Are Nitrates Good For You Or Bad For You?
Author: Dr. Stephen Chaney
 We have known for years that fruits and vegetables are good for our hearts. We have assumed that was because whole fruits and vegetables are low in saturated fats and provide heart-healthy nutrients, phytonutrients, and fiber. But could there be more?
We have known for years that fruits and vegetables are good for our hearts. We have assumed that was because whole fruits and vegetables are low in saturated fats and provide heart-healthy nutrients, phytonutrients, and fiber. But could there be more?
Recent research has suggested that the nitrates found naturally in fruits and vegetables may also play a role in protecting our hearts. Here is what recent research shows:
- The nitrates from fruits and vegetables are converted to nitrite by bacteria in our mouth and intestines.
-
- Fruits and vegetables account for 80% of the nitrate in our diet. The rest comes from a variety of sources including the nitrate added as a preservative to processed meats.
-
- Although all fruits and vegetables contain nitrates, the best sources are green leafy vegetables and beetroot. [Beet greens are delicious and also a good source of nitrate, but beetroot is the part of the beet we usually consume.]
- Nitrite is absorbed from our intestine and converted to nitric oxide by a variety of enzymes in our tissues.
- Both reactions require antioxidants like vitamin C, which are also found in fruits and vegetables.
Nitric oxide has several heart healthy benefits. For example:
- It helps reduce inflammation in the lining of blood vessels. Inflammation stimulates atherosclerosis, blood clot formation, and is associated with an increased risk of heart disease.
- It relaxes the smooth muscle cells that surround our blood vessels. This makes the blood vessels more flexible and helps reduce blood pressure.
- It prevents smooth muscle cells from proliferating, which prevents them from invading and constricting our arteries. This, in turn, has the potential to reduce the risk of atherosclerosis.
- It prevents platelet aggregation. This, in turn, has the potential to reduce the risk of heart attack and stroke due to blood clots that block the flow of blood to our heart or brain.
It is well established that nitrates from fruits and vegetables reduce blood pressure. More importantly, they can help slow the gradual increase in blood pressure as we age.
However, few studies have asked whether this reduction in blood pressure translates into improved cardiovascular outcomes. This study (CP Bondonno et al, European Journal of Epidemiology, doi.org/10.1007/s10654-021-00747-3) was designed to answer that question.
How Was This Study Done?
 This study made use of data from the Danish Diet, Cancer, and Health Program. That program enrolled 53,150 participants from Copenhagen and Aarhus between 1993 and 1997 and followed them for an average of 21 years. None of the participants had a diagnosis of cancer or heart disease at the beginning of the study.
This study made use of data from the Danish Diet, Cancer, and Health Program. That program enrolled 53,150 participants from Copenhagen and Aarhus between 1993 and 1997 and followed them for an average of 21 years. None of the participants had a diagnosis of cancer or heart disease at the beginning of the study.
Other characteristics of the participants at the time they were enrolled in the study were:
- 46% male
- Average age = 56
- BMI = 26 (20% overweight)
- Average systolic blood pressure = 140 mg Hg
- Average diastolic blood pressure = 84 mg Hg
At the beginning of the study, participants filled out a 192-item food frequency questionnaire that assessed their average intake of various food and beverage items over the previous 12 months. The vegetable nitrate content of their diets was analyzed using a comprehensive database of the nitrate content of 178 vegetables. For those vegetables not consumed raw, the nitrate content was reduced by 50% to account for the nitrate loss during cooking.
Blood pressure was measured at the beginning of the study. Data on the incidence (first diagnosis) of heart disease during the study was obtained from the Danish National Patient Registry. Data were collected on diagnosis of the following heart health parameters:
- Cardiovascular disease (all diseases of the circulatory system).
- Ischemic heart disease (lack of sufficient blood flow to the heart). The symptoms of ischemic heart disease range from angina to myocardial infarction (heart attack).
- Ischemic stroke (lack of sufficient blood flow to the brain).
- Hemorrhagic stroke (bleeding in brain).
- Heart failure.
- Peripheral artery disease (lack of sufficient blood flow to the extremities).
Is Nitrate From Vegetables Good For Your Heart?
 Intake of nitrate from vegetables ranged from 18 mg/day (<1/3 serving of nitrate-rich vegetables per day) to 168 mg (almost 3 servings of nitrate-rich vegetables per day). The participants were grouped into quintiles based on their vegetable nitrate intake. When the group with the highest vegetable nitrate intake was compared to the group with the lowest vegetable nitrate intake:
Intake of nitrate from vegetables ranged from 18 mg/day (<1/3 serving of nitrate-rich vegetables per day) to 168 mg (almost 3 servings of nitrate-rich vegetables per day). The participants were grouped into quintiles based on their vegetable nitrate intake. When the group with the highest vegetable nitrate intake was compared to the group with the lowest vegetable nitrate intake:
- Systolic blood pressure was reduced by 2.58 mg Hg.
- Diastolic blood pressure was reduced by 1.38 mg Hg.
- Risk of cardiovascular disease was reduced by 14%.
- Risk of ischemic heart disease (angina and heart attack) was reduced by 13%.
- Risk of ischemic stroke (stroke caused by lack of blood flow to the brain) was reduced by 14%.
- Risk of heart failure was reduced by 17%.
- Risk of peripheral artery disease was reduced by 31%.
- Risk of hemorrhagic stroke (bleeding in the brain) was not significantly reduced.
Two other observations were of interest:
- Blood pressure and risk of peripheral artery disease decreased with increasing vegetable nitrate intake in a relatively linear fashion. However, the other parameters of heart disease plateaued at a modest intake of vegetable nitrate intake (around one cup of nitrate-rich vegetables per day). This suggests that as little as one serving of nitrate-rich vegetables a day is enough to provide some heart health benefits.
- Only about 21.9% of the improvement in heart health could be explained by the decrease in blood pressure. This is not surprising when you consider the other beneficial effects of nitric oxide described above.
The authors concluded, “Consumption of at least ~60 mg/day of vegetable nitrate (~ one serving of green leafy vegetables or beets) may mitigate risk of cardiovascular disease.”
Are Nitrates Good For You Or Bad For You?
 You are probably thinking, “Wait a minute. I thought nitrates and nitrites were supposed to be bad for me. Which is it? Are nitrates good for me or bad for me?”
You are probably thinking, “Wait a minute. I thought nitrates and nitrites were supposed to be bad for me. Which is it? Are nitrates good for me or bad for me?”
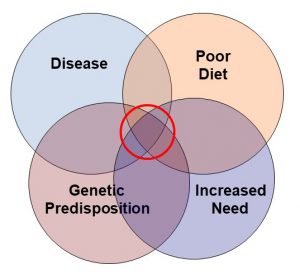
It turns out that nitrates and nitrites are kind of like Dr. Jekyll and Mr. Hyde. They can be either good or bad. It depends on the food they are in and your overall diet.
Remember the beginning of this article when I said that the conversion of nitrates to nitric oxide depended on the presence of antioxidants? Vegetables are great sources of antioxidants. So, when we get our nitrate from vegetables, most of it is converted to nitric oxide. And, as I discussed above, nitric oxide is good for us.
However, when nitrates and nitrites are added to processed meats as a preservative, the story is much different. Processed meats have zero antioxidants. And the protein in the meats is broken down to amino acids in our intestine. The amino acids combine with nitrate to form nitrosamines, which are cancer-causing chemicals. Nitrosamines are bad for us.
Of course, we don’t eat individual foods by themselves. We eat them in the context of a meal. If you eat small amounts of nitrate-preserved processed meats in the context of a meal with antioxidant-rich fruits and vegetables, some of the nitrate will be converted to nitric oxide rather than nitrosamines. The processed meat won’t be as bad for you.
What Does This Study Mean For You?
 Your mother was right. You should eat your fruits and vegetables!
Your mother was right. You should eat your fruits and vegetables!
- The USDA recommends at least 3 servings of vegetables and 2 servings of fruit a day.
- Based on this study, at least one of those servings should be nitrate-rich vegetables like green leafy vegetables and beets.
- If you don’t like any of those, radishes, turnips, watercress, Bok choy, Chinese cabbage, kohlrabi, chicory leaf, onion, and fresh garlic are also excellent sources of nitrate.
- The good news is that you may not need to eat green leafy vegetables and beets with every meal. If this study is correct, one serving per day may have heart health benefits. That means you can enjoy a wide variety of fresh fruits and vegetables as you try to meet the USDA recommendations.
Finally, if you don’t like any of those foods, you may be asking, “Can’t I just take a nitrate supplement?”
- For blood pressure, there are dozens of clinical trials, and the answer seems to be yes – especially when the nitrate comes from vegetable sources and the supplement also contains an antioxidant like vitamin C.
- For heart health benefits, the answer is likely to be yes, but clinical trials to confirm that would take decades. Double blind, placebo-controlled trials of that duration are not feasible, so we will never know for sure.
- Moreover, you would not be getting all the other health benefits of a diet full of fresh fruits and vegetables. Supplementation has its benefits, but it is not meant to replace a healthy diet.
The Bottom Line
We have known for years that fruits and vegetables are good for our hearts. We have assumed that was because whole fruits and vegetables are low in saturated fats and provide heart-healthy nutrients, phytonutrients, and fiber. But could there be more?
It is well established that nitrates from fruits and vegetables reduce blood pressure. More importantly, they can help slow the gradual increase in blood pressure as we age.
However, few studies have asked whether this reduction in blood pressure translates into improved cardiovascular outcomes. A recent study was designed to answer that question.
When the study compared people with the highest vegetable nitrate intake to people with the lowest vegetable nitrate intake:
- Blood pressure was significantly reduced.
- The risk of cardiovascular disease was reduced by 14%.
- Risk of ischemic heart disease (angina and heart attack) was reduced by 13%.
- Risk of ischemic stroke (stroke caused by lack of blood flow to the brain) was reduced by 14%.
- Risk of heart failure was reduced by 17%.
- Risk of peripheral artery disease was reduced by 31%.
- Blood pressure and risk of peripheral artery disease decreased with increasing vegetable nitrate intake in a relatively linear fashion.
- However, the other parameters of heart disease plateaued at a modest intake of vegetable nitrate intake (around one cup of nitrate-rich vegetables per day). This suggests that as little as one serving of nitrate-rich vegetables a day is enough to provide some heart health benefits.
The authors concluded, “Consumption of at least ~60 mg/day of vegetable nitrate (~ one serving of green leafy vegetables or beets) may mitigate risk of cardiovascular disease.”
Of course, you may have heard that nitrates and nitrites are bad for you. I discuss that in the article above.
For more details about this study, information about vegetable nitrate supplements, and what this study means for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.