Does Folic Acid Increase Cancer Risk?
Author: Dr. Stephen Chaney
 You’ve seen the headlines. “Folic Acid Supplements May Increase Colon Cancer Risk in People Over 50” and “Folic Acid Supplements May Increase Prostate Cancer Risk in Men”. And I’ve seen articles telling people over 50 that they should take their multivitamin tablets every other day to avoid getting too much folic acid.
You’ve seen the headlines. “Folic Acid Supplements May Increase Colon Cancer Risk in People Over 50” and “Folic Acid Supplements May Increase Prostate Cancer Risk in Men”. And I’ve seen articles telling people over 50 that they should take their multivitamin tablets every other day to avoid getting too much folic acid.
I’ve even heard of doctors telling their patients to avoid any supplements containing folic acid. So what’s the truth? Is there a cause and effect relationship between folic acid and cancer?
Why Do People Say Folic Acid Increases Colon Cancer Risk?
Perhaps a bit of historical perspective is in order. A number of population studies had suggested that high intakes of folic acid might protect against cancer, especially colon cancer, so several placebo controlled clinical studies were initiated to test that hypothesis. Those studies had mixed results, with some suggesting that folic acid might be protective and others suggesting that it had no effect. None of those studies suggested that folic acid supplementation increased the risk of any kind of cancer.
In 1998 mandatory folic acid fortification of grain products was introduced. In addition, the number of Americans taking supplements with folic has increased dramatically in recent years. As a consequence total intake of folates (folic acid from fortified foods and supplements plus folates naturally found in foods) has increased significantly. By one estimate blood levels of folates have increased 2.5-fold between 1994 (before fortification) and 2000 (after fortification).
So it was just natural to ask if this increase in folate intake might have unintended consequences. And one clinical study seemed to suggest that it might (JAMA, 297: 2351-2359, 2007)
That study looked at colorectal adenomas and reported high folate intake was associated with an increased risk of more advanced adenomas. [It is important to note that adenomas are benign tumors. They are thought to be precursors to colorectal cancer but they are not actually cancerous].
Some experts immediately started warning about getting too much folic acid in the diet – with some going so far as to warn that people over 50 should only take a multivitamin every other day.
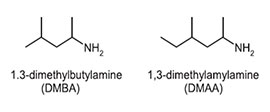
And several papers were published speculating on how differences between the way that folic acid and the other folates were utilized by the body could cause folic acid to increase the risk of colorectal cancer while naturally occurring folates decreased the risk.
Let me put this into perspective. Any good scientist knows not to trust a single clinical study. Individual clinical studies can provide misleading results. Sometimes it is possible to pinpoint the cause. For example, the study may have been poorly designed, may have included a non-representative population group, or the statistical analysis may have been incorrect. But, sometimes we never know why an individual clinical study came to the wrong conclusion.
 That is why good scientists generally say that more studies are needed and base their recommendation on the preponderance of many studies rather than a single study.
That is why good scientists generally say that more studies are needed and base their recommendation on the preponderance of many studies rather than a single study.
The problem was that all of this hype and hypothesizing about folic acid increasing the risk of colon cancer was based on a single study, and that study didn’t actually look at colorectal cancer. A Norwegian study four years later found no evidence for increased colorectal cancer at folic acid intakes of up to 800 ug/day (AJCN, 94: 1053-1062, 2011) – but it was largely ignored.
The background is similar for the claims that folic acid may increase prostate cancer risk. When a small meta-analysis that included some, but not all, published clinical studies suggested an increased risk of prostate cancer, some experts went as far as to suggest that men should completely avoid supplements with folic acid.
The problem is that even meta-analyses can be misleading if they only examine a small sub-set of clinical studies because they can be unduly influenced by a single misleading clinical study.
Does Folic Acid Increase Colon Cancer Risk?
Should We Avoid Supplemental Folate?
The American Cancer Society decided to resolve the uncertainty about folic acid intake and colon cancer risk once and for all (V.L. Stevens et al, Gastroenterology, 141: 98-105, 2011). They designed the study to answer two very important questions:
1) Has the increased folate intake by Americans over the past several years actually increased their risk for colorectal cancer?
2) Does the chemical form (folic acid versus folate) influence its effect on colorectal cancer risk?
And this study had two very important firsts:
1) This was the very first study to investigate the association between folate intake and colorectal cancer entirely in the post-fortification period.
2) This was also the very first study to separate out the effects of folate and folic acid on colorectal cancer risk.
And it was a very large study. They followed 43,512 men and 56,011 women aged 50-74 for 8 years between 1999 and 2007.
Folate intakes from food ranged from 175 ug/day to 354 ug/day while folic acid intakes from food fortification, supplements and multivitamins ranged from 71 ug/day to 660 ug/day. Total folate (both naturally occurring folates and folic acid) intakes ranged from 246 ug/day to over 1014 ug/day.
When they analyzed the data they found that high intakes of neither folic acid nor natural folates were associated with any increased risk of colorectal cancer. In fact, they found high intake of total folates was associated with a significant decreased risk of colorectal cancer.
Does Folic Acid Increase Cancer Risk?
 What about prostate cancer and other types of cancer? Could folic acid increase the risk of other cancers? To resolve this issue once and for all, a group from Oxford University (Clarke et al, The Lancet, doi: 10.1016/S0140-6736(12)62001-7) did a meta-analysis of every study published through 2010 that compared folic acid supplementation to a placebo, lasted at least 1 year, included at least 500 people and recorded cancer incidence – some 13 studies with over 50,000 participants.
What about prostate cancer and other types of cancer? Could folic acid increase the risk of other cancers? To resolve this issue once and for all, a group from Oxford University (Clarke et al, The Lancet, doi: 10.1016/S0140-6736(12)62001-7) did a meta-analysis of every study published through 2010 that compared folic acid supplementation to a placebo, lasted at least 1 year, included at least 500 people and recorded cancer incidence – some 13 studies with over 50,000 participants.
The results were clear cut. As for folic acid and cancer, supplementation did not increase the overall cancer risk, and when the incidence of individual cancers was analyzed, folic acid supplementation did not increase the risk of developing colon cancer, prostate cancer, lung cancer, breast cancer or any other site-specific cancer.
To put this in perspective the average dose of folic acid used in these clinical studies was 2 mg/day, which is 5 times the RDA and 5 times the dose in most supplements. And one of the clinical trials used 40 mg/day, which is 100 times the dose in most supplements.
The Bottom Line
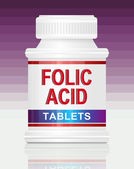
Forget the warnings and the hype. You can be confident that folic acid does not increase the risk of colorectal cancer, prostate cancer, or any other kind of cancer.
- The American Cancer Society recently performed a very large clinical study looking at the effect of folic acid intake from supplements and folate intake from foods on colon cancer risk. That study found that high intakes of neither folic acid nor natural folates were associated with any increased risk of colorectal cancer. And, they found high intake of total folates was associated with a significant decreased risk of colorectal cancer.
- The authors of that study concluded: “The findings of this study add to the epidemiological evidence that high folate intake reduces colorectal cancer risk.” “More importantly, no increased risk of colorectal cancer was found, suggesting that the high levels of this vitamin consumed by significant numbers of Americans should not lead to higher incidence rates of this cancer in the population.”
- A second meta-analysis of every clinical study looking at folic acid intake and cancer risk through 2010. The results of that study were clear cut. Folic acid supplementation did not increase the overall cancer risk, and when the incidence of individual cancers was analyzed, folic acid supplementation did not increase the risk of developing colon cancer, prostate cancer, lung cancer, breast cancer or any other site-specific cancer
Like any good scientist I am aware that future studies could change our understanding, but for now I am confident in saying that there is no credible evidence that folic acid supplementation increases your risk of any kind of cancer. If the science changes, I will be the first to let you know.
But it will be really interesting to see how long it takes all those web sites, blogs and so-called “experts” to acknowledge that the science has changed and they should stop issuing false warnings about folic acid supplementation.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.