Do Omega-3s Reduce Risk Of Heart Disease & Cancer?
Author: Dr. Stephen Chaney
Are omega-3 supplements good for you?
 You have every right to be confused. In the late 1990s and early 2000s several major clinical studies showed that omega-3 supplements reduced the risk of heart attacks and stroke. In contrast, a few months ago a major study called ASCEND was published that failed to find any benefit of omega-3s at reducing heart disease risk. The headlines said “Omega-3 Supplements Don’t Protect Against Heart Disease”. You were told that omega-3 supplements were worthless. I pointed out the weakness of that study in a previous issue of “Health Tips From the Professor”.
You have every right to be confused. In the late 1990s and early 2000s several major clinical studies showed that omega-3 supplements reduced the risk of heart attacks and stroke. In contrast, a few months ago a major study called ASCEND was published that failed to find any benefit of omega-3s at reducing heart disease risk. The headlines said “Omega-3 Supplements Don’t Protect Against Heart Disease”. You were told that omega-3 supplements were worthless. I pointed out the weakness of that study in a previous issue of “Health Tips From the Professor”.
In mid-November two more major clinical studies were published. However, if you rely on the media for your information on supplementation, you are probably still confused. Headlines ranged from “Omega-3 Supplements Do Not Prevent Cancer Or Heart Disease” to “Eating More Fish Or Taking Omega-3 Fish Oil Supplements Can Cut Heart Attack Risk.” What is the truth?
The problem is that reporters aren’t scientists. They don’t know how to interpret clinical studies. What they report is filtered through their personal biases. That is why I take the time to carefully evaluate the clinical studies, so I can provide you with accurate information. Let me sort through the dueling headlines and give you the truth about omega-3s.
Note: One of the clinical studies looked at the effect of omega-3s on both cancer and heart disease risk. I will discuss the cancer results briefly, but most of my focus will be on the heart disease findings.
How Were The Studies Designed?
The VITAL STUDY (JE Manson et al, New England Journal of Medicine, DOI: 10.1056/NEJMoa1811403 )in the United States. The study participants were 50% female, 50% male, and 20% African American. None of the participants had pre-existing heart disease. The characteristics of the study group were typical of the American population at that age, namely:
- The average BMI was 28, which means that most of the participants were significantly overweight.
- 7% of them had diabetes.
- 38% were on cholesterol-lowering medications.
- 50% had high blood pressure treated by medication.
Study participants were given questionnaires on enrollment to assess clinical and lifestyle factors including dietary intake. Blood samples were taken from about 50% of the participants to determine omega-3 index at baseline and at the end of the first year. The participants were given a high purity omega-3 supplement (1 gram capsules containing 840 mg of total omega-3s, 460 mg of EPA, and 380 mg of DHA as the ethyl esters) or a placebo and followed for an average of 5.3 years.
There were two important characteristics of this study that distinguished it from the negative ASCEND study.
- This study specifically excluded cardiovascular drugs other than statins and blood pressure medications because many of those drugs provide the same benefits as omega-3s. Patients in the ASCEND study were on 3-5 heart medications
- The omega-3 status of participants at the beginning of this study was very low. The omega-3 status of participants in the ASCEND study was near optimal at the beginning of the study.
The REDUCE-IT study (DL Bhatt et al, New England Journal Of Medicine, DOI:10.1056/NEJMoa1812792 ): This study enrolled 8,179 participants (average age = 64) from several countries. The study participants were 70% male and 90% white. The average BMI was 31, which is considered obese. This study differed from the VITAL study in that all the patients were at high risk of heart disease.
- 70% of them had preexisting heart disease.
- The remaining 30% had diabetes plus at least one additional risk factor for heart disease.
- In addition, all of them had elevated triglycerides, which is an independent risk factor for heart disease.
The participants were given a high purity EPA supplement (4 grams of EPA as the ethyl ester) or a placebo and followed for an average of 4.9 years.
Do Omega-3s Reduce The Risk Of Heart Disease?
 The VITAL Study: The primary end point for this study was something called “major cardiovascular events”, which was a composite every cardiovascular end point measured in the study. For this end point the results were negative. Omega-3 supplementation did not cause a significant decrease in major cardiovascular events compared to the placebo.
The VITAL Study: The primary end point for this study was something called “major cardiovascular events”, which was a composite every cardiovascular end point measured in the study. For this end point the results were negative. Omega-3 supplementation did not cause a significant decrease in major cardiovascular events compared to the placebo.
This was the result that was reported in the abstract and was what lazy journalists, who never read past the abstract, reported.
However, the rest of the study was very positive. For example, major cardiovascular events were reduced by:
- 26% in African-Americans.
- 26% in patients with diabetes.
- 17% in patients with a family history of heart disease.
- 19% in patients with two or more risk factors for heart disease.
- 19% in patients with low fish intake.
In other words, omega-3 supplementation caused a significant decrease in heart disease risk for high risk patients and for patients with a poor diet (low intake of omega-3s).
In addition, several individual cardiovascular events were significantly reduced by omega-3 supplementation. For example:
- Heart attacks were reduced by 28% in the general population and by 70% for African-Americans.
- Death from heart attacks was reduced by 50%.
- Total coronary heart disease was reduced by 17%.
- Death from coronary heart disease was reduced by 24%.
In short, headlines saying that omega-3 supplementation can decrease heart attack risk appear to be accurate. Saying that eating more fish can reduce heart attack risk is stretching it a bit. The study was not done with fish, and you would need to eat 2-4 servings of omega-3-rich fish a week to get an equivalent amount of omega-3s. That’s a lot of fish.
The authors attributed the positive results obtained in this study compared to the negative results obtained in several recent studies to four factors:
- Many of the previous studies had fewer participants, used lower doses of omega-3s, and were shorter. There may not have been enough statistical power to demonstrate a benefit of omega-3s in those studies.
- Participants in many of the previous studies were on multiple medications that mimicked the beneficial effects of omega-3s, making it more difficult to show a positive effect of omega-3 supplementation.
- Most of the previous studies either did not measure the omega-3 status of participants or had a study population that started the study with near optimal omega-3 status. The VITAL study showed that omega-3s had a stronger beneficial effect for people who seldom ate fish.
- African-Americans were underrepresented in most previous studies. The VITAL study showed that omega-3s were more beneficial for African-Americans than for other ethnic groups.
As for side effects, there was no increased risk of bleeding or any other serious side effect from omega-3 supplementation.
The REDUCE-IT Study: This study of high-risk patients was even more positive than the VITAL study.
- The composite of all cardiovascular end points was reduced by 25%.
- The risk reduction was greatest for men, non-whites, and people over 65.
- The risk reduction was also greatest for people with pre-existing heart disease, very high triglyceride levels, and people who required high-dose statin therapy to keep their cholesterol under control.
In other words, everyone benefited from omega-3 supplementation in this study because they were all at high risk, but those at the highest risk benefitted the most.
When they looked at individual cardiovascular events:
- Fatal and non-fatal heart attacks were reduced by 31%.
- Cardiovascular death was reduced by 20% and death from any cause was reduced by 23%.
- Fatal and non-fatal stroke was reduced by 28%.
- Hospitalization for unstable angina was reduce by 32%.
However, this very high dose of EPA was not completely without risk:
- 1% of patients in the EPA group were hospitalized for atrial fibrillation versus 2.1% in the placebo group.
- 7% of patients in the EPA group experienced a serious bleeding event compared to 2.1% in the placebo group.
Do Omega-3s Reduce The Risk Of Cancer?
 The VITAL Study: The VITAL study also looked at the effect of omega-3s on cancer risk. The results from this study were uniformly negative. There was no effect of omega-3 supplementation on invasive cancer of any type, breast cancer, prostate cancer, colon cancer, or death from cancer. Does that mean omega-3s have no role in reducing cancer risk? That’s not clear.
The VITAL Study: The VITAL study also looked at the effect of omega-3s on cancer risk. The results from this study were uniformly negative. There was no effect of omega-3 supplementation on invasive cancer of any type, breast cancer, prostate cancer, colon cancer, or death from cancer. Does that mean omega-3s have no role in reducing cancer risk? That’s not clear.
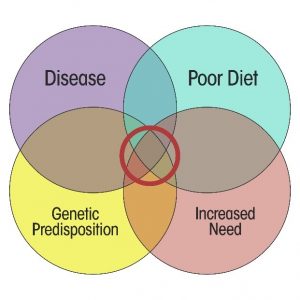
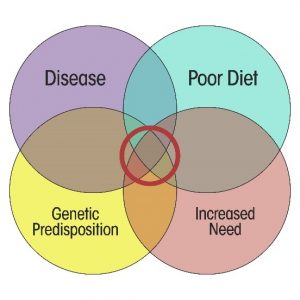
If we look at previous animal studies and human association studies, reduced cancer risk is seen when omega-3s replaced saturated fats, trans fats, and/or omega-6 fats in the diet. The subjects in the VITAL study ate a typical American diet, and the study made no effort to change what they were eating. It just added an omega-3 supplement. There is relatively little evidence that you can eat burgers and fries and expect omega-3s to reduce cancer risk.
The VITAL study merely confirms what previous studies have suggested. You can’t continue to eat a typical American diet and expect omega-3s to make cancer go away. Omega-3s should be thought of as part of a holistic approach to reducing cancer risk. If they have any role in reducing cancer risk, it is likely to be as part of a primarily plant-based diet that substitutes omega-3s for the bad fats in the American diet.
For example, the Mediterranean diet is primarily plant-based and is rich in healthy oils like olive oil and omega-3s. It is associated with reduced risk of several cancers, especially cancers of the breast and colon.
Are Omega-3 Supplements Good For You?
 There is a lot of confusion around the question of whether omega-3s are good for the heart. Some studies say yes. Others say no. If you average all the studies together, as some recent meta-analyses have done, it is easy to throw up your hands and conclude there is no definitive evidence that omega-3s reduce heart disease risk. However, if you look at why the studies differ a clear pattern emerges.
There is a lot of confusion around the question of whether omega-3s are good for the heart. Some studies say yes. Others say no. If you average all the studies together, as some recent meta-analyses have done, it is easy to throw up your hands and conclude there is no definitive evidence that omega-3s reduce heart disease risk. However, if you look at why the studies differ a clear pattern emerges.
- If the study subjects are on multiple heart medications that duplicate the beneficial effects of omega-3s, the studies tend to be negative. If the subjects are only on one or two medications, the studies tend to be positive. Since most people I know would prefer to minimize the number of medications they are on, the negative studies with multiple medications are simply not relevant to them.
- If the study subjects are at low risk of heart disease, the studies tend to be negative. If the subjects are at high risk, the studies tend to be positive. This does not mean that omega-3s are of no benefit if you are at low risk of heart disease. It simply reflects the fact it is easier to show a beneficial effect of any intervention when you have a pool of high-risk patients who are likely to experience some sort of cardiovascular event during the time-period of the study.
For example, as discussed in my recent book, “Slaying The Supplement Myths,” this the same pattern you see with statin clinical studies. If patients are at high risk, statin drugs clearly save lives. If they are at low risk, it is almost impossible to show any benefit of statin drugs. Cardiologists extrapolate from the high-risk studies and prescribe statins to low-risk patients. I think it is time to take a similar approach with omega-3s.
- If the subjects have a good omega-3 status at the beginning of the study, additional omega-3 supplementation usually has no benefit. If their omega-3 status is poor at the beginning of the study, the results of omega-3 supplementation tend to be positive. This is just common sense. Supplementation is meant to fill gaps in the diet – not to provide a surplus of nutrients. Of course, the reality is many Americans do not get enough omega-3s in their diet.
What Do These Studies Mean For You?
 Omega-3s Are Good For Your Heart: When you combine the latest studies with what we already know about omega-3s and heart disease, the results are clear-cut.
Omega-3s Are Good For Your Heart: When you combine the latest studies with what we already know about omega-3s and heart disease, the results are clear-cut.
- If you are at high risk of heart disease, don’t eat many omega-3-rich fish, and/or don’t want to be on a handful of heart medications, the evidence is strong that omega-3s reduce your risk of heart disease.
- On the other hand, if you are at low risk of heart disease, eat 2-4 servings of omega-3-rich fish a week, and/or are happy taking multiple heart medications with all their side effects, it is difficult to prove that omega-3s have any benefits. That doesn’t mean that omega-3s don’t have benefits. It just means we can’t prove they do.
If you are still having trouble making up your mind whether omega-3 supplements are the right choice for you, I might remind you:
- If you are like millions of Americans, the first sign you are at risk of heart disease might be sudden death.
- If you are like most Americans, you are probably not getting enough omega-3s in your diet.
- If you prefer taking drugs, you are probably not interested in supplements anyway.
Holistic Is Best: When you combine the VITAL study results with what we already know about omega-3s and cancer, it appears that adding omega-3s to a bad diet is unlikely to reduce your risk of cancer. However, a holistic approach that starts with a healthy, primarily plant-based diet and substitutes omega-3s for the bad fats in the American diet is likely to substantially reduce your cancer risk. The Mediterranean diet might be considered an example of that approach.
The same is likely true for heart health. While the latest two studies suggest that adding omega-3 supplements to your regular diet reduces your heart disease risk, those omega-3 supplements are likely to be even more effective if you also adopt a heart-healthy diet and lifestyle.
Omega-3 Supplements vs Omega-3 Drugs: The Omega-3 preparations used in this study are pharmaceutical-grade omega-3 preparations and are marketed as drugs. Thus, it is likely that many doctors will recommend them rather than less expensive omega-3 supplements. Which choice is best for you?
The preparation used in the VITAL study is similar in composition to many commercially available omega-3 supplements. The main difference is that it is high purity and is subject to the quality control standards required for pharmaceutical drugs. Many omega-3 supplements do not meet these standards, but some do. If you wish to use an omega-3 supplement, do your research. Inquire about their quality control standards and only buy high purity supplements.
The preparation used in the REDUCE-IT study used ultra-pure EPA only. That preparation did not contain any other omega-3s, so a commercially available omega-3 supplement would not be comparable. However, I do not recommend an EPA-only supplement for three reasons.
- The results for high risk patients in the REDUCE-IT study were similar to those for high risk patients in the VITAL study. This suggests that removing DHA and other omega-3s may not provide additional protection against heart disease. A head to head comparison of the two supplements would be required to prove the superiority of an EPA-only supplement.
- I have the same concern for this high-dose EPA supplement as I have for any high-dose single nutrient supplement. DHA and other omega-3s provide benefits such as cognitive health that EPA does not. Very high dose EPA is likely to interfere with the uptake and utilization of the other omega-3s.
- The EPA only supplement used in the REDUCE-IT study had side effects that were not seen with the mixed omega-3 supplement used in the VITAL study. It is not clear whether those side effects were due to differences in dose or differences in formulation.
Omega-3 Ethyl Esters vs Omega-3 Triglycerides: There has been a lot of hype about the superiority of omega-3 triglyceride preparations recently. These studies were both done with omega-3 ethyl esters and proved to be very effective. Until someone shows that omega-3 triglyceride preparations provide better results at reducing heart disease risk than omega-3 ethyl esters, I would leave omega-3 triglyceride supplements on the shelf.
How Much Omega-3s Do You Need? We have too few dose-response studies to reliably predict how much omega-3s are optimal for reducing heart disease risk. The 1 gram/day dose used in the VITAL study gave good results, so that is an excellent starting point. The 4 gram/day dose used in the REDUCE-IT study seemed to provide little additional benefit.
Of course, the optimal dose is likely to be different for each of us. Once the omega-3 index blood test becomes more widely available I would recommend getting your omega-3 index determined on an annual basis and aiming for an omega-3 index of 8 or above, since that is the level associated with a low risk of heart disease.
The Bottom Line
There is a lot of confusion around the question of whether omega-3s are good for the heart. Some studies say yes. Others say no. If you average all the studies together, as some recent meta-analyses have done, it is easy to throw up your hands and conclude there is no definitive evidence that omega-3s reduce heart disease risk.
However, two recent studies support the effectiveness of omega-3s for reducing heart disease risk. When you combine the latest studies with what we already know about omega-3s and heart disease, the results are clear-cut.
- If you are at high risk of heart disease, don’t eat many omega-3-rich fish, and/or don’t want to be on a handful of heart medications, the evidence is strong that omega-3s reduce your risk of heart disease.
- On the other hand, if you are at low risk of heart disease, eat 2-4 servings of omega-3-rich fish a week, and/or are happy taking multiple heart medications with all their side effects, it is difficult to prove that omega-3s have any benefits. That doesn’t mean that omega-3s don’t have benefits. It just means we can’t prove they do.
If you are still having trouble making up your mind whether omega-3 supplements are the right choice for you, I might remind you:
- If you are like millions of Americans, the first sign you are at risk of heart disease might be sudden death.
- If you are like most Americans, you are probably not getting enough omega-3s in your diet.
- If you prefer taking drugs, you are probably not interested in supplements anyway.
In addition, one of the studies confirmed what we already know about omega-3s and cancer. Adding omega-3s to a bad diet is unlikely to reduce your risk of cancer. However, a holistic approach that starts with a healthy, primarily plant-based diet and substitutes omega-3s for the bad fats in the American diet is likely to substantially reduce your cancer risk. The Mediterranean diet might be considered an example of that approach.
The same is likely true for heart health. While the latest two studies suggest that adding omega-3 supplements to your regular diet reduces your heart disease risk, those omega-3 supplements are likely to be even more effective if you also adopt a heart-healthy diet and lifestyle.
For more details read the article above. In addition, the article covers topics like omega-3 supplements versus omega-3 drugs, omega-3 ethyl esters versus omega-3 triglycerides, and how much omega-3s we need. It also discusses why several recent studies have failed to find a benefit of omega-3s for reducing heart disease risk.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.