importance for improvements of metabolic health in an overweight, middle-aged population. A high-nutrient quality energy-restricted diet enriched with soy protein, fiber, monounsaturated fats, omega-3 fats, and reduced in fructose provided additional health benefits over a low-nutrient quality energy-restricted diet, resulting in greater weight loss…and promoting an antiatherogenic blood lipid profile.”
In short, participants in this study lost more weight and had a better improvement in risk factors for heart disease on a high-nutrient-quality diet than on a low-nutrient-quality diet. Put another way, healthy eating helped them lose weight and improved their health.
Who Benefits Most From A Healthy Diet?
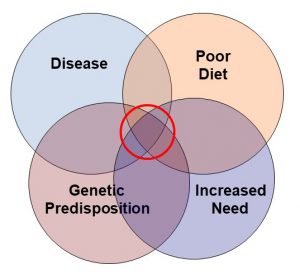
 None of the participants in this study had been diagnosed with diabetes when the study began. However, all of them were middle-aged, overweight, and had abdominal obesity. That means many of them likely had some degree of insulin resistance.
None of the participants in this study had been diagnosed with diabetes when the study began. However, all of them were middle-aged, overweight, and had abdominal obesity. That means many of them likely had some degree of insulin resistance.
Because of some complex metabolic studies that I did not describe, the investigators suspected that insulin resistance might influence the relative effectiveness of the two energy-restricted diets.
To test this hypothesis, they used an assay called HOMA-IR (homeostatic model assessment of insulin resistance). Simply put, this assay measures how much insulin is required to keep your blood sugar under control.
They used a HOMA-IR score of 2.5 to categorize insulin resistance among the participants.
- Participants with a HOMA-IR score >2.5 were categorized as insulin-resistant. This was 55% of the participants.
- Participants with a HOMA-IR score ≤2.5 were categorized as insulin-sensitive. This was 45% of the participants.
When they used this method to categorize participants they found:
- Insulin-resistant individual lost about the same amount of weight on both diets.
- Insulin-sensitive individuals lost 66% more weight on the high-nutrient-quality diet than the low-nutrient-quality diet (21.6 pounds compared to 13.0 pounds).
The investigators concluded, “Overweight, insulin-sensitive subjects may benefit more from a high- than a low-nutrient-quality energy-restricted diet with respect to weight loss…”
What Does This Study Mean For You?
 Simply put this study confirms that:
Simply put this study confirms that:
- Caloric restriction leads to weight loss, and…
- Weight loss leads to improvement in cardiovascular risk factors like total cholesterol, triglycerides, and blood pressure.
-
- This is not new.
-
- This is true for any diet that results in caloric restriction.
This study breaks new ground in that a high-nutrient quality diet results in significantly better:
- Weight loss and…
- Reduction in cardiovascular risk factors…
…than a low-nutrient quality diet. As I said above, the distinction between a “high-nutrient-quality” diet and a “low-nutrient-quality” diet may not be what you might have expected.
- Both diets were whole food diets. Neither diet allowed sodas, sweets, and highly processed foods.
- Both included fruits, vegetables, grains, and lean meats.
- Both reduced caloric intake by 25%.
-
- If you want to get the most out of your weight loss diet, this is a good place to start.
In this study the investigators designed their “high-nutrient-quality” diet so that it contained:
- More plant protein in the form of soy protein.
-
- In this study they did not reduce the amount of animal protein in the “high-nutrient-quality” diet. They simply added soy protein foods to the diet. I would recommend substituting soy protein for some of the animal protein in the diet.
- More fiber.
-
- The additional fiber came from substituting whole grain breads and brown rice for refined grain breads and white rice, adding soy protein foods, and adding an additional serving of fruit.
- More healthy fats (monounsaturated and omega-3 fats).
-
- The additional omega-3s came from adding a fish oil capsule providing 700mg of EPA and DHA.
- Less simple sugars. While this study focused on fructose, their high-nutrient-quality diet was lower in all simple sugars.
 All these changes make great sense if you are trying to lose weight. I would distill them into these 7 recommendations.
All these changes make great sense if you are trying to lose weight. I would distill them into these 7 recommendations.
- Follow a whole food diet. Avoid sodas, sweets, and highly processed foods.
- Include all 5 food groups in your weight loss diet. Fruits, vegetables, whole grains, dairy, and lean proteins all play an important role in your long-term health.
- Eat a primarily plant-based diet. My recommendation is to substitute plant proteins for at least half of your high-fat animal proteins. And this study reminds us that soy protein foods are a convenient and effective way to achieve this goal.
- Eat a diet high in natural fibers. Including fruits, vegetables, whole grains, beans, nuts, seeds, and soy foods in your diet is the best way to achieve this goal.
- Substitute healthy fats (monounsaturated and omega-3 fats) for unhealthy fats (saturated and trans fats) in your diet. And this study reminds us that it is hard to get enough omega-3s in your diet without an omega-3 supplement.
- Reduce the amount of added sugar, especially fructose, from your diet. That is best achieved by eliminating sodas, sweets, and highly processed foods from the diet. I should add that fructose in fruits and some healthy foods is not a problem. For more information on that topic, I refer you to a previous “Health Tips” article .
- Finally, I would like to remind you of the obvious. No diet, no matter how healthy, will help you lose weight unless you cut back on calories. Fad diets achieve that by restricting the foods you can eat. In the case of a healthy diet, the best way to do it is to cut back on portion sizes and choose foods with low caloric density.
I should touch briefly on the third major conclusion of this study, namely that the “high-nutrient quality diet” was not more effective than the “low-nutrient-quality” diet for people who were insulin resistant. In one sense, this was not news. Previous studies have suggested that insulin-resistant individuals have more difficulty losing weight. That’s the bad news.
However, there was a silver lining to this finding as well:
- Only around half of the overweight, abdominally obese adults in this study were highly insulin resistant.
-
- That means there is a ~50% chance that you will lose more weight on a healthy diet.
- Because both diets restricted calories by 25%, insulin-resistant individuals lost weight on both diets.
-
- That means you can lose weight on any diet that successfully reduces your caloric intake. That’s the good news.
-
- However, my recommendation would still be to choose a high-nutrient quality diet that is designed to reduce caloric intake, because that diet is more likely to be healthy long term.
The Bottom Line
A recent study asked, “Can healthy eating help you lose weight?” This study was a randomized controlled study, the gold standard of clinical studies. The participants were randomly assigned to:
- A high-nutrient quality diet that restricted calories by 25%.
- A low-nutrient-quality diet that restricted calories by 25%.
- Continue with their habitual diet.
These were not healthy and unhealthy diets in the traditional sense.
- Both were whole food diets.
- Both included fruits, vegetables, low-fat dairy, and lean meats.
- Both restricted calories by 25%.
The diets were designed so that the “high-nutrient quality” diet had significantly more plant protein (in the form of soy protein), fiber, healthy fats (monounsaturated and omega-3 fats), and significantly less fructose and other simple sugars than the “low-nutrient-quality” diet.
At the end of 12 weeks:
- Participants on the high-nutrient quality diet lost 33% more weight than participants on the low-nutrient-quality diet (18.5 pounds compared to 13.9 pounds).
When the investigators measured cardiovascular risk factors at the end of 12 weeks:
- The reduction in total serum cholesterol was 2.5-fold greater and the reduction in triglycerides was 2-fold greater in the high-nutrient quality diet group than in the low-nutrient-quality diet group.
- The reduction in systolic blood pressure was 2-fold greater and the reduction in diastolic blood pressure was 1.67-fold greater in the high-nutrient quality diet group than in the low-nutrient-quality diet group.
The authors concluded, “Our results demonstrate that the nutrient composition of an energy-restricted diet is of great importance for improvements of metabolic health in an overweight, middle-aged population. A high-nutrient quality energy-restricted diet enriched with soy protein, fiber, monounsaturated fats, omega-3 fats, and reduced in fructose provided additional health benefits over a low-nutrient quality energy-restricted diet, resulting in greater weight loss…and promoting an antiatherogenic blood lipid profile.”
In short, participants in this study lost more weight and had a better improvement in risk factors for heart disease on a high-nutrient-quality diet than on a low-nutrient-quality diet. Put another way, healthy eating helped them lose weight and improved their health.
For more details on this study, what this study means for you, and my 7 recommendations for a healthy weight loss diet, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.