The Scientific Method In Action
Author: Dr. Stephen Chaney
 You have probably heard that low alcohol consumption is healthier than complete abstinence from alcohol. It is certainly a popular viewpoint.
You have probably heard that low alcohol consumption is healthier than complete abstinence from alcohol. It is certainly a popular viewpoint.
It is also a scientific paradigm. By that I mean:
- It is supported by multiple clinical studies.
- Elaborate metabolic explanations have been proposed to support this paradigm.
- It is the official position of most medical societies, scientific organizations, and health information sites on the web.
- It is the recommendation of most health professionals.
- It has been repeated so often from so many trusted sources that everyone assumes it must be true.
So, you may have been surprised when you saw recent headlines saying, “Having an alcoholic drink or two per day is not healthier than abstaining.”
Today I will review the study (J Zhao et al, JAMA Network Open, 6(3): e236185, 2023) behind the headlines and tell you what it means for you.
But first, I want to explain to you how the scientific method works. That’s because this study is a perfect example of the scientific method in action.
The Scientific Method In Action
 I have described the scientific method in detail in my books “Slaying The Food Myths” and “Slaying The Supplement Myths”, which you will find here.
I have described the scientific method in detail in my books “Slaying The Food Myths” and “Slaying The Supplement Myths”, which you will find here.
Today, I will just give you a brief synopsis of the scientific method.
- Most scientific studies are designed to disprove existing scientific paradigms.
-
- In the scientific world, there is no glory in being the 10th person to prove that a scientific paradigm is correct. The glory comes from being the first person to disprove a scientific paradigm and create a new paradigm in the process.
-
- This constant testing of existing paradigms is one of the most important strengths of the scientific method.
2) There is no perfect study. Every study has its flaws.
-
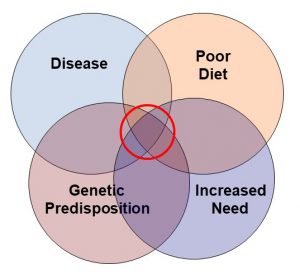
- “Confounding variables” are flaws that can be the Achilles Heel of any association study.
Now let me explain the significance of these statements in the context of the current study:
-
- All the studies supporting the current study were association studies. Association studies measure the association between a selected variable and an outcome. For these studies, the selected variable was alcohol consumption, and the outcome was increased mortality.
-
-
- Association studies try to statistically correct for other variables known to affect the outcome. For example, diseases like heart disease, diabetes, and cancer increase the risk of premature death. These are known variables that would be corrected for in any well-designed study of alcohol consumption and mortality.
-
-
-
- “Confounding variables” are unknown variables that also affect the outcome of the study. But since they are unknown, they are not corrected for.
-
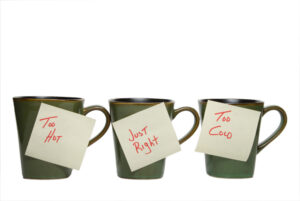
Let me give you a simplistic example of a confounding variable. Let’s say you were doing a study of dietary habits and you found an association between ice cream consumption and mortality. You might conclude that ice cream consumption is bad for you. It increases your risk of dying.
But then you might remember that ice cream consumption increases during the summer. And then you might reason that people swim more during the summer, and there is a correlation between swimming and drowning deaths.
Swimming could be a confounding variable. To make sure that your initial conclusion that ice cream increases the risk of dying was correct, you would need to correct your data for swimming deaths during the summer and see if you still found a correlation between ice cream consumption and mortality.
Could The Current Paradigm Be Incorrect?
 You might be thinking, “What does this have to do with studies on the correlation between alcohol consumption and increased mortality?” Let me explain.
You might be thinking, “What does this have to do with studies on the correlation between alcohol consumption and increased mortality?” Let me explain.
The baseline group for these comparisons was the abstainers – the group consuming no alcohol. Previous studies have compared the mortality risk associated with various amounts of alcohol consumption with the mortality risk of the abstainer group. This sounds like a reasonable approach.
But the investigators challenging the current paradigm noted that the “abstainer group” in previous studies included both lifetime abstainers and former drinkers who had become abstainers. They hypothesized that the “former drinkers” group may have become abstainers because of health issues related to excess alcohol consumption.
In short, they hypothesized that the “former drinkers” group was a confounding variable that biased the results of the previous studies. They hypothesized that the “lifetime abstainers” group was a more appropriate baseline group for this kind of study. They then set out to prove their hypothesis.
How Was This Study Done?
 The investigators searched the literature and found 107 studies with 4.8 million participants published between 1980 and July 21, 2021, that:
The investigators searched the literature and found 107 studies with 4.8 million participants published between 1980 and July 21, 2021, that:
- Assessed the correlation between alcohol consumption and mortality.
- Had data that allowed the investigators to separate lifetime abstainers from former drinkers who had become abstainers.
The investigators divided alcohol consumption into low, moderate, high, and very high categories based on the ounces of alcohol consumed per day. Since ounces of alcohol is not an easy measure for most of us, I have converted ounces/day to drinks/day based on the CDC definition of a drink (a 12-ounce beer, 5-ounce glass of wine, or 1.5 ounces of a distilled spirit like gin or vodka). And to make it even simpler, I have rounded to the nearest whole number. With that said, here are the classifications.
- Low alcohol intake = 1-2 drinks/day.
- Moderate alcohol intake = 2-3 drinks/day.
- High alcohol intake = 3-4 drinks/day.
- Very high alcohol intake = >4 drinks/day.
The risk of death associated with each of these intake levels was compared the risk of death of their preferred baseline group, the “lifetime abstainers”.
Finally, the data were corrected for other variables known to influence the correlation between alcohol consumption and mortality, namely age, sex, heart health, social status, race, diet, exercise, BMI, and smoking status. [These are known variables and had been adjusted for in most previous studies.]
Is Low Alcohol Consumption Healthy?
 When the investigators compared the mortality risk of former drinkers who had become abstainers with lifetime abstainers:
When the investigators compared the mortality risk of former drinkers who had become abstainers with lifetime abstainers:
- The former drinkers were 31% more likely to die, and this difference was highly significant.
- This is consistent with their hypothesis that the “former drinkers” group was a confounding variable that may have biased the conclusions of previous studies.
When they compared the mortality risk of various levels of alcohol consumption with lifetime abstainers instead of all abstainers, they found:
- The risk of mortality associated with low (1-2 drinks/day) and moderate (2-3 drinks/day) alcohol intake was statistically identical to the risk of mortality for lifetime abstainers.
- The high alcohol intake group (3-4 drinks/day) was 24% more likely to die than the lifetime abstainers.
- The very high alcohol intake group (>4 drinks/day) was 39% more likely to die than the lifetime abstainers.
In short, when lifetime abstainers were used as the baseline group, low to moderate alcohol intake did not reduce the risk of dying, as previous studies had suggested. This study disproves the existing paradigm.
Finally, there was a significant gender difference in the effect of alcohol consumption on mortality. For women:
- Even moderate alcohol consumption was associated with an increased risk of mortality.
- The increased risk of mortality for women was significantly higher than for men with every level of alcohol consumption.
The authors concluded, “In this…meta-analysis, daily low or moderate alcohol intake was not significantly associated with all-cause mortality risk, while increased risk was evident at higher consumption levels, starting at lower levels for women than for men.”
Of course, this isn’t the end of the story. The scientific method will continue. Old paradigms don’t die easily. Other investigators will challenge the conclusions of this study. Stay tuned. I will give you updates as future studies are published.
What Does This Study Mean For You?
 If you like to imbibe, there are two important takeaways from this study.
If you like to imbibe, there are two important takeaways from this study.
The bad news is that you can no longer claim that a drink or two a day is healthier than total abstinence from alcohol.
The good news is that this and every study preceding it have found that a drink or two a day is no less healthy than total abstinence. The studies found no increase in mortality associated with low to moderate alcohol intake.
[However, low to moderate alcohol intake may increase your risk of specific diseases. For example, many studies suggest that even low alcohol intake is associated with an increased risk of breast cancer.]
This study also agrees with previous studies that high alcohol intake increases your risk of death, and women are more susceptible to adverse effects of alcohol intake than men.
So, while this study challenges the existing paradigm that low to moderate alcohol intake is beneficial, it does not change the current recommendations on alcohol intake by most health organizations.
For example, the current CDC guidelines are:
- Adults of legal drinking age should limit alcohol intake to 2 drinks or less per day for men and one drink or less per day for women.
- Adults who do not drink alcohol should not start. [The current study strengthens this recommendation because it takes away the excuse that low to moderate alcohol consumption is healthier than abstinence.]
- Drinking less is better than drinking more.
The CDC guidelines also note that the risk of some cancers increases even at very low levels of alcohol consumption.
Finally, the CDC recommends that some people never consume alcohol, including:
- Women who are pregnant or might become pregnant.
- Anyone younger than 21.
- Anyone with medical conditions or medications that interact with alcohol.
- Anyone recovering from an alcohol use disorder or who has trouble controlling the amount they drink.
The Bottom Line
A recent study is a perfect example of the scientific method in action. Scientists are constantly challenging the existing scientific paradigms, and this is an important strength of the scientific method.
A group of scientists recently published a study challenging the paradigm that low to moderate alcohol intake is healthier than total abstinence from alcohol.
They hypothesized that previous studies supporting this paradigm had a common methodological flaw, corrected for the flaw, and reanalyzed the data from 104 studies with a total of 4.8 million participants.
The revised data showed no health benefit of low to moderate alcohol consumption compared to total abstinence.
- This is a major change to the existing paradigm because it removes the justification for low to moderate alcohol consumption.
However, the revised data did not differ from previous studies in the following ways:
- There is no health risk associated with low to moderate alcohol intake compared to total abstinence.
- High alcohol intake (>3 drinks/day) is associated with increased mortality.
- Women are more sensitive to the adverse effects of alcohol than men.
So, this study does not change current guidelines for alcohol consumption.
For more information on this study, what it means for you, and the CDC guidelines on alcohol consumption read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance