How Does DNA Testing Work Best?
 Genomics (DNA testing) is hot. You are being told that if you just knew your genes, you could lose weight successfully, be healthier, be happier, leap tall buildings in a single bound (Actually, I haven’t heard the last claim, but it’s about the only claim that genomics marketers haven’t made). Which of these claims are true, and which are just hot air?
Genomics (DNA testing) is hot. You are being told that if you just knew your genes, you could lose weight successfully, be healthier, be happier, leap tall buildings in a single bound (Actually, I haven’t heard the last claim, but it’s about the only claim that genomics marketers haven’t made). Which of these claims are true, and which are just hot air?
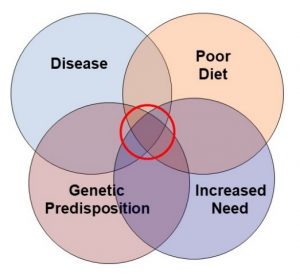
The experts agree that the benefits of DNA testing have been greatly oversold. As I said in a recent article on DNA testing, the idea that genes control our destiny is no longer considered valid. There are 3 reasons for this. I will start with the scientific term for each and then give you the non-scientific explanation.
- Penetrance simply means that the severity of most gene mutations is influenced by our genetic background. Simply put, the same mutation can have a significant effect in one individual and a trivial effect in another individual.
- Epigenetics refers to modifications of the DNA that influence gene expression. These DNA modifications are, in turn, influenced by diet and lifestyle.
- Microbiome refers our gut bacteria. In many cases, our microbiome has just as much influence on our health as our genes. And our microbiome is influenced by diet and lifestyle.
Now you know the complexity of DNA testing, it is easy to see why experts feel that it is premature to use DNA testing to predict the best diet for either weight loss or health.
As an example, one recent study used DNA testing to predict whether study participants were more likely to lose weight on a low-carb or low-fat diet. The participants were then randomly assigned to low-carb and low-fat diets. At the end of 12 months:
- There was no significant difference in weight loss for those on low-fat and low-carb diets. This has been reported in multiple previous studies but is an inconvenient truth that most low-carb enthusiasts tend to ignore.
- DNA testing offered no predictive value as to whether a low-carb or low-fat diet was more effective for weight loss.
However, DNA testing may have one benefit that is overlooked by many experts. What if the DNA test results motivated people to do better? After all, most diet advice is generic. People feel it may or may not apply to them. Does personalized diet advice based on their genetic makeup motivate people to stick with the diet better?
Some studies have suggested that people may follow personalized diet plans based on their DNA more faithfully. However, most of those studies have been short-term.
That is why I have chosen today’s study (J Horne et al, BMJ Nutrition, Prevention & Health, 2020) to discuss. It is a very well-designed study and it lasted for a full year.
How Was The Study Done?
 This was an extremely well-designed study. In fact, it was so well designed that it probably needs the “Results are not typical” designation the FDA requires when some diet companies make claims about weight loss success. Here are the details:
This was an extremely well-designed study. In fact, it was so well designed that it probably needs the “Results are not typical” designation the FDA requires when some diet companies make claims about weight loss success. Here are the details:
- The study participants were highly motivated, college educated, middle-aged (average age = 55), obese (average weight = 216 pounds) Caucasian women who had a positive attitude about their ability to change what they ate. In case you weren’t counting, there were four characteristics of this group that might be considered atypical for the average American.
- The participants volunteered for a highly structured weight loss program called the “Group Lifestyle Balance”, or GLB, program.
-
- Participants were given a detailed calorie-controlled nutrition plan at the beginning of the program.
-
- They were asked to track their daily food and beverage intake for the first 2-3 months of the program.
-
- In the second week of the program participants were educated on how to count and track calories and nutrients such as total fat or saturated fat.
-
- There were weekly meetings with dietitians the first 3 months and monthly meetings for the remainder of the 12-week program to provide the guidance and support needed to stick with their nutrition plan.
- The plan also incorporated a behavior change program called Theory of Planned Behavior (TPB) that evaluates and influences attitudes, subjective norms, and behavioral control that are key to behavior change. During the regular meetings:
-
- The participants were informed about of the health benefits associated with a healthy lifestyle.
-
- They were educated on positive mindsets and mindfulness.
-
- They were taken through a stepwise, goal setting approach designed to positively impact behavioral change.
In short, this is a gold standard diet program that provided the nutritional support needed to stick with the diet program and the psychological support needed to change eating behavior. Unfortunately, this is also atypical. Very few diet programs provide this level of support.
Everyone in the study participated in this program. However, the participants were divided into two groups.
- Both groups were advised to follow a standard calorie-controlled, moderately low-fat (25% of total calories) nutrition plan.
- In addition, the second group was put on a plan that was either high protein or low saturated fat (<10% of total calories) based on their DNA test results.
- The nutritional support was identical except that the second group was told that their nutrition plan was specific for them, based on their DNA analysis.
- The dietary intake of both groups was assessed with a 3-day dietary recall (2 week days and 1 weekend day) at baseline (before the program began) and at 3, 6, and 12 months to assess the participants adherence to their diet plan.
Can DNA Testing Help You Lose Weight?
 I hate to disappoint you, but the short answer to this question, is no. Both groups lost the same amount of weight, which is not surprising considering the comprehensive nature of the diet program that both groups were enrolled in.
I hate to disappoint you, but the short answer to this question, is no. Both groups lost the same amount of weight, which is not surprising considering the comprehensive nature of the diet program that both groups were enrolled in.
However, the group given advice based on their DNA test were more motivated to stick with their personalized nutrition goals. Specifically:
- Long-term adherence to reductions in saturated fat intake was significantly greater in the group that was told their diet plan was personalized based on their DNA analysis.
-
- The control group reduced their saturated fat intake by 12% at 3 months, but only by 4% at 6 months, and 2.5% at 12 months.
-
- The group with the personalized diet plan reduced their saturated fat intake by 14% at 3 months, 18% at 6 months, and 22% at 12 months.
- Long-term adherence to reductions in total fat intake was also significantly greater in the group that was told their diet plan was personalized based on their DNA analysis.
-
- The control group reduced their total fat intake by 18% at 3 months, but only by 4% at 6 and 12 months.
-
- The group with the personalized diet plan reduced their total fat intake by 11% at 3 months, 13% at 6 months, and 16% at 12 months.
-
- It is important to remember that both groups had been advised to reduce their total fat intake to 25% of calories and had received nutritional and psychological support to achieve that goal. The only difference was that the second group had been told that advice was based on their DNA test.
The authors of the study concluded: “Weight management interventions guided by nutrigenomics can motivate long-term improvements in dietary fat intake above and beyond gold-standard population-based interventions.”
How Does DNA Testing Work Best?
 There remain significant concerns about the validity of personalized weight loss advice based on DNA testing. However, this and other studies suggest that DNA testing may provide one valuable asset for weight loss programs. It appears that people are more likely to stick with a program they believe has been personalized for them.
There remain significant concerns about the validity of personalized weight loss advice based on DNA testing. However, this and other studies suggest that DNA testing may provide one valuable asset for weight loss programs. It appears that people are more likely to stick with a program they believe has been personalized for them.
There are, however, several caveats to this conclusion.
- Participants in this study received nutritional and psychological support throughout the 12-month program. We don’t know how well participants would have stuck with the program if they had not been continually reminded that the program had been personalized for them.
- Participants in this study were well-educated, highly motivated, Caucasian women. We don’t know whether these results apply to men and to other ethnic and socioeconomic groups.
- This study only looked at personalized diet advice based on DNA testing. Some studies suggest that other methods of diet personalization may also improve adherence.
- Personalization can be misused to recommend unhealthy dietary changes. It is not enough to follow personalized diet advice. You also need to ask whether it is healthy dietary advice.
For example, DNA test results consistent with reduced carbohydrate intake are sometimes used to recommend unhealthy diets that eliminate one or more food groups rather than low-carb versions of healthy diets like the Mediterranean diet.
The Bottom Line
There remain significant concerns about the validity of personalized weight loss advice based on DNA testing. However, DNA testing may provide one valuable asset for weight loss programs. Some studies have suggested that people are more likely to stick with a program they believe has been personalized for them.
However, most of these studies have been short term. A recent study asked whether the improvement in motivation lasted for 12 months.
Two matched groups of well-educated, highly motivated women were enrolled in a “gold-standard” weight loss program that provided both nutritional and psychological support for 12 months.
Both groups were given a diet plan that restricted total calorie intake and advised reducing fat intake to 25% of total calories. However, based on their DNA test results one group was given a personalized diet plan that also advised them to reduce their saturated fat intake to less than 10% of total calories.
- The group receiving personalized diet advice did a better job of reducing both saturated and total fat intake and maintaining that change for 12 months compared to the group that just received a set diet plan.
- These results suggest that personalization of diet advice may improve long-term adherence to healthy dietary changes.
The authors of the study concluded: “Weight management interventions guided by nutrigenomics can motivate long-term improvements in dietary fat intake above and beyond gold-standard population-based interventions.”
There are, however, several caveats to this conclusion.
- Participants in this study received both nutritional and psychological support throughout the 12-month program. We don’t know how well participants would have stuck with the program if they had not been continually reminded that the program had been personalized for them.
- Participants in this study were well-educated, highly motivated, Caucasian women. We don’t know whether these results apply to men and to other ethnic and socioeconomic groups.
- This study only looked at personalized diet advice based on DNA testing. Some studies suggest that other methods of diet personalization may also improve adherence.
- Personalization can be misused to recommend unhealthy dietary changes. It is not enough to follow personalized diet advice. You also need to ask whether it is healthy dietary advice.
For more details read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.