Why Is Diabetes Increasing In Our Children?
Author: Dr. Stephen Chaney
 Last week I shared a study documenting the alarming increase in ultraprocessed food consumption by our children and the effect it was having on their health (https://www.chaneyhealth.com/healthtips/are-we-killing-our-children-with-kindness/). For example, childhood obesity is closely linked to ultraprocessed food consumption.
Last week I shared a study documenting the alarming increase in ultraprocessed food consumption by our children and the effect it was having on their health (https://www.chaneyhealth.com/healthtips/are-we-killing-our-children-with-kindness/). For example, childhood obesity is closely linked to ultraprocessed food consumption.
In case you don’t understand why that is, here is what I said last week: “Because ultraprocessed foods are made in a factory, not grown on a farm:
- They are high in fat, sugar, and refined carbohydrates. That means they have a high caloric density. Each bite has 2-3 times the calories found in a bite of fresh fruits and vegetables.
- Even worse, the food industry has weaponized our natural cravings for sweet, salty, and fatty foods. They feed their prototypes to a series of consumer tasting panels until they find the perfect blend of sugar, salt, and fat to create maximum craving.
- And if that weren’t enough, they add additives to create the perfect flavor and “mouth appeal”.
-
- It is no wonder that clinical studies have found a strong correlation between high intake of ultraprocessed food and obesity in both children and adults.
-
- It is also no wonder that the rate of childhood obesity has almost quadrupled in the last 40 years.”
Unfortunately, whenever you see an increase in obesity, type 2 diabetes is not far behind. Several studies have reported a dramatic increase in type 2 diabetes in our children over the last 20 years.
Because diabetics can manage their blood sugar levels with insulin and/or a variety of drugs, many people consider it as just an inconvenience. Nothing could be further from the truth. Diabetes is a deadly disease, and it is even deadlier when it appears early in life.
You probably already know that long-term complications of diabetes include heart disease and irreversible damage to nerves, kidneys, eyes, and feet. But you may not have known that childhood diabetes is more dangerous than diabetes in adults because:
- It is more challenging to manage in children.
- The complications of diabetes start to show up much earlier in life and affect quality of life at a much earlier age. For example:
-
- Cardiovascular events occur 15 years earlier in someone with diabetes.
-
- On average, a 50-year-old with diabetes will die 6 years earlier than someone without diabetes.
-
- On average, a 10-year-old with diabetes will die 19 years earlier than a child without diabetes.
The study (JM Lawrence et al, JAMA, 326: 717-727, 2021) I will discuss today is the largest and most comprehensive study of childhood diabetes to date.
How Was This Study Done?
 The data for this study were obtained from the SEARCH For Diabetes In Youth Study. This study collected data on physician-diagnosed cases of diabetes in 3.47 million children ages 19 or younger from 6 geographical areas in the US in 2001, 2009, and 2017.
The data for this study were obtained from the SEARCH For Diabetes In Youth Study. This study collected data on physician-diagnosed cases of diabetes in 3.47 million children ages 19 or younger from 6 geographical areas in the US in 2001, 2009, and 2017.
The 6 geographical areas were:
- Southern California (7 counties, including Los Angeles).
- Colorado (14 counties, including Denver).
- Ohio (8 counties, including Cincinnati)
- South Carolina (4 counties, including Columbia).
- Washington State (5 counties, including Seattle).
- Indian Health Service users in select areas of Arizona and New Mexico.
The data on diabetes diagnoses were obtained by creating active surveillance networks composed of pediatric and adult endocrinologists, other clinicians, hospitals, and health plans in the study areas.
Is Diabetes Increasing In Our Children?
 To answer this question let’s start with a historical perspective:
To answer this question let’s start with a historical perspective:
- In 1950 obesity in US children was rare and type 2 diabetes in children was practically unknown.
-
- Since then, obesity rates have skyrocketed, and type 2 diabetes has followed along behind it.
- Between 1925 and 1950 the prevalence of type 1 diabetes in US children remained constant, but it has been steadily increasing since 1950.
-
- Type 1 diabetes remains more prevalent than type 2 diabetes in our children, but the prevalence of type 2 diabetes has been increasing faster than type 1 diabetes.
Now let’s look at the results from the SEARCH For Diabetes In Youth Study:
Prevalence of Type 2 Diabetes:
- The prevalence of type 2 diabetes in US children aged 10-19 increased from 0.34/1000 youths in 2001, to 0.46/1000 youths in 2009, to 0.67/1000 youths in 2017.
-
- This is a 94% increase between 2001 and 2017. Put another way, the prevalence of type 2 diabetes in our children has almost doubled in just 16 years!
-
- The greatest increase was seen among Black (0.85/1000 youths), Hispanic (0.57/1000 youths), and American Indian (0.42/1000 youths) population groups.
- These data are consistent with 3 previous studies reporting a doubling of type 2 diabetes in children over similar time periods.
Note: Since data collection ended in 2017, this study does not take into account the increase in type 2 diabetes caused by increased body weight and reduced activity in children during the pandemic. There are no firm data on the increase in type 2 diabetes in children during the pandemic, but some hospitals have reported increases of 50% to 300% in new diagnoses of type 2 diabetes in 2020.
Prevalence of Type 1 Diabetes:
- The prevalence of type 1 diabetes in US children aged 19 and younger increased from 1.48/1000 youths in 2001, to 1.93/1000 youths in 2009, to 2.15/1000 youths in 2017.
- This is a 45% increase between 2001 and 2017.
-
- The greatest increase was seen among White (0.93/1000 youths), Black (0.89/1000 youths), and Hispanic (0.59/1000 youths) population groups.
-
- These data are consistent with a similar study of type 1 diabetes in children in Holland.
In summary:
- This study documents a dramatic increase in the prevalence of both type 1 and type 2 diabetes in US children between 2001 and 2017.
- Type 2 diabetes is still less prevalent than type 1 diabetes in US children, but it is increasing twice as fast.
Why Is Diabetes Increasing In Our Children?
 When it comes to type 2 diabetes, the experts agree:
When it comes to type 2 diabetes, the experts agree:
- The increase in type 2 diabetes in children is directly related to the obesity epidemic, which is now impacting our children. The obesity epidemic is, in turn, caused by:
-
- Increased reliance on highly processed food by our children, as I discussed last week (https://www.chaneyhealth.com/healthtips/are-we-killing-our-children-with-kindness/).
-
- Decreased exercise. Video games and social media have replaced actual games played outside.
However, when it comes the increase in type 1 diabetes, the experts are perplexed. There is no easy explanation. Let’s start with the basics:
- Type 1 diabetes is an autoimmune disease. With type 1 diabetics, their immune system starts attacking the insulin-producing beta cells in their pancreas. Consequently, they lose the ability to produce insulin.
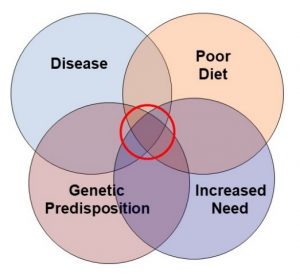
- The autoimmune response seen in type 1 diabetes is caused by a combination of genes and environment. Specifically:
-
- Certain genes predispose to type 1 diabetes. However:
-
-
- Only some people with those genes develop type 1 diabetes.
-
-
-
- Our genetics doesn’t change with time, so genetics cannot explain the increases in type 1 diabetes we are seeing.
-
- That leaves the environment. There are many hypotheses about how our children’s environment influences their risk of developing type 1 diabetes. However:
-
- Some of these hypotheses involve things that have not changed over the last 15-20 years. They cannot explain the increase in type1 diabetes we are seeing in children.
-
- Some of these hypotheses are not supported by good data. They are speculative.
With that in mind, I will list the top 5 current hypotheses and evaluate each of them.
#1: The viral infection hypothesis: Basically, this hypothesis states that type 1 diabetes can be triggered by  common viral infections such as the flu.
common viral infections such as the flu.
- This is a plausible hypothesis. Whenever our immune system is stimulated by invaders it sometimes goes rogue and triggers autoimmune responses.
- It is also supported by good data. The onset of type 1 diabetes is often associated with a viral infection in genetically susceptible children.
- However, prior to the pandemic viral infections have been constant. They haven’t changed over time. Therefore, they cannot explain an increase in type 1 diabetes between 2001 and 2017.
#2: The hygiene hypothesis: Basically, this hypothesis states that when we raise our children in a sterile environment, their immune system doesn’t develop normally. Essentially the hypothesis is saying that it’s not a bad thing if your toddler eats some dirt and moldy fruits. However:
- The data linking hygiene to food allergies is better than the data linking hygiene to autoimmune responses.
- There is no evidence that hygiene practices have changed significantly between 2001 and 2017.
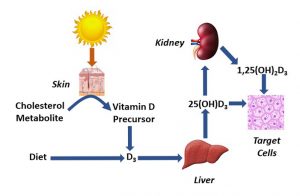
#3: The vitamin D hypothesis: Basically, this hypothesis states that vitamin D deficiency is associated with the autoimmune response that causes type 1 diabetes.
- One of the functions of vitamin D is to regulate the immune system.
- As I have reported previously, suboptimal vitamin D levels are associated with increased risk of developing type 1 diabetes.
- While we know that up to 61% of children in the US have suboptimal vitamin D levels, we don’t know whether that percentage has changed significantly in recent years.
 #4: The gut bacteria hypothesis: Basically, this hypothesis suggests that certain populations of gut bacteria increase the risk of developing type 1 diabetes. This is what we know.
#4: The gut bacteria hypothesis: Basically, this hypothesis suggests that certain populations of gut bacteria increase the risk of developing type 1 diabetes. This is what we know.
- Children who develop type 1 diabetes have a unique population of gut bacteria.
- This population of gut bacteria also triggers inflammation, and chronic inflammation can lead to autoimmune responses.
- A diet rich in highly processed foods supports growth of the same gut bacteria found in children with type 1 diabetes.
- Consumption of highly processed foods has increased significantly in the last twenty years.
#5: The obesity hypothesis: Basically, this hypothesis suggests that obesity increases the risk of developing type 1 diabetes.
- While the mechanism is not clear, childhood obesity is associated with both inflammatory and autoimmune diseases like type 1 diabetes.
- Childhood obesity has increased dramatically in the past few years.
As you may have noticed, there are weaknesses to each of these hypotheses. This is why there is no current agreement among experts as to why type 1 diabetes is increasing in our children.
My guess is that none of these hypotheses can fully explain the increase in type 1 diabetes in our children, but that several of them may contribute to it.
What Can We Do?
 Whatever the mechanism, the increase in both type 1 and type 2 diabetes in our children is troubling. Unless this trend is reversed, we may be dooming our children to short, unhealthy lives. So, what can we, as concerned parents and grandparents, do?
Whatever the mechanism, the increase in both type 1 and type 2 diabetes in our children is troubling. Unless this trend is reversed, we may be dooming our children to short, unhealthy lives. So, what can we, as concerned parents and grandparents, do?
For type 2 diabetes, the answer is clear.
1) Reverse the dominance of ultraprocessed foods in children’s diets. Encourage the consumption of whole, unprocessed or minimally processed foods, and include lots of fresh fruits and vegetables. Set a good example as well.
2) Encourage more activity. Get them outside and moving. Create family activities that involve exercise.
3) Reverse the obesity epidemic. If we succeed in reversing the dominance of ultraprocessed foods in their diet and encouraging more activity, we can reverse the obesity epidemic without putting our children on crazy diets.
For type 1 diabetes, the answer is less clear because the cause for the increase in type 1 diabetes is uncertain. However, I will point out that:
1) Increased consumption of fresh fruits and vegetables, whole grains, and legumes supports the growth of friendly gut bacteria that reduce inflammation and the risk of autoimmune diseases. For more detail on an anti-inflammatory diet, click here.
2) Reversing the obesity epidemic also reduces inflammation and the risk of autoimmune diseases.
3) Adequate vitamin D levels reduce the risk of autoimmune diseases, including type 1 diabetes. My recommendation is to get your 25-hydroxyvitamin D levels tested and supplement with vitamin D3 as needed, especially during the winter months.
The Bottom Line
Last week I shared a study documenting the alarming increase in ultraprocessed food consumption by our children and the effect it was having on their health. For example, childhood obesity is closely linked to ultraprocessed food consumption, and the rate of childhood obesity has almost quadrupled in the last 40 years.
Unfortunately, whenever you see an increase in obesity, type 2 diabetes is not far behind. This week’s study looked at the prevalence of childhood diabetes in 3.47 million children from 6 geographical areas of the United States between 2001 and 2017. This study found:
- The prevalence of type 2 diabetes in US children increased 94% between 2001 and 2017. It almost doubled.
- The prevalence of type 1 diabetes in US children increased 45% between 2001 and 2017.
These statistics are tragic because diabetes is a deadly disease.
You probably already know that long-term complications of diabetes include heart disease and irreversible damage to nerves, kidneys, eyes, and feet. But you may not have known that childhood diabetes is more dangerous than diabetes in adults because:
- It is more challenging to manage in children.
- The complications of diabetes start to show up much earlier in life and affect quality of life at a much earlier age. For example:
-
- Cardiovascular events occur 15 years earlier in someone with diabetes.
-
- On average, a 50-year-old with diabetes will die 6 years earlier than someone without diabetes.
-
- On average, a 10-year-old with diabetes will die 19 years earlier than a child without diabetes.
For more details about this study, why the prevalence of diabetes in US children is increasing, and what we can do about it, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease