Probiotics and Hero Bacteria
Author: Dr. Stephen Chaney
 Suddenly the term “microbiome” is hot. It is featured in books, internet articles, and marketing materials produced by supplement companies wanting to sell their “magic” probiotic supplements. But, you are confused. You don’t know if what you read is true or just marketing hype. What is your microbiome anyway?
Suddenly the term “microbiome” is hot. It is featured in books, internet articles, and marketing materials produced by supplement companies wanting to sell their “magic” probiotic supplements. But, you are confused. You don’t know if what you read is true or just marketing hype. What is your microbiome anyway?
You have been asking me: “What is my microbiome? “Why is it important?” “How does it affect my health?” “Should I take a probiotic?” “What else should I do?”
I covered this topic in a section of my book, “Slaying The Food Myths” called “Our Mighty Microbiome.” However, this is an exploding area of scientific research. Published papers on our microbiome have increased by 600% in just the past 10 years. I already need to update the information in my book.
What Is Your Microbiome?
 Your microbiome is defined as the community of microorganisms (bacteria, yeast and other fungi, and viruses) that live in and on you. Most of those microorganisms are bacteria, and most of them reside in your large intestine. Thus, the term “gut bacteria” is a useful and easier to understand approximation.
Your microbiome is defined as the community of microorganisms (bacteria, yeast and other fungi, and viruses) that live in and on you. Most of those microorganisms are bacteria, and most of them reside in your large intestine. Thus, the term “gut bacteria” is a useful and easier to understand approximation.
We are just beginning to understand just how complex and diverse our microbiome community is. Each of us harbor about 38 trillion microorganisms (give or take a few trillion). That means we each have slightly more microorganisms than we do cells in our body. However, it is not just the sheer number of microorganisms that is impressive. It is the number of different species we harbor in our bodies that indicates the true complexity of our microbiome.
For example, we each have more than 1,000 different species of bacteria in our large intestine. Collectively, these bacteria have around 750,000 unique genes. That is 30 times more than the human genome. Even so, understanding the health implications of our microbiome would be relatively simple if we all had the same species of bacteria in our intestines, but we don’t.
We are all unique. We all have different species in our intestines. The only simplifying principle is that these bacteria seem to exist as in distinct communities that generally group together. Even so, our microbiomes are amazingly complex.
We Are What We Eat
 You have probably heard the phrase “We are what we eat” before and dismissed it. After all, we can eat carrots all day long, and we will never turn into a carrot. However, that phrase is literally true when we consider our microbiomes. For example, the microbiomes of meat-eaters have totally different families of microorganisms than microbiomes of vegetarians. We don’t yet fully understand the implications of these differences in gut bacteria. However, we think they may be responsible for some of the differences in health outcomes of meat eaters and vegetarians.
You have probably heard the phrase “We are what we eat” before and dismissed it. After all, we can eat carrots all day long, and we will never turn into a carrot. However, that phrase is literally true when we consider our microbiomes. For example, the microbiomes of meat-eaters have totally different families of microorganisms than microbiomes of vegetarians. We don’t yet fully understand the implications of these differences in gut bacteria. However, we think they may be responsible for some of the differences in health outcomes of meat eaters and vegetarians.
Our microbiomes are also influenced by individual foods in our diet. In part, that is because each food has a unique blend of fibers. To fully comprehend the significance of that statement, we need to understand what fibers do. Most of us think of fibers as the indigestible portion of foods. We think of it as “roughage” that helps keeps our intestines moving and binds toxins, so they can be eliminated safely. That is true, but fiber is much more.
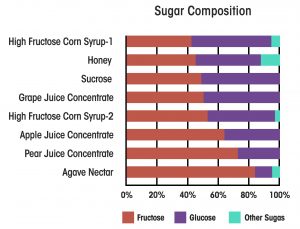
While we can’t digest fiber, the microorganisms living in our intestine can digest much of it. That fiber becomes food for the microorganisms. We refer to food for our intestinal microorganisms as “prebiotics.” That means you probably need to rethink what the term prebiotic really means.
In the past you have probably thought of prebiotics as supplements designed to support the growth of certain bacteria in our intestines. Now you know that prebiotic also refers to the fibers in the foods we eat. Because each food has a unique blend of fibers, each food supports the growth of slightly different populations of intestinal bacteria. This helps explain why the human microbiome is so complex.
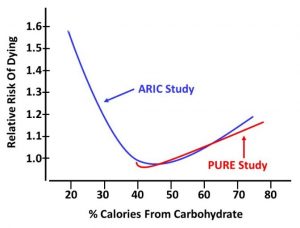
We don’t fully understand the health consequences of these differences in our microbiome, but we think they are huge (see below). This is one reason I do not recommend any diet that eliminates whole food groups. It is easy to say we can replace the missing nutrients with a multivitamin. But, what about the missing fiber? We know that will affect our microbiome. We simply don’t know enough about the long-term health consequences of altering our microbiome to recommend eliminating high fiber foods from our diet. It’s not nice to fool with Mother Nature.
For example, in “Slaying The Food Myths” I discussed the evidence that meat-based low-carb diets are less healthy long term than primarily plant-based low-carb diets. That could be because of saturated fats and excess consumption of red meat. However, it might also be caused by the effect on the microbiome of the food groups that are eliminated in meat-based, low-carb diets.
Finally, as if all of this weren’t complex enough, there is some evidence that our microbiome is influenced by lifestyle (particularly obesity and exercise) and environment (particularly toxins in the environment). But, that’s another topic for another day.
Why Is Your Microbiome Important?
 Now you know that our microbiome is incredibly complex. You also know “We are what we eat.” Why are those two things important? While there is a lot we don’t yet know, it appears that our microbiome has a powerful influence on our health.
Now you know that our microbiome is incredibly complex. You also know “We are what we eat.” Why are those two things important? While there is a lot we don’t yet know, it appears that our microbiome has a powerful influence on our health.
For example, we know that our gut bacteria can convert components of the foods we eat into compounds that are absorbed into our bloodstream and either have a positive or negative effect on our health. Let me give you some specific examples:
- “Good” intestinal bacteria produce butyrate in the process of digesting fiber. Butyrate, in turn, is thought to support intestinal health and activate genes that lower blood cholesterol levels.
- “Bad” intestinal bacteria convert carnitine (a normal human metabolite found in meat, particularly red meat) into trimethylamine-N-oxide or TMAO, which is thought to increase the risk of heart disease. In a cruel twist of fate, these particular “bad” bacteria seem to be prevalent in the microbiome of meat-eaters, but absent from the microbiome of vegetarians.
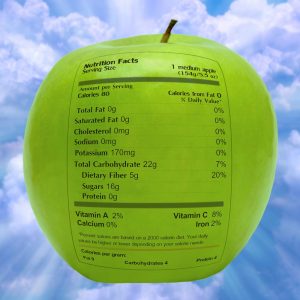
- We have been told that polyphenols are good for us. However, polyphenols are poorly absorbed. Fortunately, polyphenols are rapidly metabolized by our microbiome into metabolites that are more easily absorbed. Many experts think it is those microbiome-produced metabolites that are responsible for the health benefits of polyphenols. If everyone’s microbiome is different, how does that affect the health benefits of polyphenols. A recent study puts this into perspective. The authors fed an apple extract to 12 individuals and measured 110 polyphenol metabolites in their blood over the next 5 hours. The pattern of blood metabolites was different for every individual in the study. Furthermore, the pattern of blood metabolites correlated with differences in the species of bacteria in their intestine.
I have given examples of 3 different kinds of food-microbiome interactions here. There are more examples of each type of food-microbiome interaction in the literature. This just adds another layer of complexity. Not only does the food we eat affect our microbiome, but our microbiome influences how we metabolize the foods we eat. We are just beginning to understand how these differences influence our health. However, based on what we currently know, here are some of the ways our microbiome can influence our health:
Current evidence suggests that “bad” bacteria and yeast in our intestines may:
- Compromise our immune system.
- Create a “leaky gut”, which allows partially digested foods to get into the bloodstream where they can trigger inflammation and auto-immune responses.
- Adversely affect brain function and moods.
- Convert components of the foods we eat into compounds which increase the risk of cancer and heart disease.
- Perhaps, even make us fat.
In contrast, “good” bacteria:
- Crowd out the bad bacteria and prevent the health problems they cause.
- Break down undigested fiber into compounds that are beneficial to our health.
What About Probiotics?
 Now you know how important our microbiome is to our health, you are probably wondering whether you should add one or more probiotic supplements to your health regimen. Let me give you a brief primer on probiotic supplements.
Now you know how important our microbiome is to our health, you are probably wondering whether you should add one or more probiotic supplements to your health regimen. Let me give you a brief primer on probiotic supplements.
“Hero Bacteria”: We have over 1,000 species of bacteria in our microbiome, and they work together in families. With that complexity, you may be wondering how someone could hope to create a probiotic supplement that worked. Fecal transplants (all the intestinal bacteria from a healthy individual) have been used for some life-threatening conditions, but I don’t think that is an approach most of us want to consider.
For better or worse, modern science uses a reductionist approach. We focus on a single component of a system and test its effectiveness in clinical studies. In the probiotic world, we focus on an individual strain of bacteria. If it proves effective in clinical studies, it is given a name and is used in probiotic supplements. It becomes what I call a “hero bacteria.”
For example, if scientists were looking for a probiotic supplement to aid with digestion or immunity, they would test dozens of strains initially. They would then select the one strain for further study. It may have been selected because it performed best in the preliminary studies. However, it may have been selected based on other characteristics, such as how easy it was for the scientist to grow in a culture dish. That strain is then put through rigorous clinical trials. If it performs well there, it becomes a “hero bacteria” suitable for a probiotic supplement. It has been “proven” to provide a specific benefit to our health.
However, it is not the only bacteria to provide that benefit. It might not have even been the “best” bacteria. It may have simply been the one that grew best in the lab.
Rule #1: Look for one or more named “hero bacteria” in your probiotic supplement. They have been proven to provide a specific health benefit.
Not All “Hero Bacteria” Are Created Equal: In some cases, companies that have developed a particular strain of “hero bacteria” have published the clinical studies supporting their claims in peer-reviewed journals. In other cases, they make the study claims, but say their data is “proprietary.” I am a skeptic. If they haven’t published their data, I assume it wasn’t good enough to be published.
Rule #2: Avoid any probiotic supplements that do not provide you with studies published in peer-reviewed scientific journals showing that studies with their “hero bacteria” support their product claims.
Some Companies Get Ahead Of What Good Science Supports: Their claims sound amazing, but they aren’t supported by clinical proof. They call it marketing. I call it lying.
In some cases, the lying is clear because they don’t provide you with clinical studies published in peer-reviewed journals.
However, if their claims sound too good to be true and they have provided clinical studies published in peer-reviewed journals, my advice is to read the studies. You don’t need to be an expert. The abstracts for every published article are available online. Read the abstract and see what health claims it makes. [Reviewers of peer-review articles generally insist that the claims match the evidence.] If a company’s marketing claims exceed the claims from the published studies backing their product, they are probably lying to you.
Rule #3: If a company’s marketing claims exceed the claims from the published studies backing their product, run the other direction. They are lying to you.
It Takes A Village: While it is useful to have one or more “hero bacteria” in your probiotic supplement, don’t assume that is all you need. Remember that you have many more than one or two bacteria in your gut. You have a thousand or more different species. For every “hero bacteria” that has gone through the clinical review process, there are dozens more that provide the same benefit, and they all work together. More importantly, they work by different mechanisms. You need a holistic approach to creating a healthier microbiome.
My recommendation is to choose probiotic supplements that contain several species that work together rather than just a single “hero bacteria.” I also recommend following a diet that supports a healthy microbiome. Based on what we currently know, that would be a primarily plant-based diet containing all five food groups.
Rule #4: Choose probiotic supplements that contain several species that work together rather than a single “hero bacteria”.
The Bottom Line
Because I know how confusing the term “microbiome” is to most of you I have written a brief overview of our microbiome and what it does. Topics I have covered are:
- What is our microbiome?
- How do the foods we eat influence our microbiome?
- How does our microbiome influence the metabolism of the foods we eat?
- How does our microbiome influence our health?
- How do you select a good probiotic supplement?
If any of these topics interest you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.