Are Whole Grains Healthy?
Author: Dr. Stephen Chaney
 Low carb enthusiasts will tell you that carbohydrates are the villain. They tell you that cutting carbohydrates out of your diet will reduce your risk of obesity, diabetes, heart disease, and cancer.
Low carb enthusiasts will tell you that carbohydrates are the villain. They tell you that cutting carbohydrates out of your diet will reduce your risk of obesity, diabetes, heart disease, and cancer.
If they limited their list of villainous foods to highly processed foods with white flour and/or added sugars, many nutrition experts would agree with them. There is widespread agreement in the nutrition community that we eat far too much of these foods.
However, I don’t have to tell you that many low carb diets also eliminate whole grains, fruits, and beans from their diets based solely on the carbohydrate content of these foods. Is this good advice? Is there any data to back up this claim?
The short answer is no. Last week I shared a study showing that fruits reduced your risk of developing type 2 diabetes.
This week I will review a study looking at the effect of whole grain consumption on the risk of developing type 2 diabetes.
How Was This Study Done?
 This study combined data from women in the Nurses’ Health Study (1984-2014) and the Nurses’ Health Study II (1991-2017), and men in the Health Professionals Follow-Up Study (1986-2016). There were 158,259 women and 36,525 men in these three studies.
This study combined data from women in the Nurses’ Health Study (1984-2014) and the Nurses’ Health Study II (1991-2017), and men in the Health Professionals Follow-Up Study (1986-2016). There were 158,259 women and 36,525 men in these three studies.
None of the participants had type 2 diabetes, cardiovascular disease, or cancer at the time they entered the studies.
At the beginning of each study and every 4 years later the participants were asked to fill out a food frequency questionnaire to collect information about their usual diet over the past year. Validation studies showed that the diets of the participants changed little over the interval of the studies. [Note: This is a strength of these studies. Many clinical studies only collect dietary data at the beginning of the study, so there is no way of knowing whether the participant’s diets changed over time.]
The participants in these studies were followed for an average of 24 years. They were sent follow-up questionnaires every two years to collect information on diseases they had been diagnosed with over the past two years. Participants who reported type 2 diabetes were sent a supplementary questionnaire to confirm the diagnosis.
This study measured the effect of whole grain consumption, and frequently consumed whole grain foods, on the long term (24 year) risk of developing type 2 diabetes.
The data were adjusted for multiple possible confounding variables (other factors that might affect the risk of developing type 2 diabetes) including age, ethnicity, smoking status, alcohol intake, multivitamin use, healthy eating index (a measure of how healthy the overall diet was), caloric intake, obesity, family history of diabetes, and use of oral contraceptives or postmenopausal hormones.
In addition, a stratified analysis was performed to assess the extent to which obesity, physical activity, smoking status, and family history of diabetes influenced the outcome.
In short, this was a very rigorous and well-controlled study.
Do Whole Grains Keep Diabetes Away?
 Total whole grain consumption was divided into five groups ranging from 2 servings per day to < 0.1 serving per day. When participants with the highest whole grain intake were compared to those with the lowest whole grain intake:
Total whole grain consumption was divided into five groups ranging from 2 servings per day to < 0.1 serving per day. When participants with the highest whole grain intake were compared to those with the lowest whole grain intake:
- Whole grain consumption was associated with a 29% lower risk of developing type 2 diabetes.
-
- The association between whole grain consumption and reduced risk of developing type 2 diabetes was stronger for lean individuals (45% reduction in risk) than for overweight (34% reduction in risk) or obese individuals (23% reduction in risk).
-
- The association between whole grain consumption and reduced risk of developing type 2 diabetes was not affected by physical activity, smoking status, or family history of diabetes.
When they looked at the entire range of whole grain intake among participants in the study:
- The risk reduction for developing type 2 diabetes was nonlinear.
-
- The greatest portion of risk reduction (30% decreased risk) occurred between 0 and 2 servings/day.
-
- However, the reduction in risk continued to decrease at a slower rate up to 4.5 servings/day (38% decreased risk), the highest intake recorded for participants in this study.
When they looked at the most frequently consumed whole grain foods and compared the risk of developing type 2 diabetes for participants consuming one or more servings per day compared with less than 1 serving per month:
- People consuming whole grain cold breakfast cereals were 19% less likely to develop type 2 diabetes.

- People consuming whole grain breads were 21% less likely to develop type 2 diabetes.
- People consuming popcorn were 8% more likely to develop type 2 diabetes.
Once again, the risk reduction was nonlinear.
- For whole grain cold breakfast cereals risk reduction plateaued at around 0.5 servings per day.
- For whole grain breads the greatest portion of risk reduction occurred at around 0.5 servings per day (17% decreased risk), but the reduction in risk continued to decrease at a slower rate up to 4 servings/day (28% decreased risk).
- For popcorn, the risk reduction curve was non-linear. There was a slight, non-significant, decrease in risk at about 0.2 servings per day, followed by a steady increase in risk up to 1.75 servings per day (24% increased risk).
When they looked at less frequently consumed whole grain foods and compared the risk of developing type 2 diabetes for participants consuming two or more servings per week compared with less than 1 serving per month:
- People consuming oatmeal were 21% less likely to develop type 2 diabetes.
- People consuming brown rice were 12% less likely to develop type 2 diabetes.
- People consuming added bran were 15% less likely to develop type 2 diabetes.
There were not enough people consuming these whole grains for the investigators to determine how many servings were optimal.
The authors concluded, “Higher consumption of total whole grains and several commonly eaten whole grain foods, including whole grain breakfast cereal, oatmeal, whole grain bread, brown rice, and added bran, was significantly associated with a lower risk of type 2 diabetes. These findings provide further support for the current recommendations of increasing whole grain consumption as part of a healthy diet for the prevention of type 2 diabetes.”
Are Whole Grains Healthy?
 This is a very impressive study. As described above, it is a large (194,784 participants), long lasting (24 years), and well-designed study. With this data in mind, we can answer several important questions.
This is a very impressive study. As described above, it is a large (194,784 participants), long lasting (24 years), and well-designed study. With this data in mind, we can answer several important questions.
Are Whole Grains Healthy?
This study explodes the myth that you should avoid whole grains if you want to prevent diabetes. Instead, the study shows that whole grain consumption decreases your risk of developing type-2 diabetes.
I recently reviewed another large, well-designed study showing that whole grain consumption reduces your risk of dying from heart disease, cancer, and all causes combined.
So, clearly whole grains are good for you. They should be an important part of your diet.
Which Whole Grains Are Healthy?
According to this study, whole grain breakfast cereals, whole grain breads, oatmeal, brown rice, and bran are all healthy. All of them significantly reduce your risk of developing type 2 diabetes. Other whole grains are likely to be healthy too, but Americans consume so little of them, they could not be analyzed in this study.
However, there are some caveats:
- You have to read labels carefully. Unless it says “100% whole grain”, it probably contains more refined grains than whole grains.
-
- Yes, food manufacturers are intentionally deceptive. Who knew?
- You have to look at the food, not just “whole grain” on the label.
-
- It is hard to imagine, but Dr. Kellogg originally created breakfast cereals as health food. However, today many “whole grain” cereals are loaded with sugar and artificial ingredients. They are highly processed foods that are anything but healthy.
-
- The case of popcorn is a perfect example. Popcorn is loaded with fiber. It should reduce your risk of diabetes. However, in this study it increased the risk of diabetes. That’s because 70% of the popcorn that Americans consume is purchased either pre-popped or ready to pop. It contains unhealthy ingredients like salt, butter, sugar, trans fats, and artificial flavors. It is a highly processed food. Air popped popcorn without the added ingredients is probably very healthy.
Why Are Whole Grains Healthy?
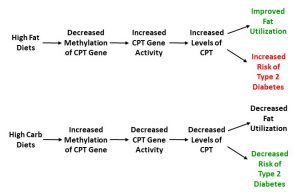
Dr. Strangelove and his buddies have told you to avoid all grains because they contain carbohydrates that are converted to sugar. That is good advice for refined grains. Not only are they rapidly converted to sugar. But they are also found in highly processed foods along with sugar, fat, and a witch’s brew of chemicals.
However, whole grains are different. Yes, whole grains are carbohydrate-rich foods, and the carbohydrate is converted to sugar during digestion. But:
- They also contain fiber, which slows the digestion of the carbohydrate and delays the absorption of the sugar released during digestion.
- The carbohydrate is trapped in a cellular matrix, which must be digested before the carbohydrate can be released.
In addition:
- Whole grains contain nutrients and phytonutrients not found in refined grains.
- The fiber in whole grains supports the growth of friendly bacteria in the gut.
How Many Whole Grain Foods Should I Be Eating?
This study found that you get the biggest “bang for your buck” when you go from 0 to around 2 servings per day of whole foods.
- If you aren’t fond of whole grain foods, that is good news. It is also in line with USDA recommendation that half the grains we eat should be whole grains. You don’t need to eat whole grains with every meal.
- If you are a purist, you can reduce your diabetes risk even more by increasing your whole grain intake up to at least 4.5 servings per day, the highest intake measured in this study.
Are Low Carb Diets Healthy?
Low carb diets may be effective for short term weight loss, but there is no evidence that they are healthy long term. And, because they cut out one or more food groups many experts feel they are likely to be unhealthy long term.
My advice is to forget “low carb” and focus on “healthy carb” instead.
- Eliminate refined carbs and the highly processed foods they are found in.
- Include fruits, whole grains, and beans as part of your diet. They are high carbohydrate foods, but, as this and other studies have shown, the carbohydrates in those foods are healthy carbs.
The Bottom Line
Low carb enthusiasts tell you to eliminate whole grains from your diet if you want to reduce your risk of developing diabetes. Is this true? Is it good advice?
A recent study put this advice to the test. It was a large (194,784 participants), long lasting (24 years), and well-designed study. Here is what the study found.
When participants with the highest whole grain intake were compared to those with the lowest whole grain intake:
- Whole grain consumption was associated with a 29% lower risk of developing type 2 diabetes.
When they looked at the entire range of whole grain intake among participants in the study:
- The risk reduction for developing type 2 diabetes was nonlinear.
- The greatest portion of risk reduction (30% decreased risk) occurred between 0 and 2 servings/day.
- But the reduction in risk continued to decrease at a slower rate up to 4.5 servings/day (38% decreased risk), the highest intake recorded for participants in this study.
When they looked at individual foods, whole grain breakfast cereals, whole grain bread, oatmeal, brown rice, and added bran all reduced diabetes risk.
The authors concluded, “Higher consumption of total whole grains and several commonly eaten whole grain foods, including whole grain breakfast cereal, oatmeal, whole grain bread, brown rice, and added bran, was significantly associated with a lower risk of type 2 diabetes. These findings provide further support for the current recommendations of increasing whole grain consumption as part of a healthy diet for the prevention of type 2 diabetes.”
For more details about this study and what it means for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.