Author: Dr. Stephen Chaney
 Some athletes, particularly Olympic athletes, are starting to use resveratrol to improve their workouts and their performance in events. Is their belief in the benefits of resveratrol justified, or is resveratrol just another of those “mythical” sports nutrition supplements? There have only been a few small studies on the subject, and those studies have been conflicting.
Some athletes, particularly Olympic athletes, are starting to use resveratrol to improve their workouts and their performance in events. Is their belief in the benefits of resveratrol justified, or is resveratrol just another of those “mythical” sports nutrition supplements? There have only been a few small studies on the subject, and those studies have been conflicting.
The study I am featuring this week (Polley et al, Appl. Physiol. Nutr. Metab. 41: 26-32, 2016) asked a more fundamental question. It asked whether resveratrol enhanced the effect of exercise on muscle mitochondrial capacity. For those of you who aren’t scientists that statement may require some interpretation.
What Are Mitochondria and Why Are They Important?
You can think of mitochondria as the power packs of the cell. They are tiny organelles that are found in most cells in our body. The foods that we eat contain a lot of energy (calories), but that energy is not in a form that our cells can use. Our cells metabolize those foods into small molecules that donate electrons to our mitochondria, and the mitochondria use those electrons to create energy in a form that our cells can utilize.
As you might imagine, mitochondria are particularly important for cells with high energy requirements, like our muscle cells. Those muscle cells responsible for endurance and high intensity (think gymnastics or weight lifting) exercise have the highest density of mitochondria and are the most dependent on those mitochondria for optimal performance.
Why Resveratrol Might Increase Muscle Mitochondrial Capacity?
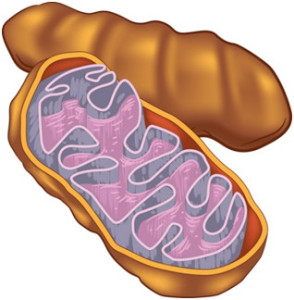 Mitochondria have a finite lifetime in our cells. As our cells age their mitochondria become less efficient and start doing bad things like releasing damaging free radicals into the cell. Exercise stress causes the mitochondria in our muscles to age more rapidly than the mitochondria in other cells. Fortunately, regular exercise also stimulates a pathway that causes production of new mitochondria and enhances their efficiency. Thus, the net effect of any exercise program is to increase both the number and efficiency of mitochondria, something referred to as mitochondrial capacity.
Mitochondria have a finite lifetime in our cells. As our cells age their mitochondria become less efficient and start doing bad things like releasing damaging free radicals into the cell. Exercise stress causes the mitochondria in our muscles to age more rapidly than the mitochondria in other cells. Fortunately, regular exercise also stimulates a pathway that causes production of new mitochondria and enhances their efficiency. Thus, the net effect of any exercise program is to increase both the number and efficiency of mitochondria, something referred to as mitochondrial capacity.
It turns out that resveratrol and a small group of related polyphenols also stimulate the same pathway. Animal and cell culture studies show that resveratrol can increase muscle mitochondrial capacity. However, since resveratrol and exercise increase mitochondrial capacity by the same mechanism, the question is whether resveratrol has any added benefit over exercise alone. That is the question this study was designed to answer.
The Benefits of Resveratrol on Muscle Mitochondrial Capacity?
Previous studies had suggested that one of the benefits of resveratrol might be increasing muscle mitochondrial capacity for people who have engaged in relatively little physical activity in the past. For examples, studies have shown that resveratrol activates the pathway leading to increased mitochondrial capacity in obese and diabetic populations, both groups that may not have been involved in regular exercise. In contrast, other studies found no enhancement of those same pathways compared to exercise alone in more highly trained populations involved in high intensity training.
 Based on those results, the present study (Polley et al, Appl. Physiol. Nutr. Metab. 41: 26-32, 2016) was specifically designed to assess the effect of resveratrol supplementation along with low-intensity exercise in an untrained muscle group. The authors recruited healthy young adults with approximately equal numbers of men and women. To assure that the muscle group was relatively untrained, they asked the subjects to perform wrist flexor exercises in their non-dominant arm. They excluded from the study anyone whose exercise regimen involved regular use of the non-dominant forearm such as rowing, rock climbing or CrossFit.
Based on those results, the present study (Polley et al, Appl. Physiol. Nutr. Metab. 41: 26-32, 2016) was specifically designed to assess the effect of resveratrol supplementation along with low-intensity exercise in an untrained muscle group. The authors recruited healthy young adults with approximately equal numbers of men and women. To assure that the muscle group was relatively untrained, they asked the subjects to perform wrist flexor exercises in their non-dominant arm. They excluded from the study anyone whose exercise regimen involved regular use of the non-dominant forearm such as rowing, rock climbing or CrossFit.
This was a double-blind, placebo-controlled study. Half of the group received 500 mg of resveratrol and the other half received the placebo. The placebo group served as a control for the effect of exercise alone. The dominant arm was not exercised, so it served as a control for the effect of resveratrol alone. The participants took resveratrol or placebo upon wakening each morning. The wrist flexor exercises were performed 3 times per week for 4 weeks. Mitochondrial capacity measurements were made using near infrared spectroscopy on a weekly basis.
The results were pretty straight-forward.
- Low-intensity training alone (placebo group) for 4 weeks resulted in a 10% increase in mitochondrial capacity.
- Low-intensity training plus resveratrol for 4 weeks resulted in a 40% increase in mitochondrial capacity. This represented a highly significant difference between the resveratrol and placebo groups.
- Neither the resveratrol group or the placebo group exhibited changes in the untrained arm, which suggests that resveratrol without exercise has little or no effect on mitochondrial capacity in young, healthy subjects.
The authors concluded: “Taken together, these findings indicate that [the] combination of exercise and resveratrol is needed for eliciting maximal muscle mitochondrial adaptations to low-intensity training programs.”
What Are the Strengths and Weaknesses of This Study?
Strengths:Because previous studies had suggested that the effects of resveratrol might be masked in highly trained individuals or by high intensity exercise, this study was specifically designed to look at the effects of resveratrol on mitochondrial capacity when administered along with low-intensity exercise in untrained muscles. In that sense this study breaks new ground and suggests that, under the right conditions, resveratrol can enhance exercise training.
Weaknesses:The weaknesses of this study were many:
- It was a very small study. That is not unusual in this area of research, but clearly much more research is needed.
- It used a higher dose of resveratrol than previous studies. However, plasma levels of resveratrol were not determined and the effect of lower doses was also not determined, so we have no idea how much resveratrol is actually needed to elicit this response.
- While increased mitochondrial capacity is a probable predictor of improved exercise efficiency, no performance outcomes were actually measured. Most people probably don’t care how well their mitochondria work. They care about how well their muscles perform.
What Does This Mean For You?
We are in the very early stages of research into the benefits of resveratrol on exercise. Many more studies are needed before we will be in a position to fully understand the effects of resveratrol on exercise efficiency and performance outcomes. This and previous studies suggest that resveratrol is likely to be most effective at enhancing exercise efficiency with low intensity exercise in relatively untrained muscles.
If true, that would mean resveratrol might be helpful for the millions of Americans who are “weekend warriors” or exercise sporadically. It may even be beneficial for those of us who exercise regularly at a low to moderate intensity level.
However, because resveratrol and exercise improve mitochondrial capacity by the same mechanism, previous studies suggest that resveratrol might be a less effective addition for highly trained athletes engaged in high-intensity exercise.If true, this would put resveratrol in the same category as several other popular exercise supplements such as arginine and citrulline that also appear to be more effective for untrained individuals than they are for highly trained athletes.
However, I am aware of many Olympic athletes who use and swear by a resveratrol polyphenol blend. It could be placebo, but it could also suggest that resveratrol does enhance performance for highly trained athletes engaged in high-intensity exercise. As I said at the beginning of this section, there is much more research to do. That’s what makes science so much fun. There are always new things to learn.
The Bottom Line
We are in the very early stages of research into the benefits of resveratrol on exercise. Many studies will be needed before we will be in a position to fully understand the effects of resveratrol on exercise efficiency and performance outcomes. However, a recent study is of interest because it introduces a new perspective to our understanding of the possible effects of resveratrol on exercise efficiency.
- Thisstudy reports that resveratrol significantly enhances the increase in mitochondrial capacity caused by low-intensity exercise in untrained muscles
- If true, that would mean resveratrol might increase exercise efficiency for the millions of Americans who are “weekend warriors” or exercise sporadically. It may even be beneficial for those of us who exercise regularly at a low to moderate intensity level.
- However, because resveratrol and exercise improve mitochondrial capacity by the same mechanism, previous studies suggest that resveratrol might be a less effective addition for highly trained athletes engaged in high-intensity exercise.
- If true, this would put resveratrol in the same category as several other popular exercise supplements such as arginine and citrulline that also appear to be more effective for untrained individuals than they are for highly trained athletes.
- However, I am aware of many Olympic athletes who use and swear by a resveratrol polyphenol blend. It could be placebo, but it could also suggest that resveratrol does enhance performance for highly trained athletes engaged in high-intensity exercise.
As I said before, there is much more research to do. That’s what makes science so much fun. There are always new things to learn.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.