How Can You Identify High Quality Products?
 When it comes to the food and supplement industries a paraphrase of the famous introduction to “A Tale Of Two Cities” comes to mind; “It is the best of worlds, it is the worst of worlds.”
When it comes to the food and supplement industries a paraphrase of the famous introduction to “A Tale Of Two Cities” comes to mind; “It is the best of worlds, it is the worst of worlds.”
There are companies who value your health more than their bottom line. They insist on the highest quality ingredients, verify the purity of their ingredients, and run extensive quality controls on their final product. It’s an expensive process, but you are worth it.
I wish I could tell you that all companies cared enough about your health to produce products that are pure and potent. Unfortunately, I cannot.
Some products don’t contain the amount of active ingredient claimed on the label. Some products contain potentially toxic contaminants. These errors are usually due to poor manufacturing processes and/or lack of proper quality controls.
Even worse, some products are adulterated. That means the manufacturer substituted a cheaper ingredient for the active ingredient. That cannot be accidental. Adulteration is a willful act to deceive the consumer.
I also wish I could tell you the USDA and the FDA are protecting you by making sure food and supplement products are pure and potent. Unfortunately, I cannot.
It’s not that they aren’t trying. They are simply overwhelmed.
- There are hundreds of charlatans in the marketplace.
- And, as soon as they put one out of business, another one pops up. It’s like that “Whack A Mole” game at the county fair.
Normally, I see reports of poor quality products every few months. But when five product horror stories crossed my desk in a few weeks, it is time to speak up. This week I will share reports on quality control and adulteration issues with:
- Turmeric supplements.
- Lavender essential oils.
- Bitter orange supplements.
- Avocado oil.
- CBD products.
Adulteration Of Turmeric Supplements
 Turmeric supplements are “hot” right now. Their sales have almost doubled in the last couple of years. Whenever a product becomes this popular, unscrupulous manufacturers are tempted to jump into the market. Looking to make a quick buck they substitute inactive, less expensive ingredients for the active ingredients – a process called “adulteration”.
Turmeric supplements are “hot” right now. Their sales have almost doubled in the last couple of years. Whenever a product becomes this popular, unscrupulous manufacturers are tempted to jump into the market. Looking to make a quick buck they substitute inactive, less expensive ingredients for the active ingredients – a process called “adulteration”.
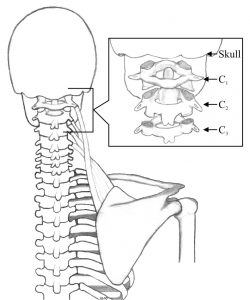
To better understand how turmeric supplements are adulterated, let’s look at how turmeric supplements are made. The active ingredients in turmeric supplements are a class of compounds called curcuminoids that come from the root of the Curcuma longa plant.
1) The simplest way to create a turmeric supplement is to simply grind the root into a powder and put the resulting turmeric powder into a capsule or tablet.
-
- However, turmeric powder is often adulterated by substituting the less expensive Curcuma zeodoria root (from wild turmeric) for the Curcuma longa
2) The more potent turmeric supplements extract the active curcuminoids from turmeric powder.
-
- However, turmeric extracts are often adulterated by substituting synthetic curcumin for the natural extract.
Fortunately, the American Botanical Council has created a program called Botanical Adulterants Prevention Program (BAPP) to identify bad players in the botanicals (meaning anything coming from plants) market. In a recent bulletin on turmeric adulteration, they reported:
- In one test of turmeric powder, all the samples tested had more Curcuma zeodoria powder than Curcuma longa
- In another test of turmeric powder, 4 out of 6 samples were adulterated with Curcuma zeodoria
- In a test of turmeric extracts, 4 out of 5 samples were adulterated with synthetic curcumin.
Is Curcuma zeodoria powder as safe and effective as Curcuma longa powder? Nobody knows.
- Curcuma zeodoria root has a different mix of curcuminoids than Curcuma longa root, and some concerns have been raised about the safety of Curcuma zeodoria
Is synthetic curcumin as safe and effective as natural turmeric extract? Nobody knows.
- The FDA views synthetic versions of natural botanical compounds as different from the botanical itself, Thus, if a supplier correctly identified their extract as containing synthetic curcumin, they would be required to file an NDI notification with FDA, including proof of safety, for products containing their extract to be legally sold in the US.
- The use of synthetic curcumin may replace the other curcuminoids found in natural turmeric extracts. In other words, you would not be getting the full spectrum of curcuminoids you would find in a natural extract standardized to 95% curcuminoids.
Note: The American Botanical Council Bulletin did not address turmeric products that are available on the marketplace. They reported on the major suppliers of the raw materials that manufacturers purchase to make their turmeric products. This has two important implications for consumers like you and me:
- Many companies base their label claims on the specifications provided by the supplier of their raw ingredients. However, unless they run independent quality control tests on the raw ingredients, they actually have no idea what is in their product.
- That means when comparing turmeric products, we should not rely on label claims or price alone. We should ask about the company’s quality control process, particularly whether they run independent quality control tests on the ingredients they use.
Adulteration Of Lavender Essential Oil
 Lavender oil has been around for hundreds of years. It has long been prized for its calming effect. It has traditionally been used in aromatherapy for relief of stress, anxiety, depression, and to improve sleep.
Lavender oil has been around for hundreds of years. It has long been prized for its calming effect. It has traditionally been used in aromatherapy for relief of stress, anxiety, depression, and to improve sleep.
With the recent “essential oil” craze, it has been reclassified as an essential oil with an impressive list of additional “benefits” – such as relieving headaches, getting rid of acne and eczema, reducing menstrual cramps, and reducing inflammation to name a few.
As you might expect, the market for lavender essential oil is exploding. It is expected to almost double between 2016 and 2024.
However, lavender oil is hard to come by. The lavender flowers are steamed to release the volatile components, and the oil is then distilled. Only a tiny fraction of the lavender plant ends up in the final product. You might suspect that manufacturers would be tempted to cut corners. You would be correct.
Once again, the American Botanical Council’s Botanical Adulterants Prevention Program (BAPP) comes to the rescue. Recently BAPP tested lavender essential oils in the marketplace. Their newly-released bulletin reported that 82% of lavender products on the market were adulterated.
- Some of the adulterated products used oils from related plant species.
- Some products used oils from unrelated plant species like rosemary.
- Other products used synthetic oils.
All the adulterated products used oils that were less expensive than genuine lavender oil. To the untrained consumer the adulterated products may smell like lavender oil, but there is no evidence that the oils substituted for lavender oil have the same benefits as lavender oil.
This is not simply a quality control issue. It was not accidental. You don’t start with plant species other than lavender and expect to end up with lavender oil. And you really don’t start with synthetic oils and expect to end up with natural lavender oil. This is deception, pure and simple.
Poor Quality Control Of Bitter Orange Supplements
 Bitter orange is another name for the Seville Oranges you may have seen in your local market. Unripe Seville Oranges are quite bitter, and this is the form used in supplements.
Bitter orange is another name for the Seville Oranges you may have seen in your local market. Unripe Seville Oranges are quite bitter, and this is the form used in supplements.
Traditionally, bitter oranges have been used as a digestive aide. More recently, some unscrupulous manufacturers have advertised bitter orange as a fat burning supplement and have marketed it as a sports nutrition and weight management supplement.
Any supplement marketed as “fat burning” attracts a lot of attention. Once again, sales have skyrocketed, and manufacturers have been tempted to cut corners. This attracted the attention of the USDA, who recently published a study assessing the quality of supplements containing bitter orange.
The USDA purchased 59 products available in the US that either contained bitter orange as the primary ingredient or as one of the major ingredients in a proprietary formula. They tested these products using state-of-the-art analytical techniques. What they found wasn’t pretty.
- Only 5 of the products had the amount of active ingredient claimed on the label. This could be a quality control issue, but it is not reassuring to you, the consumer.
- Some of the products had higher amounts of minor compounds found in the bitter orange than they did of the active ingredient. It is hard to imagine how this occurred unless those manufacturers used what was left over after other companies had extracted the active ingredient. And there is no research on the effects of these minor compounds in humans.
- 7 of the products had synthetic ingredients that had never seen a bitter orange. Once again, there is no evidence these compounds are either safe or effective.
Poor Quality & Adulterated Avocado Oil

Avocados are in. They are prized as a source of antioxidants and healthy monounsaturated fats. Avocado oil has all the benefits of raw avocados, plus it has an extremely high smoke point, making it ideal for high temperature cooking.
It’s no wonder that sales of avocado oil have soared by 52% in the last couple of years alone. Once again, there will be manufacturers who are tempted to cut corners.
Fortunately, scientist at University of California, Davis recently published a study on the quality of avocado oil. Unfortunately, they found that most of the avocado oil sold in the US was oxidized, mislabeled, or misbranded.
The scientists purchased 14 brands of avocado oil from local markets and purchased an additional 8 brands online. Here is what they found:
- 82% of the 22 brands they tested were either oxidized or mixed with other oils. Specifically:
-
- 15 of the brands were oxidized, which compromises both the taste and the health benefits of avocado oil.
-
- 6 of the brands were adulterated with cheaper oils, including sunflower, safflower, and soybean oil.
-
- 3 of the brands contained little or no avocado oil. They were mixtures of other oils. This is even worse than simple adulteration. These products should not have even been labeled as avocado oil.
-
-
- Interestingly, 2 of the 3 brands with no avocado oil were labeled “extra virgin” avocado oil, which is supposed to indicate the highest quality oil. Did I mention “buyer beware”?
-
CBD Horror Stories
 I don’t need to tell you that the CBD industry has taken off in recent years. Most of the claims for CBD products are unproven, but that is another story for another time.
I don’t need to tell you that the CBD industry has taken off in recent years. Most of the claims for CBD products are unproven, but that is another story for another time.
Even more worrisome are quality control issues for CBD products. In fact, it is so worrisome that congress asked the FDA to study quality controls in the CBD industry and report back to them, which they did last month.
Let me start with a little history. Congress has asked the FDA to set safety, efficacy (product claims), and quality standards for CBD products.
1) The FDA is farthest along with product claims. They have rejected most product claims for CBD products and have initiated legal actions against several companies that have refused to stop making these product claims.
2) With respect to safety they have specified that CBD products should contain less than 0.3% THC (marihuana) but have not yet completed safety studies on other CBD ingredients.
3) With respect to quality controls, they have started by surveying the quality of CBD products currently available in the US. They tested 147 products, and the results weren’t pretty. As described in their report to congress:
-
- 9 CBD products contained no CBD.
-
- 18 products were less potent than advertised. They contained less than 80% of the amount claimed on the label.
-
- 38 products were more potent than advertised. They contained more than 120% of the amount claimed on the label.
-
- 72 products (49% of the total) contained impermissible levels of THC.
How Can You Identify High Quality Products?
As I said in my book “Slaying The Supplement Myths” there are ethical supplement companies that care  about your wellbeing and produce high quality products. However, there is also a dark underbelly of the food and supplement industries.
about your wellbeing and produce high quality products. However, there is also a dark underbelly of the food and supplement industries.
In the article above I have shared examples of products that:
- Contained little or no active ingredient.
- Contain less or more of the active ingredient than claimed on the label.
- Contain potentially harmful contaminants.
- Are adulterated by substituting cheaper ingredients which may not be effective for the active ingredient.
At this point you are probably asking, “How do I protect myself? How do I make sure that I am not wasting my money and jeopardizing my health when I buy a supplement? I cover the answer to this question in my book, “Slaying The Supplement Myths“. Here is a  shortened version:
shortened version:
- Ignore the slick marketing.
- Don’t base your decision on price alone. That can be a trap.
- Do your research. Ask questions. Only choose reputable companies that do quality
controls on both the raw ingredients and the finished product.
The problem, of course, is that every company claims to run stringent quality control tests. My 
suggestion is to ask them about their quality control process. Here are the questions to ask (you will find more in my book):
1) Do you run tests to confirm the purity of your raw ingredients, or do you accept the claims of your suppliers?
2) How many quality control tests do you run on your final product? If it is a single nutrient product, the number should be in the dozens. If it is a multivitamin, the number should be in the hundreds. For more complex products, you should expect a thousand or more quality control tests.
3) Do you run quality controls on every batch…or, put another way…How many quality controls do you run each year? Those should run into the tens of thousands.
4) What kind of analytic methods do you use?
These are tough questions, but they are the right questions to ask before you pick a supplement company. After all, you are entrusting your health to their products.
The Bottom Line
There are ethical food and supplement companies that care about your wellbeing and produce high quality products. However, there is also a dark underbelly of both the food and supplement industries.
In the article above I have shared examples of products that:
- Contained little or no active ingredient.
- Contain less or more of the active ingredient than claimed on the label.
- Contain potentially harmful contaminants.
- Are adulterated by substituting cheaper, less effective ingredients for the active ingredient.
I shared reports of quality control and adulteration horror stories with:
- Turmeric supplements.
- Lavender essential oils.
- Bitter orange supplements.
- Avocado oil.
- CBD products.
I also shared how to find companies that make high quality products you can trust.
For more details, read the article above.
To find which supplements I recommend, click here.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.