Everything You Wanted To Know About Red Meat
Author: Dr. Stephen Chaney
 Nutrition is a bit like politics and religion. Everyone has an opinion, and there is not much grace for those with different opinions.
Nutrition is a bit like politics and religion. Everyone has an opinion, and there is not much grace for those with different opinions.
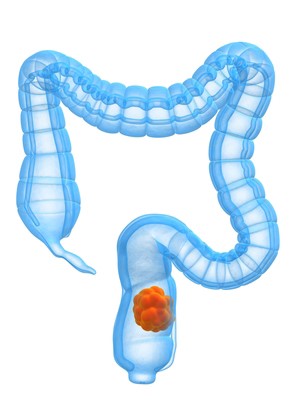
And everything is black or white. There is no middle ground. Red meat is a perfect example. Cardiologists tell us the saturated fat and cholesterol in red meat increases our risk of heart disease. Oncologists tell us red meat increases our risk of colon, breast, prostate, and pancreatic cancer.
The association with red meat consumption and colon cancer is so strong that the World Health Organization has classified red meat as a probable carcinogen.
- Vegans and vegetarians tell you to avoid red meat at all costs and substitute plant proteins in its place.
- Keto and carnivore diet enthusiasts tell you that red meat is healthy if you avoid any plant foods containing carbohydrates (which is most plant foods).
Who is right? Is red meat good for you or bad for you? As usual, the answer is somewhere in the middle. We also need to stop looking at individual foods and start looking at the overall diet. We need to ask how our overall diet alters the effect of red meat on our health.
But first, let’s explore:
- Why red meat is good for us.
- Why red meat is bad for us.
- How diet can help us minimize the bad and maximize the good.
I call this section, “Everything You Wanted To Know About Red Meat”.
Everything You Wanted To Know About Red Meat
- Red meat is an excellent source of protein, iron, and vitamin B12. Plus, the iron in red meat is primarily found in the heme molecule and heme iron is absorbed much more efficiently than other forms of iron.
- Red meat contains creatine, which powers our muscles. You can think of creatine molecules as little power packs that are charged when we eat and release a burst of energy whenever we begin to exercise.
- Red meat contains carnitine, which helps our muscles use fat as an energy source. This is particularly important for heart muscle.
- But both creatine and carnitine also have a dark side, which I will discuss below.
When we think about heart disease:
- The traditional view is that saturated fat and cholesterol are the problem, and we can reduce our risk of heart disease simply by choosing leaner cuts of meat.
- Other experts feel the link between red meat and heart disease is more complicated. For example, some recent studies have suggested that the carnitine in red meat can be converted by gut bacteria to TMAO, and TMAO increases our risk of heart disease. I have discussed this in a previous issue of “Health Tips From the Professor”.
- When fat and juices from the meat drip onto an open flame, carcinogenic polyaromatic hydrocarbons are formed that stick to the surface of the This can be reduced, but not eliminated, by lower fat meat choices.
- When red meat is cooked at high temperatures, amino acids in the meat combine with creatine, which is found in all red meats, to form carcinogenic heterocyclic amines. This can be reduced, but not eliminated, by cooking the meat at lower temperatures.
- The nitrates and nitrites used as preservatives in many processed meats react with amino acids from the meat to form carcinogenic N-nitrosamines in our intestines.
- Heme iron, which is found in all red meats, also combines with amino acids in the meat to form carcinogenic N-nitroso compounds in our intestines. This mechanism is inherent in all red meats and cannot be eliminated by choosing lower fat cuts or cooking at lower temperatures.
Finally, diets high in red meat increase several markers of inflammation, and inflammation increases the risk of both heart disease and cancer.
How Diet Can Help Us Minimize The Bad And Maximize The Good.
 I’m going to start this section with a provocative statement: “Plant foods are the antidote to all the bad effects of red meat.” Let me explain.
I’m going to start this section with a provocative statement: “Plant foods are the antidote to all the bad effects of red meat.” Let me explain.
Plant foods are an excellent source of:
- Antioxidants
- Polyphenols and other phytonutrients
- Fiber
- Plus, the fiber and phytonutrients found in plant foods support the growth of beneficial gut bacteria.
Here is where it gets very complex:
- Beneficial gut bacteria convert some of the foods we eat into compounds that are absorbed into the bloodstream and improve blood sugar control, reduce cholesterol synthesis, and reduce inflammation.
- Polyphenols support the growth of certain gut bacteria, and those gut bacteria can convert these polyphenols into compounds that can be absorbed from the intestine. This necessary for many polyphenols to exert their beneficial effects in the body.
- And, as you might expect, the gut bacteria of meat eaters and vegetarians is very different.
With this in mind, let’s come back to the concept of plant foods being the antidote for red meat.
- You may remember that I said above that the carnitine in red meat can be converted by gut bacteria into TMAO which increases the risk of heart disease. The operative wording here is “can be”. It turns out this only happens with the gut bacteria of habitual meat eaters. Here is the study that showed that:
-
- When habitual meat eaters were fed an 8-ounce sirloin steak, both carnitine and TMAO increased in their blood and urine.
-
- When vegans were fed the same 8-ounce steak, only carnitine increased. No TMAO was detected.
-
- When the meat eaters were treated with an antibiotic that wiped out their gut bacteria prior to eating the steak, no TMAO was detected. This showed it was the gut bacteria in the meat eaters that were responsible for converting carnitine to TMAO.
- Fiber from whole grains, fruits, and vegetables binds to cholesterol and flushes it out of the intestine, preventing its absorption into the bloodstream.
- Plant-based diets are anti-inflammatory.
- The fiber found in fruits, vegetables and whole grains binds to polyaromatic hydrocarbons and heterocyclic amines and flushes them out through the intestines.
- Polyaromatic hydrocarbons require activation by the liver before they become carcinogenic. Indoles and isothiocyanates found in broccoli, cabbage, and other cruciferous vegetables inhibit the enzymes that catalyze this activation.
- Antioxidants found in fruits, vegetables and whole grains reduce the formation of N-nitroso compounds in the intestines.
- A largely plant-based diet appears to favor a population of intestinal bacteria that is less likely to convert compounds in meat into cancer-causing chemicals. [Note: This is a new area of research, so the data supporting this mechanism of cancer prevention are less definitive than for the other three mechanisms.]
These observations are based studies designed to identify the mechanisms by which plant-based diets negate the bad effects of red meat. For example, let me share a recent study (T Onali et al, Journal of Nutritional Biochemistry, 141, 109906, 2025) asking whether berries could negate the bad effects of adding red meat (pork) to a typical Finnish diet.
How Was This Study Done?
 This study was conducted by a group of scientists at the University of Helsinki. They recruited 43 adults aged 20-68 and divided them into two groups. Each group was told to continue with their regular diet, except that consumption of any red meat or berries other than the foods they were provided with was prohibited.
This study was conducted by a group of scientists at the University of Helsinki. They recruited 43 adults aged 20-68 and divided them into two groups. Each group was told to continue with their regular diet, except that consumption of any red meat or berries other than the foods they were provided with was prohibited.
- Each group was given an extra 5 ounces of pork (minced pork, pulled pork, pork strips from fillet, cold cuts, sausages, and bacon) to eat each day.
- One group was also given 1 cup of berries (bilberries, strawberries, cloudberries, raspberries, lingonberries, and blackcurrant) to eat each day.
-
- Note: These are the foods most familiar to people from Finland in each category.
-
- They were provided with these foods on a weekly basis.
- This intervention portion of the study lasted four weeks.
Dietary intake was assessed in each group using 3-day food records (two weekdays and one weekend day) at the beginning and the end of the study.
Participants in the study collected stool samples on two consecutive days at the beginning and end of the study. These stool samples were analyzed in the following ways:
- Bacterial DNA was extracted from the stool samples and used to determine which gut bacteria were present in the stools.
- The stool samples were homogenized and filtered to:
-
- Determine the polyphenols and polyphenol metabolites present in the stool samples.
-
- Determine whether low molecular weight compounds present in the stool samples were able to inhibit the growth of human colon cancer cells in cell culture.
What Did The Study Show?
 The dietary analysis found that total calories, protein, carbohydrate, fat, and saturated fat did not change significantly in either group. This indicates that the study participants likely substituted the pork they were given for other high-fat meats they were eating before the study.
The dietary analysis found that total calories, protein, carbohydrate, fat, and saturated fat did not change significantly in either group. This indicates that the study participants likely substituted the pork they were given for other high-fat meats they were eating before the study.
However, in the group that was also given berries fiber, vitamin C, vitamin E, manganese, and several polyphenols increased significantly. This suggests that study participants likely substituted the berries for less healthy foods they were eating before the study.
The study found that:
- In the red meat-only group the relative abundance of beneficial Roseburia and Fecalibacterium gut bacteria was decreased. This did not occur in the red meat + berries group.
- In the red meat + berries group the concentration of several beneficial polyphenols and polyphenol metabolites was increased.
- In the red meat + berries group, the filtrate obtained from stool samples inhibited the growth of several human colon cancer cell lines in cell culture experiments. These experiments did not identify which berry polyphenols were responsible for inhibiting the growth of cancer cells. It also did not determine whether the polyphenols came directly from the berries or were created when gut bacteria modified the polyphenol(s).
But these experiments did show that something in the intestines of people consuming a high berry diet inhibited colon cancer cell growth.
The author’s concluded, “Berry supplementation to a diet high in red and processed meat led to berry-derived polyphenolic metabolites in the feces, beneficially modified gut microbiota, inhibited the viability of colon cancer cells, collectively suggesting potential in cancer prevention.
The difference seen in gut metabolism was probably induced by the higher intakes of dietary fiber, vitamin C and E, manganese, and polyphenols by the berry diet.”
Can Red Meat Be Good For You?
 This study is one piece of the puzzle to help us understand the effect of diet on the benefits and risks of red meat consumption. Here is what I mean by that.
This study is one piece of the puzzle to help us understand the effect of diet on the benefits and risks of red meat consumption. Here is what I mean by that.
We can think of scientific investigations in terms of solving a large puzzle with lots of little pieces. If you are a puzzle enthusiast, you know the best way to solve a complicated puzzle is to put the edge pieces together first and then fill in the rest of the puzzle.
In this context, the studies showing that small amounts of red meat are not harmful in the context of healthy, primarily plant-based diets like the DASH and Mediterranean diets are the edge of the puzzle. Smaller studies that define the mechanisms of this effect and provide proof these mechanisms are accurate are the interior pieces that fill out the puzzle. This study is one of those interior pieces.
So, what does that mean for you? It means that diet context is important.
Most of the studies showing the bad effects of red meat have been done in the context of the typical American diet. That might consist of an 8 or 12-ounce steak with fries and either a soft drink or iced tea. Fruits and vegetables, if present at all, are minimal. Dessert usually consists of some sugary treats.
In this context, red meat is bad for you.
In contrast, consider the place red meat occupies in a primarily plant-based diet. Red meat becomes a condiment rather than the main course. Think of 2-3 ounces of red meat as part of a green salad or stir fry with a variety of greens and other vegetables. You might have beans, whole grains, or another vegetable to round out your plate. Dessert would be whatever fruit is in season. And your beverage might be water, milk, or herbal tea.
In this context, the bad effects of red meat disappear. In short, there are no bad foods, only bad diets.
I started this blog with the question, “Can red meat be good for you?” You may be wondering if I have answered that question.
At the beginning of this article, I listed the good things about red meat, namely that it is a good source of protein, iron, vitamin B12, carnitine, and creatine.
If you remove the bad, only the good remain. So, the answer is, “Yes. In the right diet context red meat can be good for you”.
The Bottom Line
You have heard that red meat is bad for you. It increases your risk of heart disease and cancer. You should avoid it at all costs.
But is that true? In the article above I:
- Describe both the benefits and risks of red meat.
- Discuss how plant foods negate many of the bad effects of red meat.
- Share a study providing proof of that concept.
- Share how you can enjoy the benefits of red meat while avoiding the bad effects of red meat consumption.
For more details read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
______________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.