Can You Cut Your Risk Of Heart Disease And Diabetes In Half?
Author: Dr. Stephen Chaney
 It is no secret that heart disease and diabetes are among the top two causes of death in this country. They are killers. Even worse, they can affect your quality of life for years before they kill you. Finally, they are bankrupting our health care system. Anything we can do to reduce the toll of these diseases would be of great benefit.
It is no secret that heart disease and diabetes are among the top two causes of death in this country. They are killers. Even worse, they can affect your quality of life for years before they kill you. Finally, they are bankrupting our health care system. Anything we can do to reduce the toll of these diseases would be of great benefit.
Is there a connection between diet and chronic disease, specifically type 2 diabetes, stroke, and heart disease?
That is why recent headlines suggesting that deaths due to heart disease, stroke, and diabetes could be cut almost in half simply by changing our diet caught my attention. Of course, those headlines came as no surprise. It almost seems like the American diet is designed to make us fat and unhealthy. It seems designed to make us die prematurely from heart disease, stroke, and diabetes.
How Was The Study Done?
 This was a major study (R. Micha et al, JAMA, 317: 912-924, 2017 ). They started by using something called the National Health and Nutrition Examination Survey (NHANES). NHANES is a major survey conducted approximately every 10 years by the US government to collect data on demographics, disease, and diet from a cross section of the US population. They used this database to determine how frequently Americans consumed various heart-healthy and heart-unhealthy foods. They collected data from two surveys conducted in 1999-2002 and 2009-2012 to determine how consumption of those foods had changed over that 10-year period.
This was a major study (R. Micha et al, JAMA, 317: 912-924, 2017 ). They started by using something called the National Health and Nutrition Examination Survey (NHANES). NHANES is a major survey conducted approximately every 10 years by the US government to collect data on demographics, disease, and diet from a cross section of the US population. They used this database to determine how frequently Americans consumed various heart-healthy and heart-unhealthy foods. They collected data from two surveys conducted in 1999-2002 and 2009-2012 to determine how consumption of those foods had changed over that 10-year period.
- The heart-healthy foods they included in their study were fruits, vegetables, nuts & seeds, whole grains, and seafood omega-3s (long chain omega-3s).
- The heart-unhealthy foods they included in their study were red meats, processed meats, sugar-sweetened beverages, and sodium.
They then did a meta-analysis of high quality clinical studies measuring the effects of those foods on deaths due to heart disease, stroke, and diabetes. They combined the data from all these studies to calculate the deaths due to all three causes combined, something they called deaths due to cardiometabolic disease.
Diet and Chronic Disease, Preventing Type 2 Diabetes and Heart Disease
 When the investigators combined all the data, they estimated that changing one’s diet from heart-unhealthy foods to heart-healthy foods would reduce cardiometabolic deaths (deaths due to heart disease, stroke, and diabetes) by 45.4%. That is an almost 50% reduction just by eating a healthier diet.
When the investigators combined all the data, they estimated that changing one’s diet from heart-unhealthy foods to heart-healthy foods would reduce cardiometabolic deaths (deaths due to heart disease, stroke, and diabetes) by 45.4%. That is an almost 50% reduction just by eating a healthier diet.
- This probably underestimates the benefit of eating a healthier diet because they did not include the effects of reducing saturated fats, sweets, and refined carbohydrates on cardiometabolic deaths.
- The reduction in cardiometabolic deaths was consistent across all demographic groups. It ranged from 40% to 60% when they considered gender, age, or ethnicity.
- The 45.4% reduction in cardiometabolic deaths represents a holistic change to a healthier diet. When you consider the individual components of the standard American diet:
- Decreasing sodium intake gives a 9.5% reduction in deaths.
- Increasing intake of nuts and seeds gives an 8.5% reduction in cardiometabolic deaths.
- Decreasing intake of processed meats gives an 8.2% reduction in cardiometabolic deaths.
- Increasing intake of vegetables gives a 7.6% reduction in cardiometabolic deaths.
- Increasing intake of fruits gives a 7.5% reduction in cardiometabolic deaths.
- Decreasing intake of sugar-sweetened beverages gives a 7.4% reduction in cardiometabolic deaths.
- Increasing intake of whole grains gives a 5.9% reduction in cardiometabolic deaths.
- Decreasing red meat consumption gives a 4.2% decease in diabetes deaths. They did not include the effect of red meat consumption on heart disease or stroke deaths in their calculation.
 Holistic changes are best: It would be easy to look at each of those individual changes and conclude that the change is so small that it isn’t worth the effort. That would be totally missing the point. These data clearly show a relationship between diet and chronic disease:
Holistic changes are best: It would be easy to look at each of those individual changes and conclude that the change is so small that it isn’t worth the effort. That would be totally missing the point. These data clearly show a relationship between diet and chronic disease:
- A holistic change in diet that includes all these individual changes can make a huge difference in your risk of dying from heart disease, stroke, or diabetes.
- Even if you are not prepared to make this many changes at once, each individual change gets you one step closer to a longer, healthier life. In fact, if you make just one or two of these changes you have reduced your risk of dying more than if you were taking a statin drug – and with no side effects.
The good news is that Americans have made some positive changes in their diet between the first and second NHANES survey, and, as a result, cardiometabolic deaths declined by 26.5%. The biggest contributors to this improvement were:
- Increased polyunsaturated fat consumption (-20.8%).
- Increased nut and seed consumption (-18%).
- Decreased sugar sweetened beverage consumption (-14.5%).
- This was partially offset by increased processed meat consumption (+14.4%)
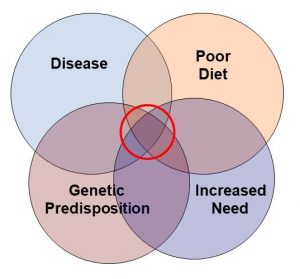
The authors concluded: “Dietary factors were estimated to be associated with a substantial proportion of deaths from heart disease, stroke, and type 2 diabetes. These results should help identify priorities, guide public health planning, and inform strategies to alter dietary habits and improve health.” Below is a summary of the relationship between diet and chronic disease (specifically type 2 diabetes, stroke, and heart disease).
The Bottom Line
It almost seems like the American diet is designed to make us fat and unhealthy. It seems designed to make us die prematurely from heart disease, stroke, and diabetes. A recent study looked at the effect of a healthier diet on what they called cardiometabolic deaths (deaths due to heart disease, stroke, and diabetes). They concluded:
- changing one’s diet from heart-unhealthy foods to heart-healthy foods would reduce cardiometabolic deaths by 45.4%. That is an almost 50% reduction just by eating a healthier diet.
- This probably underestimates the benefit of eating a healthier diet because they did not include the effects of reducing saturated fats, sugary foods, and refined carbohydrates on cardiometabolic deaths.
- The reduction in cardiometabolic deaths was consistent across all demographic groups. It ranged from 40% to 60% when they considered gender, age, or ethnicity.
- The 45.4% reduction in cardiometabolic deaths represents a holistic change to a healthier diet. When you consider the individual components of the standard American diet:
- Decreasing sodium intake gives a 9.5% reduction in deaths.
- Increasing intake of nuts and seeds gives an 8.5% reduction in cardiometabolic deaths.
- Decreasing intake of processed meats gives an 8.2% reduction in cardiometabolic deaths.
- Increasing intake of vegetables gives a 7.6% reduction in cardiometabolic deaths.
- Increasing intake of fruits gives a 7.5% reduction in cardiometabolic deaths.
- Decreasing intake of sugar-sweetened beverages gives a 7.4% reduction in cardiometabolic deaths.
- Increasing intake of whole grains gives a 5.9% reduction in cardiometabolic deaths.
- Decreasing red meat consumption gives a 4.2% reduction in diabetes deaths. They did not include the effect of red meat consumption on heart disease or stroke deaths in their calculation.
It would be easy to look at each of those individual changes and conclude that the change is so small that it isn’t worth the effort. That would be totally missing the point. These data clearly show:
- A holistic change in diet that includes all these individual changes can make a huge difference in your risk of dying from heart disease, stroke, or diabetes.
- Even if you are not prepared to make this many changes at once, each individual change gets you one step closer to a longer, healthier life. In fact, if you make just one or two of these changes you have reduced your risk of dying more than if you were taking a statin drug – and with no side effects.
The authors concluded: “Dietary factors were estimated to be associated with a substantial proportion of deaths from heart disease, stroke, and type 2 diabetes. These results should help identify priorities, guide public health planning, and inform strategies to alter dietary habits and improve health.”
For more details, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.