How To Lose Weight And Keep It Off
 Tomorrow is the official start of another dieting season. Millions of Americans will be making a New Year’s Resolution to lose weight. The top three reasons for these weight loss resolutions are:
Tomorrow is the official start of another dieting season. Millions of Americans will be making a New Year’s Resolution to lose weight. The top three reasons for these weight loss resolutions are:
1) Reduce disease risk (73%). After all, we are being told those excess pounds increase our risk of diabetes, heart disease, cancer, and just about every other disease known to man.
2) Improve self-esteem (61%). Some of this may be due to the social stigma associated with obesity, but many people simply want to improve the image they see in the mirror every morning when they get out of the shower.
3) Boost energy (49%).
Those are all good reasons for losing weight. But before you make your New Year’s resolution to embark on another weight loss journey, you should ask yourself “Do weight loss diets work?” If you look at the statistics, they aren’t very encouraging:
1) 45 million Americans go on a weight loss diet every year.
· 50% go on fad diets.
· They spend $33 billion on weight loss products.
· 90% regain almost all the weight. That’s called the yo-yo effect.
· On average, Americans gain 11 pounds on every diet yo-yo.
o They might as well have thrown that $33 billion to the wind.
2) 228,000 Americans get gastric bypass surgery.
· 80% regain almost all the weight.
o Their digestion and their health will never be the same.
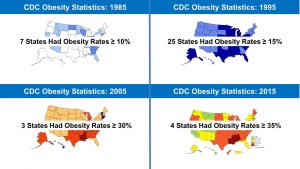
As if those statistics weren’t bad enough, the obesity epidemic gets worse year after year (see the graphic on the 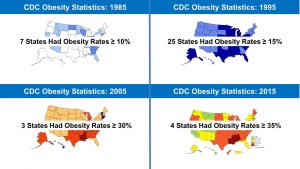 right). Americans keep getting fatter. What we are doing clearly isn’t working.
right). Americans keep getting fatter. What we are doing clearly isn’t working.
You are probably saying to yourself: “I know that, but this year I’m going to try a new diet.” As the saying goes “Hope springs eternal in the human breast”, but is it realistic to think this time will be different?
Let me share a quote from a book and TV series called “The Weight Of the Nation” by John Hoffman & Dr. Judith Salerno”:
“First we blamed fat – low fat diets didn’t work! Then we blamed carbs, eggs, red meat, dairy, white flour, sugar, juices, sodas, high-fructose corn syrup, & partially hydrogenated fats. One by one, we replaced the evil food du jour…and watched our collective waistlines grow.”
In other words, they are saying it’s not just low-fat diets that don’t work. None of the popular diets work long term. I come across lots of people who tell me the Atkins weight-loss diet works best for them. That would be convincing if they were slender, but they aren’t! They gained it all back and then some. Now that the keto diet has been around for a few years, I am starting to see the same pattern there as well.
Clearly, the problem isn’t losing the weight. Any diet can help you lose weight. The problem is keeping the weight off. Let’s look at why this is.
Why Do Most Diets Fail?
 To understand the answer to this question, let’s start with another quote from “The Weight Of the Nation”: “Our bodies were designed to store fat in times of plenty and retain fat in times of famine”
To understand the answer to this question, let’s start with another quote from “The Weight Of the Nation”: “Our bodies were designed to store fat in times of plenty and retain fat in times of famine”
Essentially, the authors were saying when our ancestors were hunters and gatherers, there were times when food was abundant, and times when food was scarce. In order to survive, our bodies had to store energy in its most efficient form when food was abundant and hold on to those energy stores as long as possible when food was scarce.
Fat provides more than twice as many calories per gram as either carbohydrate or protein. Additionally, our ability to store carbohydrate is limited. And we don’t really have protein stores. All the proteins in our body have essential functions. However, our ability to store fat is unlimited. Now you understand why fat is the preferred energy store in times of plenty and our bodies try to hold on to it as long as possible in times of famine.
With that perspective in mind, there are three reasons why most diets fail:
1) Most dieters are looking for rapid weight loss (at least 2-5 pounds/week). That is a problem because “Our bodies were designed to…retain fat in times of famine”. When we lose weight quickly, our bodies interpret that as famine. Our bodies respond by decreasing our metabolic rate so we can hold on to those fat stores.
The solution to this problem is to set more reasonable weight loss goals. If we keep the rate of weight loss in the 1-2 pound/week range (0.5-1 pounds/week is even better), we can largely avoid this famine response. You should ask yourself, “What’s the rush?” After all, the average American only gains 1-2 pounds/year. Why do we need to get rid of that excess weight in just a few weeks?
2) Most dieters are looking for significant weight loss (more than 20 pounds). That is a problem because our bodies are designed to retain fat stores, not protein stores. When our bodies sense a famine they burn our protein stores (lean muscle mass) to spare as much of our fat stores as possible. The longer the diet (famine) lasts, the more muscle mass we lose.
That’s a problem because muscle burns calories much faster than fat. The more muscle we lose, the more our metabolic rate decreases. It gets harder and harder to lose weight, and eventually we reach a plateau. Most people get discouraged at that point and go off their diet.
That’s where the other part of the quote from “The Weight Of The Nation” kicks in: “Our bodies are  designed to store fat in times of plenty”. Once again, it is fat we store, not protein. Most people never regain the protein stores they lost, so their metabolic rate remains low. They regain most of the weight they lost, and then some. This is the origin of the yo-yo effect.
designed to store fat in times of plenty”. Once again, it is fat we store, not protein. Most people never regain the protein stores they lost, so their metabolic rate remains low. They regain most of the weight they lost, and then some. This is the origin of the yo-yo effect.
There are two solutions to this problem:
· Increase your resistance exercise and your intake of protein with high levels of the essential amino acid leucine. I have covered this in a previous issue of “Health Tips From The Professor”.
· Set more reasonable weight loss goals. It is possible to lose more than 20 pounds without losing muscle mass. We just need to think in terms of reaching those weight loss goals in years rather than in months. Once again, remember it took us years to gain the weight. Why not think in terms of years to lose the weight?
3) Most dieters think in terms of diets rather than lifestyle change. Diets have an expiration date. Then most people just drift back to “the way they really live”. Lifestyle change, on the other hand, is permanent. Once we change to a healthier lifestyle, we no longer need to focus on weight loss. The weight comes off automatically.
To better understand the power of lifestyle change let’s look at something called “The National Weight Control Registry”.
How To Lose Weight And Keep It Off
 Rather than focus on the abysmal statistics for long-term weight loss, doctors Rena Hill and James O Wing decided to focus on the characteristic of people who manage to keep their weight off. They founded something called “The National Weight Control Registry” and invited people who were successful at keeping the weight off to participate in their program.
Rather than focus on the abysmal statistics for long-term weight loss, doctors Rena Hill and James O Wing decided to focus on the characteristic of people who manage to keep their weight off. They founded something called “The National Weight Control Registry” and invited people who were successful at keeping the weight off to participate in their program.
Currently, the National Weight Control Registry is tracking over 10,000 individuals who have lost 30 pounds or more and have kept it off for long periods of time. They use detailed questionnaires and annual follow-up surveys to study the behavioral and psychological characteristics and the strategies of weight loss maintainers.
When you look at how they lost weight, they are a very diverse group:
· They lost weight on every possible diet – from vegan to keto to just plain crazy.
· 50% lost weight on commercial diet programs. 50% lost weight on their own.
· Some lost weight quickly. Some lost weight slowly.
When you look at weight maintenance, you realize that the dismal weight maintenance statistics don’t have to apply to you. The good news is:
· On average, people in The National Weight Control Registry have lost 66 pounds and have kept it off for 5 years or more.
· 12-14% of them have maintained a weight loss of 100 pounds or more for 5 or more years.
· Even better, once they maintained their weight loss for 2-5 years, it became easy.
They no longer had to battle hunger and a sluggish metabolism. They no longer had to think about the lifestyle changes they were trying to maintain. Their new lifestyle became what they did automatically, without even thinking about it. Their weight loss had become permanent.
By now, you are probably wondering how they do it. Here are the top 7 characteristics of those who are successful at keeping the weight off:
at keeping the weight off:
1) They consumed reduced calorie, low-fat, healthy diets.
2) They had internalized their eating patterns. It had become how they ate every day without even thinking about it.
3) They monitored their weight regularly. This allowed them to make adjustments whenever they saw their weight start to creep up.
4) They ate breakfast on a regular basis.
5) They got lots of exercise (on average, about 1 hour/day).
6) They watched less than 10 hours of TV/week. If you were wondering where you would find the time to exercise an hour/day, this is probably your answer.
7) They were consistent. They had no planned “cheat days”. This doesn’t mean they were purists. They still allowed themselves to eat some of their favorite unhealthy foods on an occasional basis. They just didn’t set aside regular times when they planned to “pig out”.
There was one other interesting observation from this study:
· Those who used meal replacement shakes as part of their weight loss, focused more on diet and included meal replacement shakes as part of their maintenance program.
· Those who lost weight on their own, also followed healthy eating habits, but put a bit more emphasis on exercise to keep themselves on track.
· Both approaches were effective.
The take-home message of the National Weight Control Registry is clear. There is no magic diet that guarantees you will keep the weight off. The “secret” to keeping the weight off is a healthy eating pattern and a healthy lifestyle.
In short, if your resolution is to lose weight next year, don’t focus on the diet you will follow to lose the weight. Instead, focus on the healthy lifestyle you will follow to keep the weight off.
Of course, you will be most successful if the diet you are following to lose weight incorporates the healthy lifestyle you plan to follow to maintain your weight loss.
What Role Do Habits Play In Weight Loss?
 Finally, I would like to share a recent study (G Cleo et al, International Journal of Obesity, 43: 374-383, 2019) that puts the whole issue of weight loss and weight maintenance in a different perspective. This study looked at the role that habits play in weight loss.
Finally, I would like to share a recent study (G Cleo et al, International Journal of Obesity, 43: 374-383, 2019) that puts the whole issue of weight loss and weight maintenance in a different perspective. This study looked at the role that habits play in weight loss.
In short, the study enrolled 130 participants who wanted to lose weight. All the participants were told this was a weight loss study, but none of the participants were given detailed diet and exercise recommendations to follow. The study had a 12-week intervention phase followed by a 12-month follow-up phase. The participants were divided into three groups.
1) Group 1 received no advice during the intervention phase. This was the control group.
2) Group 2 focused on breaking old habits. During the intervention phase they were sent daily tests suggesting new habit patterns. These were suggestions like “Drive a different route to work today”. None of the texts had anything to do with diet or lifestyle.
3) Group 3 focused on creating new healthy habits. They were given a list of 10 healthy habits. During the intervention phase they were asked to log how many of these habits they implemented each day. The 10 healthy habits were:
#1: Keep to a daily meal routine.
#2: Choose reduced fat versions of foods.
#3: Walk off the weight (aim for 10,000 steps/day).
#4: Pack a healthy snack (Choose healthy options such as fruits, nuts, or low-fat yogurt).
#5: Read labels.
#6: Be cautious with your portions.
#7: Break up your sitting time (Stand for 10 minutes every hour).
#8: Think about your drinks (Choose water instead of sodas and fruit juices).
#9: Focus on your food (Slow down. Don’t eat while watching TV).
#10: Don’t forget your 5 servings of fruits and vegetables a day.
The results were:
· People in both habit change groups lost significantly more weight than people in the control group.
· People in the habit change groups continued to lose weight for 12 months after the intervention ended.
· Weight loss was essentially identical in the two habit change groups.
The last observation is particularly interesting. Remember that one of the habit change groups was simply focused on breaking old habits, yet people in this group did just as well as people who were taught healthy lifestyle habits. This implies that people already know about healthy lifestyle habits. They just don’t know how to break their old habits. Once they become comfortable breaking old habits, they find it easy to adopt healthier lifestyle habits.
In short, change your habits, change your lifestyle. Change your lifestyle, control your weight.
What Does This Mean For You?
 I covered a lot of information in this article. Let me sum it up by giving you my top 10 tips for losing weight and keeping it off.
I covered a lot of information in this article. Let me sum it up by giving you my top 10 tips for losing weight and keeping it off.
1) You don’t need to achieve your “ideal weight”. Losing 5-10% of your body weight may be enough.
2) Ditch diets. Focus on lifestyle change.
3) Slow and steady wins the day.
4) Change your habits, change your weight.
5) Long-term weight loss is possible.
6) Low-fat, healthy eating patterns are best.
7) Once you have internalized healthy habits, they become automatic.
8) If you stick with a healthy lifestyle long enough, keeping the weight off becomes easy.
9) Focus on all the healthy food choices you have, not what you have to give up. There is a cornucopia of great tasting, healthy foods to choose from.
10) Never say never. Allow yourself to enjoy your old favorite foods on occasion. Just don’t make it a habit.
The Bottom Line
I cover a lot of information in this article. Let me sum it up by giving you my top 10 tips for losing weight and keeping it off.
1) You don’t need to achieve your “ideal weight”. Losing 5-10% of your body weight may be enough.
2) Ditch diets. Focus on lifestyle change.
3) Slow and steady wins the day.
4) Change your habits, change your weight.
5) Long-term weight loss is possible.
6) Low-fat, healthy eating patterns are best.
7) Once you have internalized healthy habits, they become automatic.
8) If you stick with a healthy lifestyle long enough, keeping the weight off becomes easy.
9) Focus on all the healthy food choices you have, not what you have to give up. There is a cornucopia of great tasting, healthy foods to choose from.
10) Never say never. Allow yourself to enjoy your old favorite foods on occasion. Just don’t make it a habit.
For more details on how to lose weight and keep it off, read the article above. In fact, if you plan to lose weight in the coming year, you should really read this article first.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
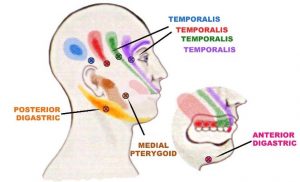
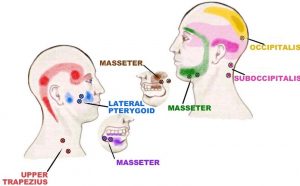
 Each of the spasms noted in these two charts can be treated by applying direct pressure onto the spasm and then holding it for 15-30 seconds. Use as much pressure as you can, but it must always be in the tolerable range, this is NOT a “no pain-no gain” situation. It is going to hurt because you are forcing toxins out of the muscle fibers, and the toxin is an acid (from lactic acid) so it burns. However, you’ll find that as you continue holding the pressure it will lessen.
Each of the spasms noted in these two charts can be treated by applying direct pressure onto the spasm and then holding it for 15-30 seconds. Use as much pressure as you can, but it must always be in the tolerable range, this is NOT a “no pain-no gain” situation. It is going to hurt because you are forcing toxins out of the muscle fibers, and the toxin is an acid (from lactic acid) so it burns. However, you’ll find that as you continue holding the pressure it will lessen.