Are Supplements The Fountain Of Youth?
Author: Dr. Stephen Chaney
 It is buyer beware in the supplement industry. I have discussed the dark side of the supplement industry in the first half of my book “Slaying The Supplement Myths.”
It is buyer beware in the supplement industry. I have discussed the dark side of the supplement industry in the first half of my book “Slaying The Supplement Myths.”
I called that section of my book “The Lies of the Charlatans.” In it, I detailed many of the false claims that some manufacturers make for their supplements. There are claims that their supplements will…
- Cure what ails you (Just fill in the disease of your choice. Some company will try to tell you they have the cure).
- Make the pounds melt away.
- Make you smarter.
- Make you stronger.
- Improve your sex life.
Can supplements help you live longer?
The list seems endless…Except for one! I don’t know of any supplement company claiming their supplements make you live longer. Nobody is claiming their supplements are the “Fountain of Youth.”
However, many of you have been asking me about headlines claiming that a recent study showed that supplements don’t extend lives. Could it be that the study generating the recent headlines was designed to disprove a claim nobody was making?
In this issue of “Health Tips From The Professor” I will analyze the study and answer two questions:
- Is it true?
- Is it important?
How Was The Study Done?
 Every few years the National Center for Health Statistics (a division of the CDC) conducts a massive survey of factors affecting the health of the American population. This survey is called the National Health and Nutrition Examination Survey (NHANES). The NHANES survey includes interviews and examinations of thousands of people across the country.
Every few years the National Center for Health Statistics (a division of the CDC) conducts a massive survey of factors affecting the health of the American population. This survey is called the National Health and Nutrition Examination Survey (NHANES). The NHANES survey includes interviews and examinations of thousands of people across the country.
The interview includes dietary, health-related, demographic, and socioeconomic questions. The examination component includes laboratory tests plus medical, dental, and physiological measurements. The NHANES database is used for many studies such as this one.
The current study (F Chen et al, Annals of Internal Medicine, doi:10.7326/M18-2478, published April 9, 2019) used data from 30,899 US adults aged 20 years or more who participated in 6 cycles of the NHANES survey from 1999 to 2010. The dietary portion of the survey taken by these participants contained questions on the dietary supplements they had used in the 30 days prior to the survey.
The NHANES data were linked to the National Death Index mortality data so that the effect of nutrient intake and supplement use on mortality could be assessed. The median follow-up for the participants in the study was 6.1 years. During that time, 3613 deaths occurred, 945 from heart disease and 805 from cancer.
Of the participants:
- 71% were white, 11% were non-Hispanic black, and 13% were Hispanic.
- 9% were female, 49.1% were male.
- 2 % of the participants reported supplement use in the 30 days preceding the survey.
- Among the supplement users, the major supplements reported were:
- Multivitamin/multimineral (74.8%).
- Vitamin C (40.3%).
- Calcium (38.6%).
- Vitamin D (37.6%).
- Zinc (34.5%).
- Magnesium (33.3%).
When they compared supplement users with non-supplement users, the supplement users were:
- More likely to be female and non-Hispanic white.
- Have higher levels of family education and income.
- Eat a healthier diet and be more physically active.
- Less likely to be current smokers, heavy drinkers, or obese.
These are all factors that favor a longer lifespan. However, the supplement users were also:
- Older (average age = 50.7 versus 42.8 for non-supplement users).
- Sicker (They were more likely to have cancer, heart disease, diabetes, high blood pressure, and high cholesterol levels).
These are factors that favor a shorter lifespan.
These are what statisticians refer to as confounding variables. They can influence the results of a study in unexpected ways.
Can Supplements Help You Live Longer?
 When they looked at the raw data, supplemental use of most-individual nutrients was associated with a lower risk for all-cause death. In simple terms, supplementation appeared to increase lifespan.
When they looked at the raw data, supplemental use of most-individual nutrients was associated with a lower risk for all-cause death. In simple terms, supplementation appeared to increase lifespan.
However, when the data were statistically adjusted for all of the confounding variables (age, sex, race/ethnicity, education, physical activity, smoking, alcohol intake, diet quality, BMI [a measure of obesity], and diseases the participants had when they entered the study), the effect of supplementation on lifespan became non-significant.
The authors concluded: “Use of dietary supplements was not associated with mortality benefits among a nationally representative sample of U.S adults.” Those are the headlines you saw from your favorite news source.
What Does This Study Mean For You?
Let’s go back to the two questions I posed about the study at the beginning of this article.
 Is it true? Can supplements help you live longer? The study had many weaknesses, which the authors identified in their discussion. Of course, the people writing the headlines never bothered to read the paper, so they were unaware of its weaknesses. Here are some of the major weaknesses reported by the authors:
Is it true? Can supplements help you live longer? The study had many weaknesses, which the authors identified in their discussion. Of course, the people writing the headlines never bothered to read the paper, so they were unaware of its weaknesses. Here are some of the major weaknesses reported by the authors:- The NHANES questionnaire only asked about supplement use over the preceding 30 days. We have no idea how long the participants had been using those supplements. It could have been years, or it could have been a month. In the words of the authors: “Dietary supplement use was assessed in the previous 30 days, which may not reflect habitual use or capture changes in use [before or] after the baseline assessment.”
- The supplement users were more likely to have been diagnosed with health conditions such as cancer, heart disease, diabetes, and high blood pressure. It is well documented that diagnosed health conditions motivate some people to initiate supplement use.
- Finally, there were multiple confounding variables in this study. The conclusion of the study rested on a statistical adjustment of the data to correct for those confounding variables. In the words of the authors: “Residual confounding may still be present.”
That last point reminds me of the famous Mark Twain quote: “There are lies. There are damn lies. And then there are statistics.” Don’t misunderstand me. I am not accusing the study authors of lying. They are some of the top scientists in the field. What Mark Twain and I are saying is that when you rely on statistics, sometimes bad things happen. You can come to erroneous conclusions.
- Is it important? Even if the conclusion of this study is true, we should ask if it is important. If there had been widespread claims that supplements make you live longer, this would be an important finding. However, nobody I know is making that claim. This study simply reaffirms what most people assumed anyway. There is no fountain of youth.
 By the way, the situation is similar for diets. There have been a few claims in the past that healthy diets will help you live longer. However, when those claims have been rigorously evaluated, there is very little effect of diet on lifespan. There have been some studies that have reported a decrease in premature death due to heart disease or cancer. However, death from all causes usually remains unchanged. Once again, the fountain of youth has eluded us.
By the way, the situation is similar for diets. There have been a few claims in the past that healthy diets will help you live longer. However, when those claims have been rigorously evaluated, there is very little effect of diet on lifespan. There have been some studies that have reported a decrease in premature death due to heart disease or cancer. However, death from all causes usually remains unchanged. Once again, the fountain of youth has eluded us.
You may be asking, if supplements don’t increase lifespan, what good are they? The answer is simple. They increase healthspan. Simply put, that means you spend a greater portion of your lifespan in good health.
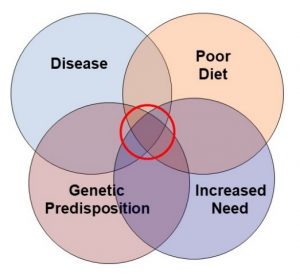
Of course, now you are probably really confused. You’ve read all those headlines saying that supplements don’t have any effect on your health. The problem is that the studies generating those headlines are flawed. They aren’t asking the right questions. When you look at populations with poor diets, increased needs, genetic predisposition, and/or pre-existing disease, supplementation is often beneficial. I cover this in the second half of my book, “Slaying the Supplement Myths.” That section is called “The Myths Of The Naysayers.”
The Bottom Line
A recent study reported that supplements do not reduce mortality. They won’t make you live longer. In this article I provide a detailed analysis of that article. The two important take-aways are:
- There are several weaknesses in the study. The conclusion may not be accurate.
- Even if it is accurate, it may not be important. If there had been widespread claims that supplements make you live longer, this would be an important finding. However, nobody I know is making that claim. This study simply reaffirms what most people assumed anyway. There is no fountain of youth. Could it be that the study generating the recent headlines was designed to disprove a claim nobody was making?
The real benefit of supplementation isn’t in increasing your lifespan. It is increasing your healthspan. I cover that in my book, “Slaying The Supplement Myths.”
For more details read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.