Are Starchy Foods Bad For Us?
Author: Dr. Stephen Chaney
 The Paleo Diet is still very popular. And it does have its good points. It is a whole food diet. It eliminates sodas, junk foods, and highly processed foods. Any diet that does that can’t be all bad.
The Paleo Diet is still very popular. And it does have its good points. It is a whole food diet. It eliminates sodas, junk foods, and highly processed foods. Any diet that does that can’t be all bad.
But is it unnecessarily restrictive? It eliminates starchy foods like grains, beans, peas, and corn. It is true that widespread consumption of these foods did not occur until after the agricultural revolution some 12,000 years ago. Our paleolithic ancestors probably did not consume significant quantities of these foods.
But did they consume other starchy foods? Our ideas about this have come primarily from comparing the diets of modern man with the diets of the few primitive hunter-gatherer populations that currently exist in our world. Based on that comparison, some Paleo advocates have concluded that the paleolithic diet contained few, if any, starchy foods.
More importantly, some Paleo advocates have gone a step further to assert that our bodies are not designed to eat starchy foods. They claim that foods like grains, legumes, corn, and potatoes are bad for us. They should be avoided.
How can we test whether these claims are true? After all, we don’t have any way of directly determining whether our paleolithic ancestors ate starchy foods or not. Or do we? That question is the topic of a new study (JA Fellows et al, PNAS, 118 No. 20 e2021655118 I will share with you today.
But first I need to acquaint you with what starch is and how we digest it. Once again, it is time for Biochemistry 101.
Biochemistry 101
 Starch is simply a long polymer of glucose molecules. Digestion of starch starts in our mouth. Our saliva contains an enzyme called alpha-amylase that breaks the bond between adjacent glucose molecules. Alpha-amylase breaks starch down sequentially, first to maltodextrin (a shorter polymer of glucose molecules), then to maltose (two glucose molecules), and finally to glucose.
Starch is simply a long polymer of glucose molecules. Digestion of starch starts in our mouth. Our saliva contains an enzyme called alpha-amylase that breaks the bond between adjacent glucose molecules. Alpha-amylase breaks starch down sequentially, first to maltodextrin (a shorter polymer of glucose molecules), then to maltose (two glucose molecules), and finally to glucose.
[Note: The nutrition gurus that tell you to read labels and avoid foods with maltodextrin are ignoring the fact that we produce maltodextrin naturally whenever we digest starch in the foods we eat.]
All humans contain the alpha-amylase gene. Simply put, that means that all humans have the potential to digest starchy foods.
However, not all humans have the same number of copies of the alpha-amylase gene. When we habitually consume a diet containing starchy foods, our bodies duplicate the alpha-amylase gene until our saliva contains enough alpha-amylase to easily digest the amount of starchy foods we are consuming. Simply put, that means our bodies are designed to easily adapt to the amount of starchy foods in our diet.
Most modern human populations have between six and 30 copies of the alpha-amylase gene. Our saliva contains a lot of alpha-amylase. However, the few primitive hunter-gatherer societies that still exist in our world have only two or three copies of the alpha-amylase gene. Their saliva contains very little alpha-amylase.
It is this difference that has led to the hypothesis that our paleolithic ancestors did not possess salivary alpha-amylase, which implies they didn’t eat starchy foods. This hypothesis also assumes that humans only began producing significant quantities of salivary alpha-amylase after the agricultural revolution when starchy foods like grains, rice, and beans became widely available.
This hypothesis is one of the central tenets of the Paleo diet. But we need to remember that it is just a hypothesis. It has not been directly tested because we thought there was no way to determine the starch content of the paleolithic diet – until now. However, before we get to the study that explodes this hypothesis, I want to revisit the Paleo Diet myths I described in an earlier issue of “Health Tips From The Professor”. I call this next section “Unicorns And The Paleo Diet”.
Unicorns And the Paleo Diet
 I titled this section “Unicorns and the Paleo Diet” because both are myths. In fact, the Paleo Diet is based on several myths.
I titled this section “Unicorns and the Paleo Diet” because both are myths. In fact, the Paleo Diet is based on several myths.
Myth #1: Our ancestors all had the same diet. What we currently know as the Paleo diet is based on the diets of a few primitive hunter-gatherer societies that still exist in some regions of the world. However, when you look at the data more carefully, you discover that the diet of primitive societies varies with their local ecosystems.
The “Paleo diet” is typical of ecosystems in which game is plentiful and fruits and vegetables are less abundant or are seasonal. In ecosystems where fruits and vegetables are abundant, primitive societies tend to be more gatherers than hunters. They eat more fruits and vegetables and less meat.
The assumption that starchy foods were absent in the paleolithic diet is also a myth. For some primitive societies, starchy fruits or starchy roots are a big part of their diet. In short, our paleolithic ancestors ate whatever nature provided.
Myth #2: Our genetic makeup is hardwired around the “paleolithic diet”. In fact, humans are very adaptable. We are omnivores, which means we can eat whatever nature provides. We are designed to thrive in a wide variety of ecosystems. It is this adaptability that has allowed us to expand to every nook and cranny of the world.
For example, the enzymes needed to digest grains are all inducible, which means the body can turn them on when needed. Our paleolithic ancestors may not have eaten much grain, but we can very quickly adapt to the introduction of grains into our diet. As I described above, for alpha-amylase this adaptation occurs through gene duplication.
Myth #3: Our paleolithic ancestors were healthier than modern man: It some respects, the paleolithic diet is healthy, as I mentioned above. However, we need to remember that our paleolithic ancestors rarely lived past 30 or 40. They simply did not live long enough to experience degenerative diseases like heart disease and cancer. We have no idea whether a diet that served our paleolithic ancestors well will keep us healthy into our 70s, 80s and beyond.
How Was This Study Done?
 This is a fascinating study, and one that would have been impossible just a few years ago. As I have described in previous issues of “Health Tips From the Professor”, studies on our microbiome, the bacteria that inhabit our bodies, is a rapidly evolving area of research.
This is a fascinating study, and one that would have been impossible just a few years ago. As I have described in previous issues of “Health Tips From the Professor”, studies on our microbiome, the bacteria that inhabit our bodies, is a rapidly evolving area of research.
When we talk about our microbiome, we generally think about our gut bacteria. However, the term “microbiome” includes all the bacteria that reside in our body, including those that reside in our oral mouth.
And, like our gut bacteria, the species of bacteria that reside in our mouth are heavily dependent on the foods we eat. Specifically, there are three species of oral bacteria that thrive on starch. They possess an “amylase binding protein” that allows them to capture salivary alpha-amylase and use it to break down dietary starch so they can use it as an energy source.
Consequently, the abundance of these three bacterial species in the oral microbiome is a precise marker for the amount of starch in a person’s diet. More importantly, high throughput DNA sequencing and supercomputers have made it simple to sequence all the bacteria in the oral microbiome and quantify the relative abundance of these three bacterial species.
You are probably thinking, “That’s fine, but how could you possibly determine the abundance of those bacteria in the mouth of a paleolithic human?” Here is where it gets really interesting!
The bacteria in our mouth form biofilms on our teeth, something we refer to as plaque. If the plaque remains on our teeth long enough, it calcifies, forming what is referred to as dental calculus (tooth tartar).
In the modern world we remove dental biofilms by brushing after every meal. We remove dental plaque and tartar by semi-annual visits to the dentist. But these are recent developments. They are not something our ancestors did.
Our ancestors simply accumulated dental calculus during their lifetime. More importantly, the dental calculus excluded air and water, so it preserved the DNA of the bacteria in their oral microbiome. That was the basis of the current study.
The study was a collaboration of 50 scientists over a 7-year period. The scientists sequenced 124 oral microbiomes from humanoid species in Africa, including Neanderthals (430,000 to 40,000 years ago), Late Pleistocene (129,000 to 11,700 years ago) humans, and modern-day humans.
Bacterial DNA from modern-day humans was obtained from dental calculus obtained during routine dental cleaning procedures by practicing dentists. The older DNA samples were obtained from dental calculus in the teeth of skeletal remains. The oldest DNA sample was obtained from a Neanderthal that lived around 100,000 years ago.
For comparison they also obtained bacterial DNA from the dental calculus of chimpanzees and gorillas, man’s closest primate relatives.
The species of bacteria in the oral microbiome from all these samples were determined by high throughput sequences and computerized analysis using high speed supercomputers.
Is The Paleo Diet Based On A Myth?
 There were three important findings from this analysis:
There were three important findings from this analysis:
- The species of bacteria in the oral microbiome of Neanderthals and Late Pleistocene humans was much more diverse than for modern humans. This suggests that their diets were more diverse (perhaps depending on what foods were available in their environment), while modern diets have become more standardized.
2) The species of bacteria that thrive on starchy foods were remarkably constant in the oral microbiome of all human species from Neanderthals to Late Pleistocene humans to modern-day humans.
3) The species of bacteria that thrive on starchy foods were virtually absent from the oral microbiomes of our most closely related primates – chimpanzees and gorillas.
The authors concluded, “This … supports an early importance of starch-rich foods in Homo evolution.”
In other words, our paleolithic ancestors likely did eat starchy foods. Their diet may not have contained grains, rice, or beans in significant quantities. However, they consumed whatever starchy roots, fruits, and vegetables they could find.
So, is the Paleo diet based on a myth? It depends on how you phrase the question.
- If we ask whether our paleolithic ancestors consumed grains, rice, or beans, the answer is probably, “No”. The introduction of these foods in significant quantities probably depended on the agricultural revolution that occurred thousands of years later.
- If we ask whether our paleolithic ancestors consumed starchy foods, the answer is probably, “Yes”. The foundation of the Paleo diet was based on a myth. Their oral microbiome contained bacterial species that thrived on starchy foods. In fact, starchy foods may have been an important staple in their diet because they are more calorie dense than other fruits and vegetables.
- If we ask whether our paleolithic ancestors were capable of thriving on a diet that included grains, rice, and beans, the answer is also probably, “Yes”. The oral bacterial species that thrive on starchy foods do so by utilizing the alpha-amylase in human saliva. This means our paleolithic ancestors likely had enough alpha-amylase in their saliva to digest and to thrive on starchy foods like grains, rice, and beans.
Are Starchy Foods Bad For Us?
 It is not just the Paleo diet. Many popular diets have villainized starchy foods. Are starchy foods as bad for us as some “experts” would have you believe?
It is not just the Paleo diet. Many popular diets have villainized starchy foods. Are starchy foods as bad for us as some “experts” would have you believe?
Let’s start by identifying starchy foods. If we think in terms of whole foods, they are:
- Root vegetables (for example, potatoes, sweet potatoes, beets, carrots, and parsnips).
- Legumes (for example, beans, peas, and lentils).
- Grains (for example, wheat, rye, barley, oats, and rice).
- Winter squash (for example, acorn squash, butternut squash, hubbard squash, and pumpkin).
These foods are good sources of nutrients and phytonutrients. Many of them are also excellent sources of fiber, including a special type of fiber called resistant starch. (I have described the benefits of resistant starch in a previous issue of “Health Tips From the Professor”.) These are foods that definitely deserve to be part of a healthy diet.
The only drawback of starchy vegetables is that they tend to be more calorie dense than other vegetables. While this was a “plus” for our paleolithic ancestors, it is not quite as advantageous in our modern world. If you are trying to watch your calories, my advice is to incorporate these foods into your diet sparingly.
However, there is another class of starchy foods you want to avoid. Of course, I am talking about highly processed foods made from grains, legumes, and corn. They retain all the calories but lose most of the nutrients, phytonutrients, and fiber of the foods they came from.
In short, starchy whole foods are a valuable part of a healthy diet. It is the starchy processed foods made from these whole foods you want to avoid. Of course, I am talking about bread, pasta, and pastries made from refined grains and sugar.
So, how do you know which starchy foods to avoid? My advice is not to become an expert label reader. Just eat foods without labels.
The Bottom Line
One of the founding principles on which the Paleo diet is based is that our paleolithic ancestors ate very few starchy foods, and the human body really isn’t designed to handle these foods. Accordingly, the Paleo diet recommends we should avoid starchy foods like grains and legumes. This has the unfortunate effect of creating an unbalanced diet that overemphasizes meat and animal fats.
But is this founding principle correct, or is it just a myth? When you look beneath the surface, you discover that it is a hypothesis based on the diets of the few primitive hunter-gatherer populations that still exist in our world.
It has been assumed that was as good an estimate of the paleolithic diet as we could get. After all there was no way to directly determine the starch content of the paleolithic diet – until now.
In this issue of “Health Tips From the Professor” I describe a novel approach that allowed scientists to determine the species of bacteria residing in the mouth of our humanoid ancestors based on the DNA extracted from the plaque coating their teeth. (For details on how this was done, read the article above.)
What the scientists found was that all human species, including a Neanderthal who died 100,000 years ago, harbored bacteria in their mouths that thrive on starchy foods.
The scientists concluded, “This … supports an early importance of starch-rich foods in Homo evolution.” In other words, our paleolithic ancestors likely did eat starchy foods. Restricting whole grains and legumes from the Paleo diet is based on a myth. They are an important part of a healthy diet.
For more details about the study and which starchy foods are bad for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
 Things are hot here in Sarasota – today the temperature was 95 degrees in the sun. Fortunately, my office is in the shade. On the plus side it rained, and my garden was dancing with delight.
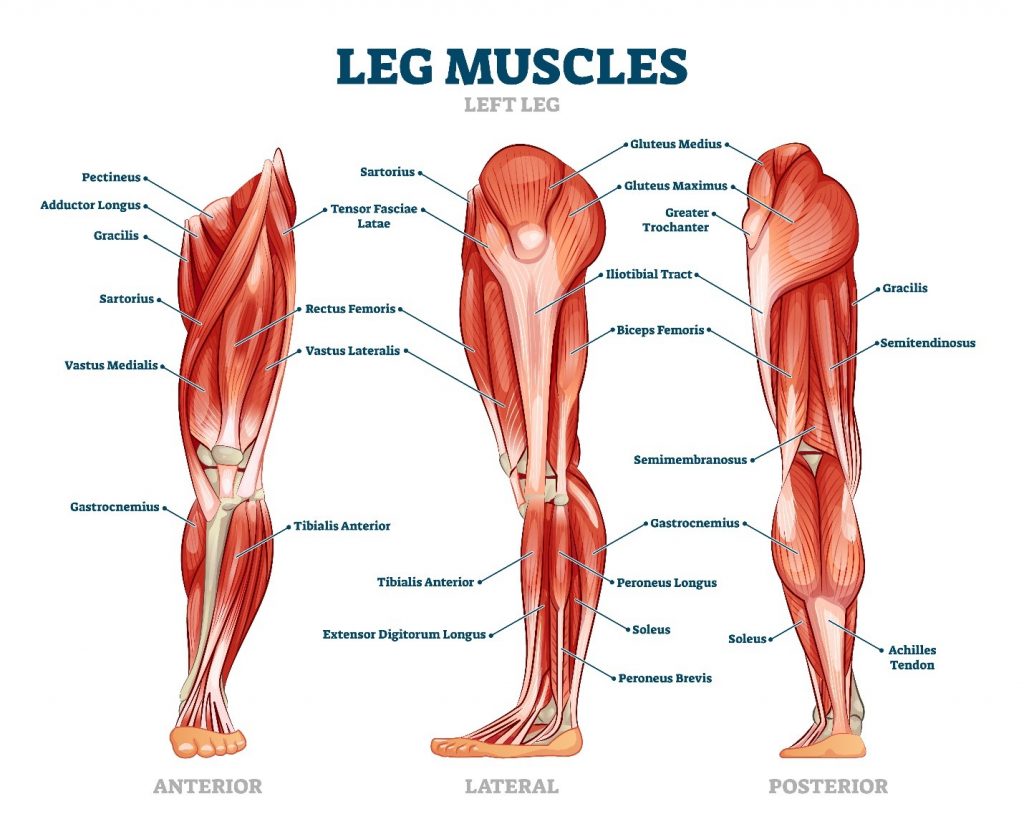
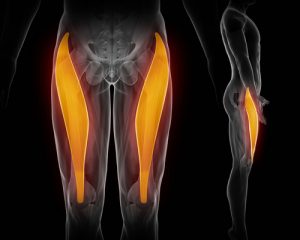
Things are hot here in Sarasota – today the temperature was 95 degrees in the sun. Fortunately, my office is in the shade. On the plus side it rained, and my garden was dancing with delight. My client was actually in to see me for a totally different condition, but while I was working on her I noticed that her left foot was turned in.
My client was actually in to see me for a totally different condition, but while I was working on her I noticed that her left foot was turned in. The self-treatment for these muscles is easy, but it can be painful at about the point where you see the ball in the picture to the left, and again closer to the bottom of your ankle.
The self-treatment for these muscles is easy, but it can be painful at about the point where you see the ball in the picture to the left, and again closer to the bottom of your ankle.
 I treated all the muscles of the lower leg, paying special attention to the two muscles mentioned. I’m happy to say that when I finished and she stood up, her feet were almost straight. With more self-treatment every day, her foot will straighten out.
I treated all the muscles of the lower leg, paying special attention to the two muscles mentioned. I’m happy to say that when I finished and she stood up, her feet were almost straight. With more self-treatment every day, her foot will straighten out.