Is It Three Strikes And You Are Out?
Author: Dr. Stephen Chaney
 If you are pregnant, you want the best for your unborn baby. Your doctor has recommended a prenatal supplement, but do the prenatal supplements on the market meet your needs? A few months ago, I shared two studies that concluded that most prenatal supplements on the market are woefully inadequate.
If you are pregnant, you want the best for your unborn baby. Your doctor has recommended a prenatal supplement, but do the prenatal supplements on the market meet your needs? A few months ago, I shared two studies that concluded that most prenatal supplements on the market are woefully inadequate.
In fact, the authors said, “[Our] analysis found that prenatal supplements vary widely in content, often only contain a subset of essential vitamins, and the levels were often below…recommendations.”
In other words, their study found that most prenatal vitamins on the market may not be adequate to support your needs and the needs of your child through pregnancy and breastfeeding.
Now, a third study on the topic has been published (KA Saunders et al, American Journal of Clinical Nutrition, 117: 823-829, 2023. It differs from the previous studies in that:
1) The previous two studies took a comprehensive approach, while this study focused on 6 key nutrients.
- The previous studies included all nutrients important for a healthy pregnancy including choline, iodine, and vitamin K, which have only recently been shown to be important for a healthy pregnancy.
- This study focused on 6 nutrients, vitamin A, vitamin D, folic acid, calcium, iron, and omega-3 fatty acids, which have long been recognized as essential for a healthy pregnancy.
2) The previous two studies focused on prenatal supplements, while this study focused on all supplements that might be taken by pregnant women.
3) The previous two studies asked whether supplements provided recommended amounts of all nutrients needed for a healthy pregnancy. This study took a “Goldilocks approach” and asked whether levels of these 6 essential nutrients were appropriate (“just right”). The study:
- Started by determining the intake of these 6 key nutrients by American women. The authors of the study then added the amount of each nutrient provided by the supplements in their study to the amount of that nutrient in the diet of American women and:
-
- Calculated the minimum amount of each nutrient that would be needed to assure that 90% of American women taking a particular supplement would meet the recommended intake for pregnant and lactating women.
-
- Calculated the maximum amount of each nutrient provided by supplements in their study to assure that that 90% of American women taking that supplement would not get potentially toxic amounts of that nutrient.
- In other words, for each of the 6 nutrients they calculated a supplemental dose range that was neither too low nor too high. They called this the “appropriate dose range” for each nutrient. Goldilocks would have called it “just right”.
I’m sure you are anxiously waiting to learn what their study found. But before we go there, I will describe how the study was done.
How Was The Study Done?
 For the dietary intake portion of the study, the authors used dietary intake data previously collected from the Environmental Influences on Child Health Outcomes (ECHO) study.
For the dietary intake portion of the study, the authors used dietary intake data previously collected from the Environmental Influences on Child Health Outcomes (ECHO) study.
The ECHO study is a consortium of 69 medical centers across multiple states. It is an observational study of mothers and their offspring designed to understand the effects of early life exposures on child health and development.
The current study analyzed dietary intake data for 2450 participants from 6 medical centers across 5 states in the ECHO study. The women in this study were diverse with respect to ethnicity, education, and weight.
All pregnant women in the current study completed at least one 24-hour dietary recall between 6-week gestation until delivery (24% completed one dietary recall. 76% completed two or more dietary recalls). Dietary intake was generally assessed with an expert interviewer and included all foods and beverages consumed in the previous 24 hours.
For the supplement portion of the study, the authors used the NIH Dietary Supplement Label Database because it is the most complete listing of supplements in the US. The authors selected 20,547 supplements that contained at least one of the 6 essential nutrients from this database.
To determine which of the 20,547 supplements contained appropriate levels of the 6 nutrients (vitamin A, vitamin D, folic acid, calcium, iron, and omega-3 fatty acids) selected for this study, the authors used the process described in the introduction above. Briefly:
- The authors added the amount of each nutrient provided by the supplements in their study to the amount of that nutrient in the diet of American women and:
- Calculated the minimum amount of each nutrient that would be needed to assure that 90% of American women taking a particular supplement would meet the recommended intake for pregnant and lactating women.
- Calculated the maximum amount of each nutrient provided by supplements in their study to assure that that 90% of American women taking that supplement would not get potentially toxic amounts of that nutrient.
In other words, for each of the 6 nutrients they calculated a supplemental dose range that was neither too low nor too high. They called this the “appropriate dose range” for each nutrient.
Why Are The 6 Nutrients Included In This Study Important?
 Dietary Intake Is Often Inadequate
Dietary Intake Is Often Inadequate
The diet analysis of pregnant American women in this study found:
- 42% were at risk of inadequate vitamin A intake.
- 96% were at risk of inadequate vitamin D intake.
- 45% were at risk of inadequate folic acid intake.
- 55% were at risk of inadequate calcium intake.
- 93% were at risk of inadequate iron intake.
- 67% were at risk of inadequate omega-3 intake.
The percentage of women at risk for inadequate intake of these nutrients varied with age, ethnicity, and income levels. But the overall message is clear. Most American women are not getting enough of these essential nutrients from their diet alone.
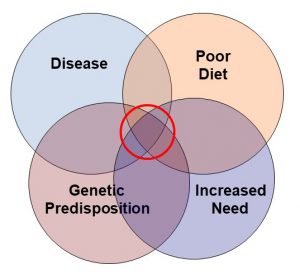
The Risk of Inadequate and Excessive Intake Of These Nutrients
These 6 nutrients were chosen in part because reviews by the Cochrane Collaboration have concluded that inadequate intake of these nutrients are associated with complications during pregnancy and delivery. They can also adversely affect the health and normal development of the baby.
This is important because the Cochrane Collaboration is considered the Gold Standard of clinical studies. You can find a more detailed description of Cochrane Collaboration studies and why they are the Gold standard here.
[Note: The Cochrane Collaboration has not yet evaluated choline, iodine, and vitamin K for pregnant women, but their inclusion in prenatal supplements is supported by multiple clinical studies.]
In addition, excess intake of all these nutrients except omega-3s can harm both the fetus and the mother. The is why the Food and Nutrition Board has set ULs (Upper Limits – the level above which toxicity can occur) for 5 of the 6 nutrients. This is important because previous studies have suggested that up to 25% of women may be getting toxic levels of one or more of these nutrients when you consider both their dietary intake and their prenatal supplement.
Summary
In other words, both too little and too much of these nutrients can harm the mom and her baby. It is critical that prenatal supplements get the dosing right.
It is for that reason that the authors of this study have set an “appropriate dose range” (high enough that 90% of women have enough of each nutrient to prevent deficiency and low enough that 90% of women do not exceed the UL for each nutrient) as the standard for evaluating the adequacy and safety of supplements for pregnant women.
Prenatal Supplements Strike Out Again
 Of the 20,547 supplements (421 labeled as prenatal supplements) available on the US market as of December 31, 2022, the investigators reported that:
Of the 20,547 supplements (421 labeled as prenatal supplements) available on the US market as of December 31, 2022, the investigators reported that:
- Only 69 (0.3%) supplements contained all 6 nutrients considered essential for a healthy pregnancy.
- Only 1 supplement contained all 6 nutrients at the appropriate doses, and it wasn’t even labeled as a prenatal supplement.
In addition:
- One supplement containing all 6 nutrients put 100% of the women in their study at risk for excessive intake of folic acid.
- Another supplement containing all 6 nutrients put 46% of the women in their study at risk of inadequate calcium intake.
The authors concluded, “Almost no US dietary supplements provide key nutrients in the doses needed for pregnant women. Affordable and convenient products that fill the gap between food-based intake and estimated requirements of pregnancy without inducing excess intake are needed to support pregnant women and their offspring.”
In short, the conclusion of this study can be summed up as, “Prenatal Supplements Strike Out Again”.
[Note: It sometime takes a while for supplement labels to be posted in the NIH Dietary Supplement Label Database. The authors acknowledged that this study may not include supplements introduced or reformulated in the last quarter of 2022.]
Is It Three Strikes And You Are Out?
 If you are pregnant or thinking of becoming pregnant, this should be a wake-up call.
If you are pregnant or thinking of becoming pregnant, this should be a wake-up call.
70% of pregnant women in this country take prenatal supplements, usually based on recommendations by their health care provider. They assume the prenatal supplements meet their needs and the needs of their unborn baby.
Yet three studies evaluating the adequacy of prenatal supplements have been published in the past few months. They took very different approaches in evaluating the supplements. But all three studies concluded that the vast majority of prenatal supplements on the market are woefully inadequate.
You may be wondering, “Is it three strikes, and you are out?” Are there no decent prenatal supplements on the market? The answer to those questions is, “No. There are good prenatal supplements on the market.”
You may be wondering how I can say that in the face of such overwhelming negative data. That’s because while all 3 studies were very good studies, they each had “blind spots”:
1) Each of the studies used very stringent criteria for identifying adequate prenatal supplements. In some cases, their criteria were stricter than the RDA recommendations and the recommendations of the American College of Obstetrics and Gynecology for pregnant and lactating women. It could be argued that their criteria were too stringent.
2) In the case of the current study, it could also be argued that evaluating only 6 nutrients is not a good criterion for evaluating the adequacy of prenatal supplements. For example, I looked up the one supplement rated as adequate in this study. It does provide appropriate doses of the 6 nutrients this study focused on. It also provides appropriate doses of vitamin K and iodine. But it does not provide choline. It is a very good supplement for women, but it is not the perfect prenatal supplement.
So, what can you do? How can you find the best prenatal supplement for you? Unfortunately, you cannot rely on advice from your friends or your health professional. You cannot rely on advertisements. That is a good place to start, but you have to do your own sleuthing.
With that in mind, I have listed 7 simple rules for selecting the best possible prenatal supplement in my article about the first two studies. Use these rules for evaluating every prenatal supplement you come across. Happy sleuthing.
The Bottom Line
A recent study evaluated all 20,547 supplements on the US market to see if they met the needs of pregnant women in this country.
- They focused on 6 nutrients (vitamin A, vitamin D, folic acid, calcium, iron, and omega-3s) known to be essential for a healthy pregnancy.
- They determined the dietary intake for all 6 nutrients in a cross section of pregnant women in the US.
- They added the amount of the 6 nutrients in each of the 20,547 supplements to the dietary intake of those nutrients by pregnant women.
- They then asked which supplements provided the “appropriate dose” of all 6 nutrients. They defined “appropriate dose” as the dose range that was.
-
- High enough to prevent deficiency of that nutrient in 90% of pregnant women taking the supplement…and…
-
- Low enough to prevent toxicity from that nutrient in 90% of pregnant women taking the supplement.
- In other words, for each of the 6 nutrients they calculated a supplemental dose range that was neither too low nor too high.
Of the 20,547 supplements (421 labeled as prenatal supplements) available on the US market:
- Only 69 (0.3%) supplements contained all 6 nutrients they considered essential for a healthy pregnancy.
- Only 1 supplement contained all 6 nutrients at the appropriate doses, and it wasn’t even labeled as a prenatal supplement.
The authors concluded, “Almost no US dietary supplements provide key nutrients in the doses needed for pregnant women. Affordable and convenient products that fill the gap between food-based intake and estimated requirements of pregnancy without inducing excess intake are needed to support pregnant women and their offspring.”
[Note: It sometime takes a while for supplement labels to be posted in the NIH Dietary Supplement Label Database. The authors acknowledged that this study may not include supplements introduced or reformulated in the last quarter of 2022 or early 2023.]
If you are pregnant or thinking of becoming pregnant, this should be a wake-up call.
70% of pregnant women in this country take prenatal supplements, usually based on recommendations by their health care provider. They assume the prenatal supplements meet their needs and the needs of their unborn baby.
Yet three studies evaluating the adequacy of prenatal supplements have been published in the past few months. And all three studies concluded that the vast majority of prenatal supplements on the market are woefully inadequate.
You may be wondering, “Is it three strikes, and you are out?” Are there no decent prenatal supplements on the market? The answer to those questions is, “No. There are good prenatal supplements on the market.”
You may be wondering how I can say that in the face of such overwhelming negative data. That’s because while all 3 studies were very good studies, they each had “blind spots”:
For more details on this study and 7 tips on finding the best prenatal supplement for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
 July is here and Florida is hot! The “Snowbirds” have gone north to the cooler weather (a goal of mine!) and life is moving in the slow lane.
July is here and Florida is hot! The “Snowbirds” have gone north to the cooler weather (a goal of mine!) and life is moving in the slow lane. Hopefully you aren’t suffering from restless leg syndrome (RLS), but maybe you know someone who is, and if so, this newsletter may be of some help.
Hopefully you aren’t suffering from restless leg syndrome (RLS), but maybe you know someone who is, and if so, this newsletter may be of some help.
 You can locate the source of your pain, and then see how to do the Julstro self-treatments that can stop the pain FAST!
You can locate the source of your pain, and then see how to do the Julstro self-treatments that can stop the pain FAST!