Have The Dangers Of Eggs Been “Eggagerated”?
 It’s no wonder you are confused about whether or not eggs are good for you. The advice you have been given about eggs over the years has been constantly changing.
It’s no wonder you are confused about whether or not eggs are good for you. The advice you have been given about eggs over the years has been constantly changing.
Eggs are an affordable source of high-quality protein, iron, unsaturated fats, phospholipids like lecithin and choline, and carotenoids. That almost qualifies them as a health food. However, they are also a major source of cholesterol in the American diet. Back when we thought of dietary cholesterol was bad for us, that made eggs the enemy.
Then we discovered that dietary cholesterol has relatively little effect on blood cholesterol levels. It was obesity plus saturated fat and sugar in our diet that raised blood cholesterol levels and increased our risk of heart disease.
Then several studies reported that eggs did not increase our risk of heart disease. A study out of China even found that eggs decreased the risk of heart attack and hemorrhagic stroke. Suddenly, eggs became our best friend.
That only lasted a few years until a study from the United States reported that eggs increased your risk of heart disease, and a study from Europe reported that eggs increased your risk of hemorrhagic stroke. Eggfusion (egg confusion) reigned.
Most of these studies were large studies. They followed their participants for 5-10 years. Why were their results so confusing? A careful analysis of the studies shows that most of them suffered from three major weaknesses.
- They only measured egg consumption at the beginning of the study. This fails to account for the fact that egg consumption has waxed and waned over the years as eggs have gone from enemy to friend and back to enemy.
- They did not assess how the overall diet influences the effect of egg consumption on heart disease. If we believe the previous studies, eggs lower the risk of heart disease and hemorrhagic stroke in China and increase the risk of both in the United States and Europe. This suggests that overall diet is important, but this hypothesis has not been tested.
- They also did not address the question of whether eggs, because of their cholesterol, might have a more adverse effect on heart disease in individuals who already have high blood cholesterol and have difficulty controlling their cholesterol levels.
That is why the study (JP Drouin-Chartier et al, British Medical Journal, 368:m513, 2020) I am reporting on today is so important. It is a huge study, much larger than any previous study on the topic. Plus, it was designed in such a way that it had none of the weaknesses of previous studies.
How Was The Study Done?
 This study started by combining the data from three major clinical trials:
This study started by combining the data from three major clinical trials:
- The first Nurse’s Health Study, which ran from 1980 to 2012,
- The second Nurse’s Health Study, which ran from 1991-2013, and
- The Health Professional’s Follow-Up Study, which ran from 1986-2012.
These studies combined enrolled 173,563 women and 42,055 men and followed them for an average of 32 years. All the participants were free of heart disease, type 2 diabetes, and cancer at the time they were enrolled. The design of these studies was extraordinary.
- A detailed food frequency questionnaire was administered every 2-4 years. This allowed the investigators to calculate cumulative averages of all dietary variables, including egg intake. This assured that the effects of egg consumption and diet represented the participant’s diet over the 32-year duration of the study.
- Participants also filled out questionnaires that captured information on disease diagnosis, disease risk factors, medicines taken, weight, and lifestyle characteristics every 2 years with follow-up rates >90%. This allowed the investigators to measure the onset of disease and medicine use for each participant during the study. More importantly, 32 years is long enough to measure the onset of diseases like heart disease, diabetes, and cancer – diseases that require decades to develop.
- The endpoint of the study was “incident heart disease”, which the investigators defined as non-fatal heart attack, death from heart disease, and fatal and non-fatal stroke. During this study, 14,806 participants developed incident heart disease. This was a large enough number for a detailed statistical analysis of the data.
- For example, statistical analysis showed that the participants with the highest egg intake also were more likely to be obese and more likely to consume red meat, bacon and other processed meats, refined grains, French fries, and sugar-sweetened beverages. These are what we refer to as “confounding variables” because they also increase the risk of heart disease and are likely to confound (confuse) the analysis. Therefore, the investigators statistically corrected the data on egg consumption for these confounding variables. Many previous studies did not have the data or statistical power to correct their egg consumption data for these confounding variables.
In short, this study was much larger, ran far longer, and was better designed that any of the previous studies on egg consumption and heart disease risk. However, the authors did not stop there. They also performed a meta-analysis of 28 previous studies with a total of 1,720,108 participants and 139,195 cardiovascular disease events.
The only weakness in this study is that only 2% of the participants ate more than one egg per day. Consequently, it cannot address the health consequences of eating more than one egg per day on a regular basis.
Before sharing the results of this study with you, I need to provide some background about how our bodies regulate blood cholesterol levels. So, let’s move on to my favorite topic, “Biochemistry 101”.
Biochemistry 101: Cholesterol Metabolism
 Most people think of cholesterol only as a bad thing – something that can kill us. Nothing could be further from the truth. In fact, cholesterol is essential for life.
Most people think of cholesterol only as a bad thing – something that can kill us. Nothing could be further from the truth. In fact, cholesterol is essential for life.
- Our body makes vitamin D and coenzyme Q10 from cholesterol.
- Our body makes steroid hormones such as cortisol, estrogen, and testosterone from cholesterol.
- Cholesterol is a vital component of the myelin sheath that coats our nerve cells.
- And that is just the beginning.
Because cholesterol is essential, our body makes its own cholesterol and has an elegant control system that keeps our blood cholesterol levels right where they should be.
- When we get lots of cholesterol from our diet, our body makes less and excretes any excess.
- When we get little cholesterol from our diet, our body makes more and excretes less.
Unfortunately, many Americans muck up this elegant control system. There are several factors that can throw our body’s ability to regulate blood cholesterol levels out of whack, leading to elevated blood cholesterol levels and increased risk of heart disease. For example:
- Obesity
- Type 2 diabetes
- Diets high in saturated fats
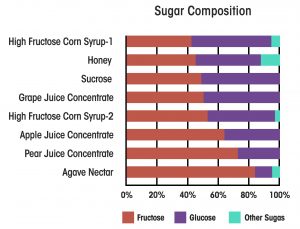
- Diets high in sugar and refined carbohydrates
- Genetics
And it’s not just elevated cholesterol that is the problem. These same factors are associated with inflammation, which also increases the risk of heart disease.
Of course, we can’t do anything about our genetics, but the other factors are under our control. Let’s keep that in mind as we look at the results of this study.
What Is The Truth About Eating Eggs And Heart Disease?
 When the investigators looked at their combined data from the Nurse’s Health Studies and the Health Professional’s Study:
When the investigators looked at their combined data from the Nurse’s Health Studies and the Health Professional’s Study:
- There was no difference in heart disease outcomes for participants consuming an average of one egg/day and participants consuming less than one egg/month.
- When the investigators examined heart attack and stroke separately, there was no difference in either outcome for participants consuming an average of one egg/day and participants consuming less than one egg/month.
- As mentioned above the participants who consumed the most eggs weighed more; were less physically active; were more likely to be current smokers; and were more likely to consume red meat, processed meats, refined grains, potatoes (think French fries and potato chips), full fat milk, and sugar-sweetened beverages.
-
- Without correcting for these factors eating one egg/day resulted in a 10% increase in heart disease risk.
-
- After correcting for these factors, eating one egg/day resulted in a 7% decrease in heart disease risk.
-
- In both cases the differences were statistically non-significant. However, they were in line with the previous studies mentioned above.
When they looked at the data generated by their meta-analysis of 28 studies:
- There was no association between heart disease risk and egg consumption.
-
- In Asian countries where the diet was primarily unrefined, plant-based foods, egg consumption decreased heart disease risk.
-
- In people with type 2 diabetes, egg consumption increased heart disease risk.
The authors concluded “…moderate egg consumption (up to one egg/day) is not associated with cardiovascular disease risk overall, and is associated with potentially lower cardiovascular disease risk in Asian populations.”
The authors also noted that their data did not allow them to evaluate the effect of consuming more than one egg/day.
Have The Dangers Of Eggs Been “Eggagerated”?
 This study clears up a lot of confusion about egg consumption and heart disease risk. The problem is that the scientific and medical communities have been looking for a “one size fits all” recommendation about egg consumption. This study shows us that the reality is much more complicated. Let me describe my interpretation of the data.
This study clears up a lot of confusion about egg consumption and heart disease risk. The problem is that the scientific and medical communities have been looking for a “one size fits all” recommendation about egg consumption. This study shows us that the reality is much more complicated. Let me describe my interpretation of the data.
I think the results of this and previous studies are best described by the phrase, “Eggs are a healthy part of a healthy diet”. Here is what I mean by that.
- If you are consuming a primarily plant-based diet, your body is fully able to regulate your blood cholesterol levels. Then, you can reap the full benefits of the egg, namely the protein, iron, unsaturated fats, lecithin, choline, and carotenoids it provides. Under these conditions, eating up to one egg/day reduces your risk of heart disease.
- If you are consuming a diet that contains primarily chicken or fish and unprocessed plant foods, egg consumption is neutral. It neither increases nor decreases your risk of heart disease.
- If you are consuming a diet that contains sugar-sweetened beverages, red and processed meats, high fat dairy products, refined grains, and junk foods (ie, the typical American diet), your body is no longer able to regulate blood cholesterol levels well. Now the cholesterol content of eggs becomes an issue and consuming one egg/day slightly increases your risk of heart disease.
- If you are overweight and have developed type 2 diabetes, your body has become insulin resistant. This also interferes with your body’s ability to regulate blood cholesterol levels. In this situation, consuming one egg/day also increases your risk of heart disease.
The caveat is, of course, that these conclusions are based averages, and none of us are average.
The Bottom Line
You are probably aware that the effect of egg consumption on heart disease risk is controversial. Some studies report that egg consumption has no effect on heart disease risk. Other studies report egg consumption decreases heart disease risk. Still other studies report that egg consumption increases heart disease risk. No wonder you are confused.
A recent study has cleared up much of the confusion. This was not just another study. This study was much larger, ran far longer, and was better designed that any of the previous studies.
If you look at this and previous studies, it becomes clear that the effect of egg consumption on heart disease risk is strongly influenced by your overall diet and lifestyle.
- If you are consuming a primarily plant-based diet, your body is fully able to regulate your blood cholesterol levels. Then, you can reap the full benefits of the egg, namely the protein, iron, unsaturated fats, lecithin, choline, and carotenoids it provides. Under these conditions, eating up to one egg/day reduces your risk of heart disease.
- If you are consuming a diet that contains primarily chicken or fish and unprocessed plant foods, egg consumption is neutral. It neither increases nor decreases your risk of heart disease.
- If you are consuming a diet that contains sugar-sweetened beverages, red and processed meats, high fat dairy products, refined grains, and junk foods (ie, the typical American diet), your body is no longer able to regulate blood cholesterol levels well. Now the cholesterol content of eggs becomes an issue and consuming one egg/day slightly increases your risk of heart disease.
- If you are overweight and have developed type 2 diabetes, your body has become insulin resistant. This also interferes with your body’s ability to regulate blood cholesterol levels. In this situation, consuming one egg/day also increases your risk of heart disease.
In short, eggs are a healthy part of a healthy diet.
For more details, read the article above. You may also want to read the section “Biochemistry 101: Cholesterol Metabolism” to gain a better understanding of the mechanism behind these statements.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease