Treating Your Rectus Femoris Muscle Safely
Author: Julie Donnelly, LMT – The Pain Relief Expert
Editor: Dr. Steve Chaney
 I hope that 2023 was kind to you and your family. Covid seemed to come and go, with new strains popping up every time we turned around. And then there is RSV and the flu. What a year!
I hope that 2023 was kind to you and your family. Covid seemed to come and go, with new strains popping up every time we turned around. And then there is RSV and the flu. What a year!
In December the foods all seemed to be fattening – delicious for sure, but fattening. Which brings me to the topic of the month. Maybe you are trying to walk off some of the extra calories you put on last month.
Walking will help burn calories, but it can also come with aches and pains from muscles getting used repetitively.
This month I want to focus on pain that prevents you from bending your knee after several days of walking more than your body is used to. It can reduce your walks to a slow hobble at best. And that isn’t going to burn off any extra calories.
One Quadricep Muscle is the Source of Pain from the Low Back to the Knee.
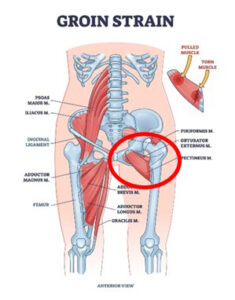
You likely already know that there are four quadriceps that form the front of your thigh. You probably also know that they are responsible for straightening your leg when you want to stand up from sitting. But there is so much more…especially for one of the quads…the rectus femoris.
Your Rectus Femoris Muscle And Knee Pain
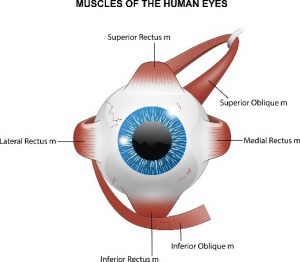
The rectus femoris is a long muscle located in the front, and a bit toward the outside of your thigh.
The rectus femoris is the only one of the four quads that originate on the tip of your pelvis (ASIS), the rest: vastus lateralis, vastus intermedius, and vastus medialis, all originate along your thigh bone (femur). These four muscles join together and attach to your kneecap (patella).
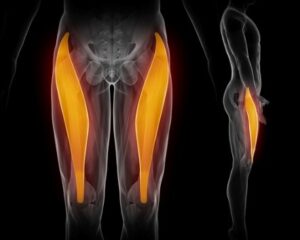 This picture shows the muscle but fails to show the tendon that starts at the top of your kneecap, goes over your kneecap (patella), and inserts into the front of your shin bone (tibia).
This picture shows the muscle but fails to show the tendon that starts at the top of your kneecap, goes over your kneecap (patella), and inserts into the front of your shin bone (tibia).
It is the patella tendon that causes knee pain and can prevent you from bending your knee when you sit down or want to walk up steps.
Think of the analogy I use so frequently. When you pull your hair, your head hurts, but you don’t need to rub your head, take pain pills, or have brain surgery. You just need to let go of your hair!
In the same way, the muscle is pulling down on the front of your hip and may cause anterior hip pain, and it’s pulling up on your patella tendon, causing your kneecap to move up so you can’t bend your knee, and putting stress on your shin bone.
Your knee and front of your hip are NOT the problem, they are the symptom!
The Function Of The Rectus Femoris Muscle:
Since the muscle originates on the tip of your pelvis,
- The rectus femoris flexes (bends) the hip along with two other muscles I’ve discussed in the past, the sartorius and iliopsoas. The four quads pull up on your lower leg at the knee, straightening your leg so you can stand up.
Injury To The Rectus Femoris Muscle:
- In acute rectus femoris muscle injuries, a person may feel a tearing sensation at their knee, with an abrupt onset of pain.
- Subacute injuries may present with gradual onset of pain at either the front of your hip or your knee. If you enjoy running, you may also have knee pain while you’re running uphill.
- You may feel that you have arthritis in your knee joint. If that is the case, it is beneficial to see a deep muscle massage therapist to eliminate tight muscles from the diagnosis. You can also do the Julstro self-treatment that is shown below to release the tension in the muscle.
- When a muscular strain injury occurs, a person may also have moderate to severe pain in the groin.
- Pain can be sudden, like kicking the ball in soccer or sprinting from a standing position. Or it may build up gradually as an overuse problem with repeated tearing and repeated stress.
- Stretching, without first releasing the tension in the muscle, can cause tearing where the muscle inserts into the tendon, or tear the tendon fibers from the bone.
- Spasms in your rectus femoris can also be caused by contractions in the muscles that impact your lower back and pelvis. If this is the case, you need to treat each of the muscles before your thigh muscles release. I demonstrate the full treatment in my books in the chapter about the Julstro Protocol.
Treating Your Rectus Femoris Muscle Safely
There are multiple ways to treat your rectus femoris muscle and I show them to you in my books: The Pain-Free Athlete and Treat Yourself to Pain-Free Living.
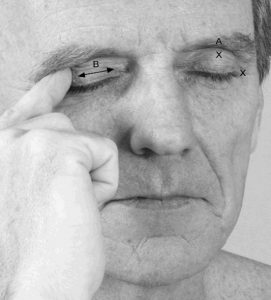
 Using a 12” length of 1” PVC pipe, place the pipe as shown in this picture. This is the perfect position to treat the rectus femoris.
Using a 12” length of 1” PVC pipe, place the pipe as shown in this picture. This is the perfect position to treat the rectus femoris.
Hold the pipe loosely in your hand or hold your four fingers straight out so you are not curling them around the pipe. This will prevent tension from forming in your forearm muscles.
Press into your thigh and slide, don’t roll, down your thigh to just above your knee.
Do this to your entire thigh, outside/front/inside so you treat all four quadriceps.
I suggest you treat both thighs, even if you are only having pain in one leg.
Wishing you well,
Julie Donnelly
www.FlexibleAthlete.com
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
About The Author
Julie Donnelly has been a licensed massage therapist since 1989, specializing in the treatment of chronic pain and sports injuries. The author of several books including Treat Yourself to Pain-Free Living, The Pain-Free Athlete, and The 15 Minute Back Pain Solution.
Julie has also developed a proven self-treatment program for the symptoms of carpal tunnel syndrome.
She has a therapy practice in Sarasota, Florida, and she travels around the USA to teach massage and physical therapists how to do the Julstro Method, and she also teaches self-treatment clinics to anyone interested in taking charge of their own health and flexibility.
She may be reached at her office: 919-886-1861, or through her website: www.FlexibleAthlete.com