Tips For Choosing A Diet That Works
Author: Dr. Stephen Chaney
 Diet season starts in just a few days! Like millions of Americans you will probably be setting a goal to lose weight. But which diet should you choose? Vegan, Paleo, Keto, 360, Intermittent Fasting, low-carb, low fat – the list is endless.
Diet season starts in just a few days! Like millions of Americans you will probably be setting a goal to lose weight. But which diet should you choose? Vegan, Paleo, Keto, 360, Intermittent Fasting, low-carb, low fat – the list is endless.
And then there are the commercial diets: Meal replacements, low calorie processed foods, prepared meals delivered to your door – just to name a few of the categories.
You can choose to count calories, focus on portion sizes, or keep a food journal.
And, if you really want to live dangerously, you can try the latest diet pills that claim to curb your appetite and rev up your metabolism.
The advertisements for all these diets sound so convincing. They give you scientific-sounding mumbo-jumbo to explain why they work. Then they talk about clinical studies they say prove their diet works.
If you are like most Americans, you have already tried several of these diets. They worked for a while, but the pounds came back – and brought their friends with them.
But, as the saying goes, “Hope springs eternal in the human breast. Surely some diet you haven’t tried yet will work for you.
There is such a diet. But it will require a change of mindset. It will also require effort. There is no magic wand that will chase the extra pounds away forever.
If you are searching for the perfect diet to start the new year, let me be your guide. Here are:
- 4 tips on what to avoid and…
- 6 tips on what to look for…
…when you are choosing the perfect diet.
Tips For Choosing A Diet That Works
Things To Avoid:
Endorsements by your favorite athlete or public person are paid for. They don’t necessarily represent their opinion. Nor do they assure you that they follow that diet or use that diet supplement.
Endorsements by Dr. Strangelove and his buddies can be equally misleading. They usually tell you that the medical establishment has been lying to you, and they have discovered the “secret” to permanent weight loss and the “Fountain of Youth”.
Recommendations of the medical and scientific communities usually represent a consensus statement by the top experts in their field. I would choose their advice over Dr. Strangelove’s opinion any day.
2) Testimonials
Most of the testimonials you see on TV or in print are either paid for or are fake
Testimonials by your friends can be equally misleading. We are all different. What works for your friend or your trainer may not work for you.
For example, some of us do better on low-carb diets, and others do better on low fat diets.
[Note: Some DNA testing companies claim they can sequence your DNA and tell you which diet is best. However, as I reported in a recent article in “Health Tips From The Professor”, independent studies show that DNA testing is of no use in predicting whether low-carb or low-fat diets are better for you.]
3) Diets Based on “Magic” Or “Forbidden” Foods or Food Groups.
I have often said we have 5 food groups for a reason. Each food group provides a unique blend of nutrients and phytonutrients. And each plant food group provides a unique blend of fibers that support the growth of different types of friendly gut bacteria.
The bottom line is that each of us does better with some foods than others, but there are no “magic” or “forbidden” foods that apply to everyone.
4) “Magic” Diets.
 I have written perhaps the first diet book, “Slaying The Food Myths”, that doesn’t feature a “magic” diet that is going to make the pounds melt away and allow you to live to 100. Instead I recommend a variety of healthy diets and suggest you choose the one that fits you best.
I have written perhaps the first diet book, “Slaying The Food Myths”, that doesn’t feature a “magic” diet that is going to make the pounds melt away and allow you to live to 100. Instead I recommend a variety of healthy diets and suggest you choose the one that fits you best.
However, I understand the allure of “magic” diets. Dr. Strangelove claims the diet will be effortless. He gives you some scientific-sounding mumbo-jumbo to convince you the diet is scientifically sound. Then he cites some clinical studies showing the diet will cause you to lose weight and will improve your health parameters (things like cholesterol, triglycerides, blood sugar, and blood pressure). It sounds so convincing.
Before you fall for Dr. Strangelove’s latest “magic” diet, let me share two things that may blow your mind:
-
- The studies are all short-term (usually 3 months or less).
-
- When you rely on short-term studies, the very low-fat Vegan diet and very low-carb Keto diet give you virtually identical weight loss and improvement in health parameters!
Those two diets are as different as any two diets could be. That means we can forget all the scientific-sounding mumbo-jumbo as to why each of those diets work. Instead, we should ask what these two diets have in common.
The answer is simple:
#1: The clinical studies are comparing “magic” diets to the typical American diet. Anything is better than the typical American diet! It is high in sugar, refined carbohydrates, saturated fat, and highly processed foods. No wonder the “magic” diets look so good.
#2: The diets are whole food diets. Anytime you eliminate sodas, fast foods, and highly processed foods, you will lose weight.
#3: The diets eliminate one or more food groups. Whenever you eliminate some of your favorite foods from your diet, you tend to lose weight without thinking about it. I call this the cream cheese and bagels phenomenon.
- If you are following a low-fat diet, it sounds great to say you can eat all the bagels you want. But without cream cheese to go with the bagels, you tend to eat fewer bagels.
- If you are following a low-carb diet, it sounds great to say you can eat as much cream cheese as you want, but without bagels to go with your cream cheese, you tend to eat less cream cheese.
#4: Because they eliminate many of your favorite foods, “magic” diets make you focus on what you eat. Whenever you focus on what you eat, you tend to lose weight. That is why food journals and calorie counters are effective.
#5: Finally, whenever you lose weight, your health parameters (cholesterol, triglycerides, blood sugar, and blood pressure) improve.
Things To Look For In Choosing A Healthy Diet For The New Year
 1) Choose whole food diets. Avoid sodas, fast foods, and highly processed foods.
1) Choose whole food diets. Avoid sodas, fast foods, and highly processed foods.
2) Choose primarily plant-based diets. These can range from Vegan through semi-vegetarian, Mediterranean, DASH, and Nordic. All are healthy diets. I have discussed the evidence for this recommendation in my book “Slaying The Food Myths”. Here is a brief summary.
When we look at long term (10-20 year) studies:
-
- Vegetarians weigh less and are healthier than people consuming the typical American diet.
-
- People consuming semi-vegetarian, Mediterranean, and DASH diets are healthier than people consuming the typical American diet.
If you look at low-carb diets:
-
- People consuming plant-based low-carb diets weigh less and are healthier than people consuming the typical American diet.
-
- People consuming meat-based low-carb diets are just as fat and unhealthy as people consuming the typical American diet.
-
- The Atkins diet low-carb diet has been around for more than 50 years, and there is no evidence it is healthy long-term
3) Choose diets that include a variety of foods from all 5 food groups. I have discussed the rationale for that recommendation above.
4) Choose diets that consider meat as a garnish, not a main course.
5) Choose diets that feature healthy carbs and healthy fats rather than low-carb or low-fat diets.
6) Think lifestyle, not diet. If you choose a restrictive diet so you can achieve quick weight loss, you will probably be just as fat and unhealthy next December 31st as you are this year. Instead, choose diets that teach healthy eating and lifestyle changes that you can make a permanent part of your life.
Tips For Keeping The Weight Off
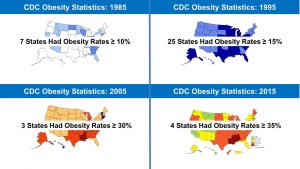
 You know the brutal truth. Around 95% of dieters regain everything they lost and then some within a few years. You have probably gone through one or more cycles of weight loss and regain yourself – something called “yo-yo dieting”. You may even be asking yourself if it is worth bothering to try to lose weight this year.
You know the brutal truth. Around 95% of dieters regain everything they lost and then some within a few years. You have probably gone through one or more cycles of weight loss and regain yourself – something called “yo-yo dieting”. You may even be asking yourself if it is worth bothering to try to lose weight this year.
Rather focusing on the negative statistics of weight loss, let’s look at the good news. There are people who lose the weight and keep it off. What do they do?
There is an organization called the National Weight Control Registry that has enrolled more than 10,000 people who have lost weight and kept it off. The people in this group lost weight on almost every diet imaginable. However, here is the important statistic: On average people in this group have lost 66 pounds and kept it off for 5 years.
The National Weight Control Registry has kept track of what they have done to keep the weight off. Here is what they do that you may not be doing:
- They consume a reduced calorie, low fat diet.
- They get lots of exercise (around 1 hour/day).
- They have internalized their eating patterns. In short, this is no longer a diet. It has become a permanent part of their lifestyle. This is the way they eat without even thinking about it.
- They monitor their weight regularly. When they gain a few pounds, they modify their diet until they are back at their target weight.
- They eat breakfast on a regular basis.
- They watch less than 10 hours of TV/week.
- They are consistent (no planned cheat days).
Which Weight Loss Diet Is Best For You?
I have covered a lot of ground in this article. Let me summarize it for you.
If you are thinking about popular diets:
- Primarily plant-based diets ranging from Vegan to Mediterranean and Dash are associated with a healthier weight and better health long term.
- If want to lose weight quickly, you may want to start with the more restrictive plant-based diets, like Vegan, Ornish, Pritikin or semi-vegetarian.
- If you do better with a low-carb diet, my recommendation is the low-carb version of the Mediterranean diet.
- If your primary goal is rapid weight loss, you could also start with one of the healthier of the restrictive low-carb diets, like the Paleo or the 360 diet. I do not recommend the Keto diet.
- No matter what diet you start with, plan to transition to the primarily plant-based diet that best fits your lifestyle and food preferences. This is the diet you will want to stick with to maintain your weight loss and achieve better health long term.
- Plan on permanent lifestyle change rather than a short-term diet. Otherwise, you are just wasting your time.
- Eat whole foods. Big Food keeps up with America’s favorite diets and is only too happy to sell you highly processed foods that match your favorite diet. Avoid those like the plague.
If you are thinking about commercial diets featuring meal replacement products:
- Look for meal replacement products that:
-
- Do not contain artificial sweeteners, flavors, or preservatives.
-
- Use non-GMO protein. A non-GMO certification for the other ingredients is not necessary. For a more detailed explanation of when non-GMO certification is important and when it is unnecessary, see my article in “Health Tips From the Professor”.
-
- Have stringent quality controls in place to assure purity. “Organic” and/or “non-GMO” on the label do not assure purity.
- Look for programs that can provide clinical studies showing their diet plan is effective for weight loss and for keeping the weight off. Many programs have short-term clinical studies showing they are effective for weight loss, but very few have longer-term studies showing the weight stays off.
- Finally, look for programs that teach permanent lifestyle change. This should include guidance on exercise and healthy eating.
I do not recommend most commercial diets that feature prepared low-calorie foods “shipped right to your door” as a major part of their program. The foods are highly processed. Plus, they include all your favorite unhealthy foods as part of the program. Even if they include lifestyle change as part of their program, they are undermining their message with the foods they are providing you.
I would be remiss if I didn’t mention that Weight Watchers is highly recommended by most experts in the field. Weight Watchers emphasizes journaling and counting calories, which is a plus because it makes you focus on what you are eating. They also have a good lifestyle program and support that can help you transition to permanent lifestyle change if you are willing to put in the effort. However, I don’t recommend their prepared low-calorie foods. They are no better than foods provided by the other commercial diet programs.
The Bottom Line
Weight loss season is upon us. If you plan to lose weight and/or adopt a healthier diet in the coming year, you are probably trying to decide which diet to try this year. In this issue of “Health Tips From The Professor” I give you:
- 4 tips on what to avoid when selecting your diet.
- 6 tips on how to choose your perfect diet.
- 7 tips on how to keep the weight off.
Then I put all this information together to help you choose the best diet, the best meal replacement product, and/or the best commercial diet program.
For more details read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.