Are There Any Sports Supplement Companies You Can Trust?
Author: Dr. Stephen Chaney
 “Pump up your muscles”, “Explode your muscles”, “”Blast your fat”, “Annihilate your fat”, “Ramp up your energy”: The claims leap off the page of the ads for many sports and weight loss supplements. But, are sports supplements safe?
“Pump up your muscles”, “Explode your muscles”, “”Blast your fat”, “Annihilate your fat”, “Ramp up your energy”: The claims leap off the page of the ads for many sports and weight loss supplements. But, are sports supplements safe?
The easiest way to ramp up your energy and annihilate your fat is to put amphetamines or other illegal stimulants in the supplement. The easiest way to pump up your muscles is to put steroids in the supplement. Unfortunately, there are always a few unscrupulous companies that are only too willing to do just that.
Well, the chickens have come home to roost. It’s been a bad few weeks for the sports supplement industry. It seems like every time you turned around there was another article about a sports supplement making fraudulent claims, containing illegal ingredients, or actually harming people. It makes you wonder whether you should just completely avoid sports supplements all together.
That would be unfortunate because sports supplements can help with hydration, endurance and recovery. They can help you maximize the benefits of your exercise program. Furthermore, there are a lot of reputable sports supplement companies out there. The problem is that there are a few “bad apples” in the industry, and the FDA is not really doing its job to protect the American consumer from their deceptive and dangerous products.
Even worse, when the FDA acts, major retail nutrition stores often drag their feet at actually removing the products from their shelves (https://www.chaneyhealth.com/healthtips/are-dietary-supplements-safe/), and the unscrupulous manufacturers just switch to another equally dangerous stimulant.
It is, therefore, important for those of us who are nutrition educators to warn consumers like you about the dangerous products that are in the marketplace. The FDA will eventually act, but you need to know about those products now!
I have previously warned you about sports nutrition products containing the amphetamine-like stimulants DMAA (https://www.chaneyhealth.com/healthtips/are-dietary-supplements-safe/), DEPEA (https://www.chaneyhealth.com/healthtips/are-fat-burning-sports-supplements-safe/) and DMBA (https://www.chaneyhealth.com/healthtips/supplements-to-avoid/). As you might guess from the names, these are all structurally related compounds. They have several other characteristics in common:
- They are all synthetic amphetamine analogs.
- The sports nutrition companies selling products with these ingredients tried to fool the public (and the FDA) by claiming that they were natural components of the herbal ingredients in their product.
- None of them had ever been tested for safety and efficacy in humans. Some of them actually killed people before the FDA stepped in and banned them.
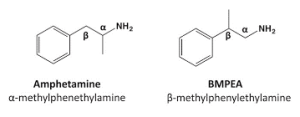
Amphetamine and amphetamine-like substances are popular in sports nutrition and weight loss products because they increase energy levels and speed up metabolism. Unfortunately, they also cause high blood pressure, arrhythmia, heart attacks and death.
Are Sports Supplements Safe? Yes and No.
 Sports Supplements Containing a Form of Amphetamine
Sports Supplements Containing a Form of Amphetamine
Yet another analog of DMAA called beta-methylphenethylamine (BMPEA) has appeared in the sports nutrition marketplace. It is an isomer of amphetamine that was first synthesized in the 1930’s. Because it is an analog of amphetamine, BMPEA is classified as a banned substance by the World Anti-Doping Agency. Unfortunately, its story is all too familiar.
The FDA first reported the presence of pharmacological doses of BMPEA in 43% of sports and weight loss supplements containing the herbal ingredient Acacia rigidula in 2012. The manufacturers claimed that the BMPEA in their products came from the Acacia rigidula even though there was no scientific evidence that it had ever been successfully extracted from Acacia rigidula.
BMPEA causes high blood pressure in animals and has never been tested for safety or efficacy in humans. Its close analog, DMAA, caused scores of deaths before the FDA finally banned it. However, the FDA did not warn consumers that supplements with the ingredient Acacia rigidula might contain BMPEA and might, therefore, be dangerous.
A group led by Dr. Pieter Cohen of Harvard University (Cohen et al, Drug Testing and Analysis, DOI: 10.1002/dta.1793, 2015) recently decided to analyze sports and weight loss supplements containing Acacia rigidula to see whether some companies had voluntarily removed DMPEA from their products over the last two years. One might hope that at least some of those companies might have been more motivated by protecting the health of their customers than by profit.
Not a chance! Dr. Cohen and his colleagues tested 21 products containing Acacia rigidula and found that 11 of them (52%) contained BMPEA – some in amounts as high as 94 mg/serving.
Dr. Cohen was quoted as saying “More than two years after the FDA’s discovery [of BMPEA in sports supplements], the FDA has yet to warn consumers about the presence of an amphetamine isomer in supplements. This is really about the FDA and why the FDA is not enforcing the law. This is a great example of how the FDA could so easily move now and not wait like it did with DMAA, wait until strokes and heart attacks had become front page news.”
After Dr. Cohen’s article became front page news several Senators called on the FDA to ban BMPEA. A week later the FDA finally caved in and announced that BMPEA was not a legal ingredient and that any products listing it on the label must be withdrawn from market. A skeptic might note that this was a full two years after the FDA discovered the existence of products containing BMPEA. The FDA’s announcement also did not cover BMPEA-containing products listing only Acacia rigidula on the label – which made up most of the BMPEA-containing products identified by Dr. Cohen and his colleagues. As the old saying goes, the FDA action was “a day late and a dollar short”.
Sports Supplements Containing Steroids
 A week later the FDA issued a warning to consumers to stop using a product call Tri-Methyl Extreme because of reports of serious liver damage in people using it. The product contained the anabolic steroids methyl-stenbolone, MAX LMG (a non-methylated prohormone) and epistane.
A week later the FDA issued a warning to consumers to stop using a product call Tri-Methyl Extreme because of reports of serious liver damage in people using it. The product contained the anabolic steroids methyl-stenbolone, MAX LMG (a non-methylated prohormone) and epistane.
There are two important take home lessons from this incident.
- The product actually claimed that it contained anabolic steroids. Anabolic steroids are known to cause liver damage, heart attack and stroke, testicular cancer, infertility and mood disorders. It is hard to imagine why anyone would use a product that claimed to contain anabolic steroids. Unfortunately, some people are willing to do almost anything that will increase muscle mass and strength.
- The FDA often only acts once a product has either seriously injured or actually killed people. I tend to agree with Dr. Cohen that it would be far preferable for the FDA to be proactive and warn consumers about products that have the potential to do harm.
Sports Supplements That Cause Cancer
As if that weren’t bad enough, at about the same time a paper was published reporting that use of muscle-building supplements by young men may increase their risk of testicular cancer by up to 177% (Li et al, British Journal of Cancer, DOI: 10.1038/bjc.2015.26).
The incidence of testicular germ cell cancer in men 15-39 years old has increased 1.6-fold between 1975 and 2011. The reason for that increase is not known, but the authors of British Journal of Cancer article noted that the use of performance-enhancing supplements in that group has also increased dramatically during the same time period.
A previous study of testicular cancer patients reported that a high percentage of them (~20%) had used performance-enhancing supplements, but no control group was included in that study. Thus, the authors of this study set out to carefully match testicular cancer patients with healthy men of the same age and demographics – something we scientists call a case-control study.
The study compared 356 testicular cancer patients age 18-55 from Connecticut and Massachusetts with 513 controls that were matched by age, race, education, tobacco and alcohol use, exercise level, injury to testes or groin, and family history of testicular cancer. The results were pretty scary.
- Use of muscle building supplements increased the risk of testicular cancer by 65% compared to men who never used that kind of supplement.
- For men who started using muscle building supplements before they were 25, the risk of developing testicular cancer increased by 121%.
- For men who used muscle building supplements for more than 3 years, the risk increased to 156%.
- For men who used more than 2 types of muscle building supplements, the risk increased to a whopping 177%. That’s almost double.
This study did not identify the actual ingredients that caused the increased testicular cancer risk, but with so many of the muscle-building supplements on the market containing dangerous and/or illegal ingredients it is perhaps not surprising that they might increase cancer risk. After all, this demographic (young males) is the group most likely to choose the “Monster Muscle Builder” products rather the less glamorous, but safer, sports supplements.
Sports Supplements That Mislead
 At the same time that we were hearing about sports supplements with dangerous and illegal ingredients and sports supplements that may cause cancer, the Advertising Standards Authority (the British equivalent of the FTC) accused a British sports supplement company of making false and misleading ingredient claims. That’s a polite way of saying they were lying!
At the same time that we were hearing about sports supplements with dangerous and illegal ingredients and sports supplements that may cause cancer, the Advertising Standards Authority (the British equivalent of the FTC) accused a British sports supplement company of making false and misleading ingredient claims. That’s a polite way of saying they were lying!
In particular, they disallowed claims that:
- CLA builds lean muscle and attacks fat stores, promotes fat loss, improves mood and focus and boosts energy.
- Acetyl-L-Carnitine aids weight loss, burns fat, boosts energy, improves mental performance, and improves focus.
There were more claims they disallowed (click here for the complete report) (http://www.asa.org.uk/Rulings/Adjudications/2015/4/Protein-World-Ltd/SHP_ADJ_288571.aspx#.VS2VbJOk9RN), but I included those two because you’ve probably seen similar claims for those ingredients on this side of the Atlantic. Those claims are just as bogus in the United States as they are in England.
How To Choose A Sports Supplement Company You Can Trust
 By now you are probably convinced that you should never use a sports supplement product again. However, as I said above good sports supplements properly used can improve hydration, endurance, recovery and the results you obtain from your exercise program. Here are the questions to ask. Are sports supplements safe? They can be. Which sports nutrition products can you trust? Here are some simple guidelines to help you choose a trustworthy sports supplement company.
By now you are probably convinced that you should never use a sports supplement product again. However, as I said above good sports supplements properly used can improve hydration, endurance, recovery and the results you obtain from your exercise program. Here are the questions to ask. Are sports supplements safe? They can be. Which sports nutrition products can you trust? Here are some simple guidelines to help you choose a trustworthy sports supplement company.
- Avoid the hyped claims. If the supplement makes claims like “Get ripped fast”, “Intense Energy”. “Extreme Energy”, “Eviscerate fat”, “Makes fat cells self-destruct” or “boosts testosterone”, you should run the other direction.
- Ignore testimonials. The placebo effect is close to 50% for things like energy, and if an athlete “thinks” they have more energy every time they work out, they will get stronger.
- Look for published clinical studies showing that the product is safe and effective. Those clinical studies should be published in peer-reviewed scientific journals. If the company just cites their own “studies” or “white papers”, ignore them. They may look impressive, but they have not been peer reviewed. You have no idea whether they are accurate.
- I could tell you to look for rigorous quality control standards, but every company claims they have excellent quality controls. Instead I will tell you to look for supplements that are used by medal winning Olympic athletes. Why Olympic athletes? That is because Olympic athletes are more rigorously drug tested than any other athlete. They absolutely cannot afford to have any stimulants, steroids or other banned substances in their body at any time. They need products that are pure, safe and effective.
- Finally, avoid products with artificial ingredients. While the risks associated with artificial sweeteners, artificial flavors and artificial colors are not as great as the risks associated with stimulants and steroids, they are still ingredients to be avoided. We simply do not know the long term health consequences of artificial ingredients.
The Bottom Line
- There are a few bad apples in every barrel, and the sports supplement industry is no exception. Are sports supplements safe? Over one two-week period lately we have learned:
- Over 50% of sports nutrition products labeled as containing an innocuous sounding herbal ingredient were actually found to contain an amphetamine isomer called BMPEA that has been banned by the World Anti-doping Agency. After years of dragging its feet, the FDA finally banned some of the products containing BMPEA, but left many others on the market. As the old saying goes, the FDA was “a day late and a dollar short”.
- Even though they are extremely dangerous, new sports supplements with anabolic steroids keep popping up online. Once again, the FDA has had to warn consumers not to use a new muscle building supplement containing steroids because several people using that supplement suffered severe liver damage.
- A study reported that young men who use muscle building supplements may increase their risk of testicular cancer by up to 177%.
- The British equivalent of our FTC has told a British sports supplement manufacturer that it must stop making false and misleading claims about ingredients like CLA and acetyl-L-carnitine. That is noteworthy because some sports supplement companies in the US make very similar claims for the same ingredients.
- You shouldn’t necessarily avoid sports supplements because of a few bad apples. Good sports supplements properly used can improve hydration, endurance, recovery and the results you obtain from your exercise program. There are a few simple guidelines that can help you choose the good sports supplement companies and avoid the bad ones:
- Avoid the hyped claims.
- Ignore testimonials.
- Look for published clinical studies showing that the product is safe and effective.
- Look for supplements that are used by medal winning Olympic athletes. That’s because Olympic athletes absolutely need products that are pure, safe and effective.
- Avoid products with artificial ingredients.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.