The Promise And Problems Of Nutrigenomics
Author: Dr. Stephen Chaney
 When the human genome was sequenced in 2003, many of us in the scientific community thought we were on the verge of a revolution in human health and longevity. We would soon be able to tell individuals their risk of developing various diseases.
When the human genome was sequenced in 2003, many of us in the scientific community thought we were on the verge of a revolution in human health and longevity. We would soon be able to tell individuals their risk of developing various diseases.
Even better, we would be able to tell them the kind of diet and supplementation they needed to avoid those diseases. We would be able to personalize our nutritional recommendation for every individual based on their genome – something called nutrigenomics.
How naive we were! It has turned out to be much more complicated to design personalized nutrition recommendations based on someone’s genome than we ever imagined.
What Is Nutrigenomics?
 As a Professor at the University of North Carolina I specialized in cancer drug development for over 30 years. Over the last decade of my career a field called pharmacogenomics became widely accepted in the field of cancer drug development. In simple terms, pharmacogenomics looks at how an individual’s genes influence the effectiveness and side effects of drugs.
As a Professor at the University of North Carolina I specialized in cancer drug development for over 30 years. Over the last decade of my career a field called pharmacogenomics became widely accepted in the field of cancer drug development. In simple terms, pharmacogenomics looks at how an individual’s genes influence the effectiveness and side effects of drugs.
Because of pharmacogenomics, drugs today are being approved to target cancers for people whose cancer cells have a particular genetic makeup. These drugs would not have been approved a decades ago because if you test them on cancer in the general population, they have little or no effectiveness. They only work on a subset of people who have a form of cancer with a specific genetic makeup.
In principle, nutrigenomics is the same principle. You’ve heard for years that we all have unique nutritional needs. Now we are starting to learn why. It’s because we all have unique variations in our genetic makeup. These genetic mutations increase our risk of certain diseases, and they increase our needs for certain nutrients.
For example, mutations in the MTHFR gene increase the risk of certain birth defects, and supplementation with folic acid is particularly important for reducing birth defects in that population group.
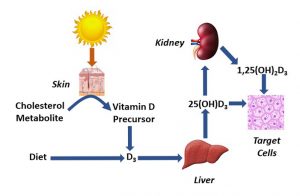
Similarly, mutations in the vitamin D receptor, the VDR gene, interfere with vitamin D absorption from foods and are associated with a condition known as “vitamin D-resistant rickets”. Babies born with this genetic defect require mega doses of vitamin D for normal bone formation.
These are the best-established examples of gene mutations that affect nutritional needs. Many more gene-nutrient interactions have been proposed, but they have not been validated by follow-up experiments.
The situation is similar when we look at gene mutations associated with metabolic responses such as fat and carbohydrate metabolism, obesity, insulin resistance and type 2 diabetes. There are a few gene mutations that have strong associations with obesity and diabetes. Many more gene-metabolism interactions have been proposed, but the data are weak and inconsistent.
The Promise And Problems Of Nutrigenomics
The Promise Of Nutrigenomics.
 Now that you understand what nutrigenomics is and have some background information about it, let’s look at the promise of nutrigenomics. One promise of nutrigenomics is personalized supplement programs.
Now that you understand what nutrigenomics is and have some background information about it, let’s look at the promise of nutrigenomics. One promise of nutrigenomics is personalized supplement programs.
We all have different nutritional needs. Wouldn’t it be wonderful if someone could analyze your genome and provide you with a personalized supplement program that precisely fits your genetically determined nutritional requirements?
There are companies that offer such personalized supplement programs. Are they providing you with something of value or is their testing bogus? Are their supplements worthless?
Another promise of nutrigenomics is personalized diet advice. Some people seem to do better on low-fat diets. Other people do better on low-carb diets. Saturated fats and red meats may be more problematic for some individuals than for others. Wouldn’t it be wonderful if someone could analyze your genome and provide you with a personalized diet program – one that allows you to lose weight easily and gain vibrant health.
There are companies that will analyze your genome and tell you whether you are more likely to lose weight and be healthier on a low-fat or low-carbohydrate diet. Is their testing accurate or is it bogus? Are they providing you with useful information, or is their diet advice worthless?
The Problem With Nutrigenomics
 The short answer to the questions I posed in the previous section is that personalized supplement and diet programs are on the horizon, but we are not there yet. Companies promising you personalized nutrition programs based only on DNA tests are misleading you. They quote a few studies supporting the tests they run and ignore the many studies showing their tests are worthless.
The short answer to the questions I posed in the previous section is that personalized supplement and diet programs are on the horizon, but we are not there yet. Companies promising you personalized nutrition programs based only on DNA tests are misleading you. They quote a few studies supporting the tests they run and ignore the many studies showing their tests are worthless.
In case you think that is just my opinion, let me quote from some recent reviews on the current status of nutrigenomics.
For example, a review (C Murgia and MM Adamski, Nutrients, 366, 2017) published in 2017 concluded: “The potential applications to nutrition of this invaluable tool were apparent since the genome was mapped. The first articles discussing nutrigenomics and nutrigenetics were published less than a year after the first draft of the human DNA sequence was made available…However, fifteen years and hundreds of publications later, the gap between the experimental and epidemiologic evidence and health practice is not yet closed.”
“The [complexity] of the genotype information is not the only factor that complicates this translation into practice. The discovery of other levels of control, including epigenetics [modifications of DNA that affect gene expression] and the intestinal microbiome, are other complicating factors. While the science of nutritional genomics continues to demonstrate potential individual responses to nutrition, the complex nature of gene, nutrition and health interactions continues to provide a challenge for healthcare professionals to analyze, interpret and apply to patient recommendations.”
Another review (M Gaussch-Ferre et al, Advances in Nutrition, 9: 128-135, 2018) published in 2018 concluded: “Overall, the scientific evidence supporting the dissemination of genomic information for nutrigenomic purposes remains sparse. Therefore, additional knowledge needs to be generated…”
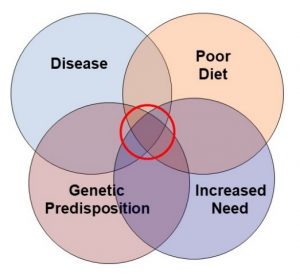
In short, the experts are saying we still don’t know enough to predict the best diets, or the best supplements based on genetic information alone. Why is that? Why is it so complicated? In part, it can be explained by a term called penetrance. Penetrance simply means that the same gene mutation can have different effects in different people. In some people, its effects may be barely noticeable. In other people its effects may be debilitating.
The Truth About DNA Testing And Personalized Nutrition
 Penetrance is just a word. It’s a concept. The important question is, “What causes differences in genetic penetrance?” Here are the most likely explanations.
Penetrance is just a word. It’s a concept. The important question is, “What causes differences in genetic penetrance?” Here are the most likely explanations.
1) Human genetics is very complex. There are some gene mutations, such as those causing cystic fibrosis and sickle cell anemia, that can cause a disease by themselves. Most gene mutations, however, simply predispose to a disease or metabolic disturbance and are highly influenced by the activity of other genes. That’s because the products of gene expression form intricate regulatory and metabolic networks. When a single gene is mutated, it interacts with many other genes in the network. And, that network is different for each of us.
2) Many common diseases are polygenic. That includes diseases like heart disease, diabetes, and most cancers. Simply put, that means that they are not caused by a single gene mutation. They are caused by the cumulative effect of many mutations, each of which has a small effect on disease risk. The same appears to be true for mutations that influence carbohydrate and fat metabolism and affect nutrient requirements.
3) The outcome of gene mutations is strongly influenced by our diet, lifestyle, and environment. For example, a common mutation in a gene called FTO predisposes to obesity. However, the effect of this mutation on obesity is strongest when it is coupled with inactivity and foods of high caloric density (translation: junk foods and fast foods instead of fresh fruits and vegetables). Simply put, that means most of us are genetically predisposed to obesity if we follow the American lifestyle, but obesity is not inevitable.
4) Epigenetics has an important influence on gene expression. When I was a graduate student, we believed our genetic destiny was solely determined by our DNA sequence. That was still the prevailing viewpoint when the human genome project was initiated. We thought that once we had our complete DNA sequence, we would know everything we needed to know about our genetic destiny.
How short sighted we were! It turns out that our DNA can be modified in multiple ways. These modifications do not change the DNA sequence, but they can have major effects on gene expression. They can turn genes on or turn them off. More importantly, we have come to learn that these DNA modifications can be influenced by our diet, lifestyle, and exposure to environmental pollutants.
This is the science we call epigenetics. We have gone from believing we have a genome (DNA sequence) that is invariant and controls our genetic destiny to understanding that we also have an “epigenome” (modifications to our DNA) that is strongly influenced by our diet, lifestyle, and environment and can change day-to-day.
 5) Our microbiome has an important influence on our health and nutritional status. Simply put, the term microbiome refers to our intestinal microbes. Our intestinal bacteria are incredibly diverse. Each of us has about 1,000 distinct species of bacteria in our intestines.
5) Our microbiome has an important influence on our health and nutritional status. Simply put, the term microbiome refers to our intestinal microbes. Our intestinal bacteria are incredibly diverse. Each of us has about 1,000 distinct species of bacteria in our intestines.
Current evidence suggests these intestinal bacteria influence our immune system, inflammation and auto-immune diseases, brain function and mood, and our predisposition to weight gain – and this may just be the tip of the iceberg.
More importantly, our microbiome is influenced by our diet. For example, vegetarians and meat eaters have entirely different microbiomes. Furthermore, the effect of diet on our microbiome is transitory. If you change your diet, the species of bacteria in your microbiome will completely change in a few weeks.
Finally, our microbiome also influences our nutritional requirements. For example, some species of intestinal bacteria are the major source of biotin and vitamin K2 for all of us and the major source of vitamin B12 for vegans. Intestinal bacteria may also contribute to our supply of folic acid and thiamine. Other intestinal bacteria inactivate and/or remove some vitamins from the intestine for their own use. Thus, the species of bacteria that populate our intestines can influence our nutritional requirements.
Now that you know the complexity of gene interactions you understand why we are not ready to rely on DNA tests yet. We don’t yet know enough to design a simple DNA test to predict our unique nutritional needs. That science is at least 10-20 years in the future. Companies that tell you otherwise are lying to you.
What Role Should DNA Testing Play In Nutritional Recommendations?
 The algorithms that are most successful in creating personalized diet and/or supplement recommendations:
The algorithms that are most successful in creating personalized diet and/or supplement recommendations:
1) Start with an analysis of your diet and lifestyle. They powerfully affect both gene expression and your microbiome.
2) Add in health parameters such as blood pressure, LDL cholesterol, HDL cholesterol, triglycerides, and hemoglobin A1c (a measure of blood sugar control). For example, a DNA analysis may suggest you are at risk for having elevated cholesterol, but whether you do or not is influenced by many other factors. A simple blood test indicates whether that risk is real for you.
3) Consider your personal health goals. If nutritional recommendations are to be personalized to you, they should emphasize the health goals you value most.
4) Include any diseases you have and recommendations of your doctor. If your doctor has recommended you lower your blood pressure, your cholesterol, or blood sugar levels, that is valuable information to include in the mix.
5) Now you are ready to include DNA testing in the mix. It can provide some valuable insights, but those insights need to be filtered through the lens of all the critical information collected in the first four steps. Genetics gives you possibilities. The information collected in the first four steps represents your realities.
The Bottom Line
Nutrigenomics is defined as the interaction between our genetic makeup and our diet. How far have we advanced in the science of nutrigenomics? Can a simple DNA test provide us with useful information?
For example, we all have different nutritional needs. Wouldn’t it be wonderful if someone could analyze your genome and provide you with a personalized supplement program that precisely fits your genetically determined nutritional requirements?
There are companies that will analyze your genome and offer personalized supplement programs. Are they providing you with something of value or is their testing bogus? Are their supplements worthless?
There are companies that will analyze your genome and tell you whether you are more likely to lose weight and be healthier on a low-fat or low-carbohydrate diet. Is their testing accurate or is it bogus? Are they providing you with useful information, or is their diet advice worthless?
Two recent reviews have surveyed the nutrigenomic literature (all published clinical studies) and have concluded that we still don’t know enough to predict the best diets, or the best supplements based on genetic information alone. Why is that? It is because:
1) Human genetics is very complex.
2) Many common diseases are polygenic (caused by the cumulative effect of many mutations).
3) The effect of gene mutations on our health and wellbeing is strongly influenced by our diet, lifestyle, and environment.
4) Epigenetics has an important influence on gene expression.
5) Our microbiome has an important influence on our health and nutritional status.
For more details on these studies and the kind of testing that best determines the right diet and/or supplement program for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.